* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download diet
Thrifty gene hypothesis wikipedia , lookup
Food choice wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Oral rehydration therapy wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Selfish brain theory wikipedia , lookup
Chromium(III) picolinate wikipedia , lookup
Human nutrition wikipedia , lookup
Dietary fiber wikipedia , lookup
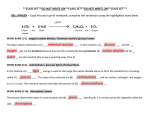
Perspectives in Nutrition, 8th Edition Chapter 5 Outline: Carbohydrates After studying this chapter, you will be able to: 1. Identify the major types of carbohydrates and give examples of food sources for each. 2. List alternative sweeteners that can be used to reduce sugar intake. 3. Describe recommendations for carbohydrate intake and health risks caused by low or excessive intakes. 4. List the functions of carbohydrates in the body. 5. Explain how carbohydrates are digested and absorbed. 6. Identify the cause of, effects of, and dietary treatment for lactose intolerance. 7. Describe the regulation of blood glucose, conditions caused by blood glucose imbalance, types of diabetes, and dietary treatments for diabetes. 8. Describe dietary measures to reduce the risk of developing type 2 diabetes. 5.1 Structures of Carbohydrates A. General 1. Composed of carbon, hydrogen, and oxygen 2. Plants produce glucose by photosynthesis from carbon (air), oxygen (air), hydrogen (water), and energy (sun) 3. General chemical formula is (CH2O)n B. Monosaccharides: Glucose, Fructose, Galactose, Sugar Alcohols, and Pentoses 1. Each monosaccharide contains 6 carbon, 12 hydrogen, and 6 oxygen molecules, but in slightly different configurations (see Figure 5-3) 2. Having 6 carbon molecules classifies these monosaccharides as hexoses 3. Glucose a. Most abundant monosaccharide b. Usually linked with other monosaccharides c. Also called dextrose 4. Fructose a. Found in fruits, vegetables, honey, and high-fructose corn syrup b. HFCS is sweeter and less expensive than sucrose, used in many food products c. Also called levulose 5. Galactose in the diet is usually linked with glucose to form lactose 6. Sugar alcohols are derivatives of monosaccharides; used as sweeteners in gum and dietetic foods a. Sorbitol b. Mannitol c. Xylitol 7. Pentoses: 5 carbon sugars C. D. E. a. Ribose (part of RNA) b. Deoxyribose (part of DNA) Disaccharides: Maltose, Sucrose, and Lactose 1. Contain 2 monosaccharides linked together in a condensation reaction, which forms 1 molecule of water (see Figure 5-4) a. Alpha bonds: found in maltose and sucrose; easily broken down by intestinal enzymes b. Beta bonds: found in lactose and dietary fiber; not easily broken down by intestinal enzymes 2. Maltose a. Glucose + glucose b. Found in malted alcoholic beverages: seeds allowed to sprout c. Formed in small intestine upon digestion of longer-chain polysaccharides 3. Sucrose a. Glucose + fructose b. Found in plants such as sugar cane, sugar beets, maple tree sap c. Brown, white, and powdered sugars are produced from plant sources 4. Lactose a. Glucose + galactose b. Found in milk and milk products c. Lactose intolerance results from insufficient lactase production, leads to intestinal gas, bloating, cramping, discomfort when undigested lactose is metabolized into acids and gases by colonic bacteria 5. Simple sugars include monosaccharides and disaccharides Oligosaccharides: Raffinose and Stachyose 1. Oligosaccharides a. Contain 3 - 10 simple sugar units b. Cannot be digested by human enzymes, metabolized by colonic bacteria, produce intestinal gas c. Enzyme preparation (e.g., Beano) breaks down oligosaccharides before they reach the large intestine 2. Raffinose: indigestible oligosaccharide made of 3 monosaccharides (galactose + glucose + fructose) 3. Stachyose: indigestible oligosaccharide made of 4 monosaccharides (galactose + galactose + glucose + fructose) Polysaccharides: Starch, Glycogen, and Fiber 1. General a. Polysaccharides are complex carbohydrates with many glucose molecules b. Digestibility is determined by type of bonds (alpha or beta) 2. Digestible Polysaccharides: