* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Practice-Based Learning and Designing a Quality Improvement
Survey
Document related concepts
Transcript
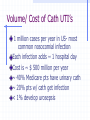
Practice-Based Learning and Designing a Quality Improvement Project Richard Schifeling, MD EBM Working Group November 15, 2007 Quality Improvement (QI) Experiment You are the hospital administrator at your institution in charge of QI You’ve just learned that CMS will no longer reimburse hospitals for care related to preventable cathetherassociated urinary tract infections What do you do? Administrator reaction Join the writers’ strike Look for a job in ambulatory care Form a committee to study the impact on your institution Check with infection control Check with nursing education & providers Beginning Oct. 2008, CMS to withhold payments: Catheter-associated UTI’s Vascular catheter-associated infections Mediastinitis post- CABG Pressure sores Falls Objects left in patients’ bodies Air embolism, incompatible blood tx’s CMS Methodology No reimbursement for select conditions: High cost or high volume or both Would result in higher payment as 2nd Dx Reasonably prevent by using evidencebased guidelines Volume/ Cost of Cath UTI’s 1 million cases per year in US- most common nosocomial infection Each infection adds ~ 1 hospital day Cost is ~ $ 500 million per year ~ 40% Medicare pts have urinary cath ~ 20% pts w/ cath get infection < 1% develop urosepsis Prevention of UTI’s Use catheters only when necessary and only as long as necessary- not for convenience of staff Staff training for aseptic management, proper irrigation and urine flow Handwashing Practice-Based Learning & Improvement Residents expected to: analyze practice experience & perform practice-based improvement activities locate, appraise, use “best practices” related to their patients’ health problems appraise clinical studies use information technology to manage info, support clinical care, pt education & own education Need for quality improvement Institute of Medicine (www.iom.edu) Quality of Health Care in America “To Err Is Human: Building a Safer Health Sytem” 1999 “Crossing the Quality Chasm: A New Health System for the 21st Century” 2000 Need for quality improvement Quality of healthcare can be measured Serious, widespread problems in quality throughout U.S. healthcare All systems affected: managed care, fee-for-service, big/ small communities Must change system of healthcare delivery to improve quality Chassin MR,JAMA1998;280:10005. Need for quality improvement U.S. healthcare at its best is superb Often it is not at its best resulting in population burden measured in: lost lives (IOM estimates 98K iatrogenic deaths each year in US hospitals) reduced functioning wasted resources Chassin MR,JAMA1998;280:10005. Definition of Quality Degree to which health services for individuals and populations: increase likelihood of desired outcomes are c/w current professional knowledge Systems of care/ critical factors Healthcare professionals practice in groups & systems of care Systems need to prevent/ minimize errors and harm Coordinate care for settings & providers Relevant/ accurate healthcare info must be available when needed Classification of quality of care issues/ opportunities Overuse, Underuse, Misuse Overuse: give service for which potential risk outweighs benefit Underuse: fail to give service for which potential benefit outweighs risk Misuse: appropriate service given in manner leading to avoidable risks Examples Overuse: Rx of antibiotic for URI, use urine catheter for convenience Underuse: lack beta-blocker post-MI, lack immunization, lack prenatal care, lack medication reconciliation Misuse: preventable complications like wrong-side surgery The 100,000 Lives Campaign: Getting Started Institute for Healthcare Improvement www.ihi.org/IHI/Programs/Campaign/ Six Changes That Save Lives Deployment of Rapid Response Teams…at the first sign of patient decline Delivery of Reliable, Evidence-Based Care for Acute Myocardial Infarction…to prevent deaths from heart attack Prevention of Adverse Drug Events (ADEs)…by implementing medication reconciliation Prevention of Central Line Infections…by implementing a series of interdependent, scientifically grounded steps called the “Central Line Bundle” Prevention of Surgical Site Infections…by reliably delivering the correct perioperative antibiotics at the proper time Prevention of Ventilator-Associated Pneumonia…by implementing a series of interdependent, scientifically grounded steps called the “Ventilator Bundle” Prevent Adverse Drug Events by Implementing Medication Reconciliation Reconciliation: A process of identifying the most accurate list of all medications a patient is taking—including name, dosage, frequency, and route—and using this list to provide correct medications for patients anywhere within the health care system Requires comparing the patient’s list of current medications against the physician’s admission, transfer, and/or discharge orders Medication Reconciliation IOM estimates 7000 deaths annually due to medication errors About 50% these errors occur at transition points (hosp admit, D/C, transfer to another unit) JCAHO makes medication reconciliation a National Patient Safety Goal Medication Reconciliation Requires change in system Emphasizes teamwork/ efficiency Improves patient safety Can improve medication errors at transition points ? Impact on adverse drug events and deaths- limited evidence thus far Institute of Medicine Vision of Future Quality Healthcare U.S. healthcare will be: Safe (avoiding patient injury) Effective (EBM & avoid overuse/underuse) Patient-centered (patient values) Timely (reducing waits and delays) Efficient (avoid waste) Equitable (no practice variability based on socioeconomics, race, gender, geography) Crossing the Quality Chasm 2000:5-6 Institute of Medicine Vision Current care systems can’t do the job They rely on outmoded systems of work Need redesigned systems of care for safer, high-quality care Need better use of information tech. to support clinical and administ. processes Institute of Medicine Vision Majority of healthcare services address ~ 15 to 25 conditions Focus attention on chronic care processes for these common conditions Evidence-based processes, supported by automated clinical info & decision support systems promise best outcomes QI project using EBM Consider common chronic care problem that needs improvement and has EBM best practice(s) Consider changes in system of healthcare needed to improve quality Consider how to measure performance pre-/ post-intervention & complete cycle QI Project Steps Choose specific area of care or provider education to improve Check project idea meets criteria Define best practice Measure current practice Change system to improve practice Measure post-intervention practice •Question(Hypothesis) *To know where to look, you need a hypothesis to guide you. *This is the key to any successful research(QI project) •Confronting Quality Problems *Underuse of Services *Overuse of Services *Misuse of Services *Variation of Services AHRQ: http://www.ahrq.gov/ IOM: http://www.nap.edu/catalog/10027.html?se_side • Evidence - review of the literature - finding similar questions and study designs - shows that EBM is fun http://hubnet.buffalo.edu/loginiphome.html Time Allocation •Decide your direction •Limit the scope •Schedule the time •Dedicate the time •Delegate the tasks •Start now! Attitude QI requires a positive attitude and the mindset to continue to ask questions.