Starch and Glycogen a. Starch i. Major digestible dietary polysaccharide ii. iii. 3. Storage form of glucose in plants Amylose: straight chain of many glucose molecules linked by alpha bonds iv. Amylopectin: branched chain of many glucose molecules linked by alpha bonds; causes more rapid rise in blood glucose than amylose because there are more sites for enzyme action v. Cooking increases digestibility of starches by making them soluble in water vi. Modified food starch is made by amylose molecules bound together; used as thickening agent in foods b. Glycogen i. Storage form of carbohydrate in humans and animals ii. Glucose units linked by alpha bonds iii. More highly branched than amylopectin; broken down quickly iv. Stored in liver and muscle cells, amount is influenced by dietary intake Indigestible Polysaccharides: Dietary and Functional Fiber a. Total fiber: dietary fiber + functional fiber b. Dietary fiber: occurs naturally in foods c. Functional fiber: added to foods, provides health benefits d. Nutrition Facts panel only includes dietary fiber e. Non-starch polysaccharides with beta bonds i. Cellulose ii. Hemicelluloses iii. Pectins iv. Gums v. Mucilages f. Non-carbohydrate component i. Lignins g. Fermented by colonic bacteria to produce short-chain fatty acids and gases (pectins, gums, and mucilages yield ~1.5 - 2.5 kcal/g) h. Body adapts to higher fiber intake - decreased bloating, gas, discomfort i. Insoluble fibers i. Not easily dissolved in water ii. Not easily metabolized by colonic bacteria iii. Decrease intestinal transit time iv. Reduce constipation, diverticular disease, and colon cancer v. Examples: cellulose (skin of fruits and vegetables, legumes, celery, whole grains), hemicelluloses (whole grains, some vegetables), lignins (seeds of fruits, bran layer) j. Soluble fibers (a.k.a. viscous fiber) i. Dissolve in water ii. Metabolized by colonic bacteria iii. iv. v. vi. vii. 5.2 Lower blood cholesterol Delays gastric emptying Lower blood glucose Reduce risk of CVD and diabetes Examples: pectin (fruits), some hemicelluloses (oat bran), gums and mucilages (legumes, seaweed, psyllium) Carbohydrates in Foods A. Starch 1. Legumes 2. Tubers 3. Grains (wheat, rye, corn, oats, barley, rice) used to make breads, cereals, and pasta B. Fiber 1. Whole grains 2. Legumes 3. Tubers 4. Psyllium 5. Seaweed 6. Functional fiber is available as supplement C. Nutritive Sweeteners 1. Can be metabolized to yield energy 2. Monosaccharides (glucose, fructose, galactose) 3. Disaccharides (sucrose, lactose, maltose) 4. Most dietary sucrose has been added during processing; not naturally-occurring 5. High-fructose corn syrup a. Made by treating cornstarch with acid and enzymes to break down starch to glucose; some glucose converted to fructose by enzymes b. Final product is 40 - 90% fructose c. Similar to sucrose in sweetness, but less expensive 6. Sugar Alcohols a. Examples i. Sorbitol ii. Mannitol iii. Xylitol b. Do not promote dental caries because they are not metabolized by bacteria in the mouth c. Do contribute energy (1.5 - 3 kcal/g), but are absorbed and metabolized more slowly than sugars d. May induce diarrhea in large quantities D. Alternative Sweeteners (see Table 5-1) 1. General a. 2. 3. 4. 5. 6. Non-caloric or very-low-calorie sugar substitutes for diabetes or weight loss b. Safety determined by FDA, indicated by Acceptable Daily Intake guideline: amount of a sweetener that an individual can safely consume daily over a lifetime (mg/kg body weight/d) c. ADIs are based on animal studies and set 100 times less than level at which no harmful effects were noted in animal studies d. Considered safe for use by adults and children and during pregnancy Saccharin (Sweet n’ Low) a. 300x sweeter than sucrose b. Early research linking saccharin to bladder cancer has been proven weak and inconclusive c. ADI: 5 mg/kg/d (3 cans of diet soft drinks or 7 packets) d. Not useful in cooking because heating causes bitter taste e. Uses: tabletop sweetener, variety of foods and beverages Aspartame (NutraSweet, Equal) a. Not useful in cooking because it loses its sweetness when heated b. Yields 4 kcal/g c. 180 - 200 x sweeter than sucrose d. ADI: 50 mg/kg/d (14 cans of diet soft drink or 80 packets) e. Some reports of adverse reactions (e.g., headaches, dizziness, seizures, nausea) f. Should be avoided by those with phenylketonuria (PKU) a disease that interferes with phenylalanine metabolism g. Uses: beverages, gelatin desserts, chewing gum, cookies, toppings and fillings of baked goods Neotame a. Heat stable, can be used in cooking and as tabletop sweetener b. 7000 - 13,000 x sweeter than sucrose c. Contains phenylalanine, but is not a problem for individuals with PKU d. ADI: 2 mg/kg/d e. Uses: baked foods, non-alcoholic beverages, chewing gum, confections, frostings, frozen desserts, gelatin, pudding, jams, jellies, processed fruits and fruit juices, toppings, syrups Acesulfame-K (Sunette) a. 200 x sweeter than sucrose b. Not digested, provides no calories c. Heat stable, can be used in baking d. ADI: 15 mg/kg/d e. Uses: chewing gum, powdered drink mixes, gelatins, puddings, baked goods, tabletop sweeteners, candy, throat lozenges, yogurt, non-dairy creamers Sucralose (Splenda) a. b. c. d. e. f. 7. 8. 5.3 600 x sweeter than sucrose Substitutes 3 chlorines for 3 hydroxyl groups on sucrose Not digested, yields no calories Heat stable, used in cooking and baking ADI: 5 mg/kg/d Uses: tabletop sweetener, soft drinks, chewing gum, baked cookies, syrups, gelatins, frozen dairy desserts, jams, processed fruits and fruit juices Tagatose (Naturlose) a. Isomer of fructose b. Almost as sweet as sucrose c. Can be used in cooking and baking d. Poorly absorbed, yields 1.5 kcal/g e. Prebiotic effect f. Should be avoided by those with disorders of fructose metabolism g. Uses: cereals, diet soft drinks, health bars, frozen yogurt, fat-free ice cream, soft and hard confectionary products, frosting, chewing gum Stevia a. 100 - 300 x sweeter than sucrose b. Provides no calories c. FDA has not yet approved its used in foods, but it can be purchased as a dietary supplement Recommended Intake of Carbohydrates A. Recommendations for total carbohydrate intake 1. RDA for adults: 130 g/d of digestible carbohydrate to supply adequate glucose for the brain and central nervous system without having to rely on ketosis 2. Food and Nutrition Board recommends that carbohydrates comprise 45 - 65% of total energy intake 3. Various weight-loss approaches vary considerably from FNB recommendations 4. Carbohydrates should come mainly from fiber-rich fruits, vegetables, and whole grains with little added sugars and caloric sweeteners 5. Ample carbohydrate intake may be achieved by consuming 6 oz grains, 2.5 c vegetables, 2 c fruit, and 3 c milk B. Recommendations for added sugars 1. Dietary Guidelines recommend limiting added sugars to 6% of total energy intake 2. World Health Organization recommends limiting added sugars to 10% to total energy intake (12 tsp or 50 g/d for 2000-kcal diet) 3. Food and Nutrition Board set upper limit of 25% of total energy intake from added sugars (30 tsp or 125 g/d for 2000-kcal diet) C. Recommendations for dietary fiber 1. 14 g/1000 kcal D. 5.4 2. Women: 25 g/d 3. Men: 38 g/d Our Carbohydrate Intake 1. Typical North Americans consume 50% of total energy intake as carbohydrates, mostly from white bread, soft drinks, cookies, cakes, doughnuts, sugars, syrups, jams, potatoes 2. Worldwide carbohydrate intake averages 70- 80% of total energy, mostly from whole grains, fruits, vegetables, and legumes 3. Added sugars supply 16% of total energy intake (mainly due to sweetened beverages) 4. Insufficient fiber intake (25 - 50% lower than recommendations) a. Lack of knowledge about fiber-rich food sources and benefits b. Confusing food labeling (e.g., “wheat” bread is not necessarily made from whole grains Functions of Carbohydrates in the Body A. Digestible Carbohydrates 1. Providing Energy a. Most digestible carbohydrates are broken down to glucose, source of energy for all body cells b. Red blood cells and CNS cells use glucose almost exclusively c. Glucose provides 4 kcal/g 2. Sparing Protein from Use as an Energy Source a. Adequate carbohydrates are required to allow amino acids to be used to build body tissues and perform vital processes b. Gluconeogenesis: synthesis of glucose from amino acids c. Typical American protein intake is high, sparing protein is not a primary concern except for energy-reduced diets and malnutrition 3. Preventing Ketosis a. When carbohydrate intake falls below 50 - 100 g/d, fatty acids are incompletely metabolized for energy, generating ketone bodies b. Brain and CNS can adapt to using ketones for energy when carbohydrates are inadequate c. Excessive ketone production (ketoacidosis) may result from poorly controlled diabetes due to inadequate insulin (or insulin resistance) for cells to use glucose d. Ketosis is promoted by some weight-loss programs because it suppresses appetite and increases water losses, but over time, can lead to dehydration, loss of lean body mass, and electrolyte imbalances B. Indigestible Carbohydrates 1. Promoting Bowel Health a. Fiber adds bulk to feces to ease bowel movements, preventing constipation b. 2. 3. 4. 5.5 Straining during defecation can lead to i. Hemorrhoids ii. Formation of diverticula (diverticulosis), which may become inflamed (diverticulitis) iii. Fiber intake must be limited during episodes of diverticulitis, but high-fiber, high-fluid diet with physical activity is recommended for prevention of future attacks of diverticulitis c. High-fiber diets may reduce risk of colon cancer, likely due to nutrients present in high-fiber foods (e.g., vitamins, minerals, phytochemicals) Reducing Obesity Risk a. Bulk of high-fiber diet limits energy intake, contributes to satiety Enhancing Blood Glucose Control a. Soluble fibers slow glucose absorption from the small intestine and decrease insulin release from the pancreas b. Low-fiber diet increases risk of developing diabetes Reducing Cholesterol Absorption a. High soluble fiber intake inhibits absorption of cholesterol and reabsorption of bile acids from small intestine b. Reduced risk of cardiovascular disease c. Reduced risk of gallstones d. Short-chain fatty acids from bacterial fermentation of soluble fiber in the large intestine reduce cholesterol synthesis in the liver Carbohydrate Digestion and Absorption A. Digestion 1. Starts with food preparation - softens tough, fibrous tissues of vegetables, fruits, and whole grains; swelling with water aids digestion 2. Mouth: salivary amylase breaks down starch into smaller polysaccharides and disaccharides 3. Stomach: salivary amylase inactivated by acidity of stomach 4. Small intestine a. Pancreatic amylase further digests polysaccharides b. Disaccharides are digested to monosaccharides by specific enzymes i. Maltase ii. Sucrose iii. Lactase 5. Large intestine: indigestible carbohydrates (dietary fibers and resistant starch) are fermented to acids and gases by bacteria 6. Intestinal diseases may interfere with carbohydrate digestion (e.g., lactose), leading to bloating, flatulence, and diarrhea B. Absorption 1. Glucose and galactose are actively absorbed with sodium 2. Fructose is absorbed by facilitated diffusion; slower process than active transport 3. 4. 5. 5.6 Once absorbed, monosaccharides are transported via portal vein to liver In liver, fructose and galactose are converted to glucose Glucose circulates from liver to body cells where it is used for energy or stored as glycogen (stored in liver and muscle) or fat (stored in adipose tissue) Health Concerns Related to Carbohydrate Intake A. Very High Fiber Diets 1. Fiber intakes about 50 - 60 g/d, especially combined with low fluid intake, can result in hard, dry stools, leading to painful elimination, hemorrhoids, rectal bleeding, or intestinal blockages 2. May decrease absorption of some minerals (e.g., zinc and iron) 3. May lead to inadequate calorie consumption in children, elderly, and malnourished individuals B. High Sugar Diets 1. Average American sugar intake is 20 tsp/d (82 g) 2. Provide empty calories, contribute to obesity 3. Excess consumption of sugar-sweetened drinks decreases milk consumption, leading to lower calcium and vitamin D intakes, thus diminishing bone health 4. Low-fat and fat-free snacks are usually made with lots of sugar 5. High intake of sugar (especially fructose) is associated with increased risk for CVD (decreased HDL and increased LDL) 6. Purported link between high sugar diets and hyperactivity in children is not supported by scientific evidence 7. Dental caries develop when oral bacteria metabolize sugars into acids, which dissolve tooth enamel and cause decay C. Lactose Intolerance 1. Primary lactose intolerance: insufficiency of lactase that develops after childhood in ~75% of the world’s population a. In North America, ~25% of adults have decreased lactose digestion b. Asian, African, or Latino/Hispanic individuals are more likely to have primary lactose intolerance than Caucasians c. Not all people with primary lactose intolerance experience symptoms d. Nearly all people with lactase deficiency can tolerate ½ to 1 c of milk with meals e. Hard cheese, yogurt, and acidophilus milk are well tolerated because lactose has been converted to lactic acid 2. Secondary lactose intolerance a. Conditions of the small intestine (e.g., Crohn’s diease or severe diarrhea) damage lactase-producing cells b. Symptoms are often temporary 3. Symptoms with ingestion of lactose a. Abdominal pain b. Bloating D. c. Gas d. Diarrhea Glucose Intolerance 1. Regulation of Blood Glucose a. Fasting blood glucose typically varies from 70 to 100 mg/dl b. Hyperglycemia: high blood glucose, above 126 mg/dl while fasting c. Hypoglycemia: low blood glucose, below 50 mg/dl i. Hunger ii. Shakiness iii. Irritability iv. Weakness v. Headache d. Liver regulates how much glucose from a meal is released into the blood and how much is stored as glycogen e. Pancreas releases hormones to regulate blood glucose i. Insulin promotes uptake of glucose by cells, storage of glucose and glycogen, thus lowering blood glucose when it is high ii. Glucagon prompts breakdown of glycogen to glucose when blood sugar is too low f. Adrenal glands secrete hormones to regulate blood glucose (fight or flight response) i. Epinephrine (adrenaline) triggers breakdown of glycogen to increase blood glucose ii. Norepinephrine triggers breakdown of glycogen to increase blood glucose iii. Cortisol decreases glucose use by muscle g. Pituitary gland i. Growth hormone decreases glucose use by muscle 2. Metabolic Syndrome a. Group of factors that increase risk of type 2 diabetes and CVD i. Insulin resistance or glucose intolerance (e.g., FBG >110 mg/dl) ii. Abdominal obesity (e.g., waist circumference >35” for women or 40” for men) iii. High blood triglycerides (e.g., >150 mg/dl), high LDL, low HDL (e.g., <40 mg/dl for men or <50 mg/dl for women) iv. Elevated blood pressure (e.g., >130/85 mmHg) v. Increased inflammatory proteins (e.g., C-reactive protein) b. Diagnostic criteria are not standardized; American Heart Association and National Heart, Lung, and Blood Institute suggest diagnosis based on presence of 3 or more of the above criteria c. Treatments include lifestyle modification focused on weight loss, decreased dietary fat intake, and increased physical activity 3. Hypoglycemia a. b. E. Can occur with or without diabetes Among people with diabetes, hypoglycemia may occur with use of too much insulin, low food intake, or exercising without increasing carbohydrate intake c. Reactive hypoglycemia i. Exaggerated insulin response after eating ii. Symptoms include irritability, sweating, anxiety, weakness, headache, and confusion occurring 2 - 5 hours after a meal d. Fasting hypoglycemia i. Low blood glucose after fasting for 8 hours or more ii. Usually caused by underlying medical condition (e.g., cancer, liver disease, renal disease) e. Diagnosis requires classic symptoms of hypoglycemia and BG <50 mg/d f. Treatment i. Regular meals with balance of protein, fat, and low glycemic load carbohydrates ii. Ample fiber iii. Substitute high-protein snacks for high-carbohydrate snacks iv. Spread carbohydrate intake throughout day v. Limit caffeine and alcohol Glycemic Index and Glycemic Load 1. Glycemic index (GI): ratio of blood glucose response of a given food compared with a standard (e.g., glucose or white bread) a. Influenced by i. Starch structure (amylose or amylopectin) ii. Fiber content iii. Food processing iv. Physical structure v. Temperature vi. Protein and fat content b. High GI foods i. Potatoes ii. Breads iii. Gatorade iv. Short-grain white rice v. Honey vi. Jelly beans c. Based on serving of food that supplies 50 g carbohydrate, which may or may not reflect typical serving size 2. Glycemic load: accounts for GI and amount of carbohydrate consumed: (g carbohydrate X GI)/100 3. Table 5-7 shows the GI and GL of common foods 4. Why GI and GL? a. 5. 5.7 High GL foods elicit increased insulin response followed by rapid drop in blood glucose b. Chronically high insulin increases blood triglycerides, fat deposition in adipose tissue, fat synthesis in liver, and rapid return of hunger after a meal c. Low GL foods typically contribute needed fiber Limitations of GI and GL a. Neither tool indicates blood glucose responses to mixed meals Medical Perspective: Diabetes Mellitus A. General 1. Diagnosis of diabetes is based on fasting blood glucose >126 mg/dl 2. Affects 6% of North Americans, leads to 200,000 deaths/year 3. 15% of North Americans show evidence of pre-diabetes (FBG 100 - 126 mg/dl) B. Type 1 Diabetes (insulin-dependent, juvenile-onset) 1. Classic symptoms of hyperglycemia a. Increased hunger b. Excessive thirst c. Excessive urination d. Weight loss 2. Caused by autoimmune attack on pancreas, leading to insufficient insulin production to allow glucose uptake by cells 3. Moderate genetic predisposition 4. Excess glucose excreted in urine 5. Experience ketosis as fats are broken down for energy; also causes electrolyte imbalances, dehydration, coma, or even death 6. Historical treatment included low-calorie, high-fat diet, which led to poor growth among children and poor compliance 7. In 1921, Banting and Best isolated insulin and used it as a treatment 8. Complications of type 1 diabetes a. CVD b. Kidney disease c. Nerve disease (neuropathy) i. Constipation or diarrhea ii. Amputations of limbs d. Blindness e. Infections 9. Treatment a. Insulin i. Injections ii. Pump b. Diet i. Regular meals and snacks ii. C. D. Regulated ratio of carbohydrate:protein:fat to maximize insulin action and moderate glucose excursions iii. Ample fiber iv. Balance calorie intake with expenditure v. Meets overall nutritional needs vi. Carbohydrate counting and diabetic exchange system are tools to regulate dietary intake c. Exercise enhances glucose uptake by muscles independent of insulin action d. Diabetes Control and Complications Trial demonstrated that development of CVD and nerve damage can be delayed with aggressive blood glucose control Type 2 Diabetes (non-insulin-dependent, adult-onset) 1. 90% of all cases of diabetes 2. 30 - 50% of cases of type 2 diabetes are asymptomatic 3. Characterized by insulin resistance, wherein cells become resistant to the action of insulin, thereby decreasing uptake of glucose by cells 4. Risk factors a. Strong genetic predisposition b. Obesity c. Physical inactivity d. Ethnicity (e.g., Latino/Hispanic, African, Asian, Native American, Pacific Islander) e. Metabolic syndrome f. Pre-diabetes 5. Treatment a. Diet i. Energy-controlled ii. Meets nutrient needs iii. Regular mealtimes iv. Limit total and saturated fat v. Moderate alcohol (1 drink/d) may increase HDL to reduce CVD risk, but must be consumed in conjunction with meals to avoid hypoglycemia b. Exercise c. Oral medications i. Reduce glucose production by liver ii. Increase insulin synthesis by pancreas iii. Slow intestinal absorption of glucose iv. Decrease insulin resistance d. Insulin (in advanced cases) Gestational diabetes 1. Occurs in 7% of all pregnancies E. 2. Treated with dietary therapy and insulin 3. Resolves after delivery 4. Increases maternal risk for developing type 2 diabetes later in life Decreasing the Risk of Diabetes and Protecting Health if Diabetes is Diagnosed 1. Maintain healthy body weight 2. Stay physically active 3. Follow MyPyramid guidelines 4. Regular testing of FBG for those with genetic predisposition