* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hypophosphataemia in Adults - Nottingham University Hospitals
Survey
Document related concepts
Transcript
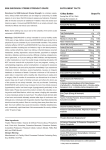
Title of Guideline (must include the word “Guideline” (not protocol, policy, procedure etc) Contact Name and Job Title (author) Directorate & Speciality Date of submission Date on which guideline must be reviewed (this should be one to three years) Explicit definition of patient group to which it applies (e.g. inclusion and exclusion criteria, diagnosis) Version Abstract Key Words Statement of the evidence base of the guideline – has the guideline been peer reviewed by colleagues? Evidence base: (1-6) 1 NICE Guidance, Royal College Guideline, SIGN (please state which source). 2a meta analysis of randomised controlled trials 2b at least one randomised controlled trial 3a at least one well-designed controlled study without randomisation 3b at least one other type of well-designed quasiexperimental study 4 well –designed non-experimental descriptive studies (i.e. comparative / correlation and case studies) 5 expert committee reports or opinions and / or clinical experiences of respected authorities 6 recommended best practice based on the clinical experience of the guideline developer Consultation Process Target audience This guideline has been registered with the trust. However, clinical guidelines are guidelines only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. Guideline for the Treatment of Hypophosphataemia in Adults Dr Peter Prinsloo Consultant Clinical Chemistry Azma Malik Senior Pharmacist Diagnostics and Clinical Support March 2016 March 2019 Guideline for Adult patients excluding critical care and renal. 3 This guideline describes the management of hyphosphataemia in adult inpatients Hypophosphataemia, hypophosphatemia, Phosphate 5 expert committee reports or opinions and / or clinical experiences of respected authorities Plus national advice in BNF Drugs & Therapeutics Committee (DTC) Consultant Clinical Chemistry Senior Pharmacist Critical Care Pharmacist Nursing, pharmacy & medical staff Guideline for the treatment of hypophosphataemia in adults. March 2016 1 GUIDELINES FOR THE TREATMENT OF ACUTE HYPOPHOSPHATAEMIA IN ADULTS Clinical guidelines are guidelines only. These guidelines are not intended to cover all factors relating to hypophosphataemia in critical care or the renal unit, where specialist advice should be sought. The interpretation and application of these guidelines remain the responsibility of the clinician. If in doubt, a senior colleague should be contacted. Intravenous phosphate is potentially dangerous and can cause fatal hypocalcaemia. This treatment must only be used within the recommendations of this guideline. Normal adult phosphate range = 0.8-1.45 mmol/L Severity of Hypophosphataemia Mild Moderate Severe Serum phosphate level (mmol/L) 0.65 - 0.79 0.32 - 0.64 <0.32 Symptoms usually occur when serum phosphate falls below 0.32 mmol/L Signs, symptoms and consequences of hypophosphatemia Generalised muscle weakness, myopathy Confusion, irritability, hallucinations, somnolence Paraesthesia Coma Hypotension Respiratory failure Rhabdomyolysis Decreased cardiac contractility Abnormal LFTs Cardiomyopathy, arrhythmias Seizures Guideline for the treatment of hypophosphataemia in adults. March 2016 2 Causes of hypophosphataemia Internal distribution *Refeeding syndrome, recovery from diabetic ketoacidosis, alkalosis, sepsis, drugs (see below) Decreased intestinal Vitamin D deficiency, diarrhoea, malabsorption, absorption vomiting, starvation Increased urinary Renal tubular defects, hyperparathyroidism, excretion disorders of vitamin D metabolism, diuretics, renal treatment. Dietary or internal Chronic alcoholism distribution *See refeeding syndrome guideline. http://nuhnet/nuh_documents/Guidelines/Trust%20Wide/Nutrition/1881.pdf Drug induced hypophosphataemia This is not an exhaustive list. Please contact Medicines Information, on extension 64185 for more details. Adrenaline Aminophylline Diuretics Beta2-agonists Insulin Phosphate binders Dopamine Steroids Sucralfate Theophylline Antacids Cautions Phosphate supplements should be started only once a definitive diagnosis is made. Intravenous phosphate should be used only when oral therapy has failed or is inappropriate or on the advice of a specialist. Potassium dihydrogen phosphate 9mmol in 250ml sodium chloride 0.9% contains 9mmol of potassium (in addition to 9 mmol of phosphate) per 250ml of solution. Caution should be used with infusion rate and in patients with hyperkalaemia. Monitor the patient’s potassium. If patient is hyperkalaemic, intravenous phosphate may be administered in the form of sodium glycerophosphate (see below). Guideline for the treatment of hypophosphataemia in adults. March 2016 3 Intravenous and oral phosphate should be used with caution in patients with severe renal impairment and dosage adjustment will be required. Large doses can result in metabolic acidosis. If creatinine clearance <15 ml/min, discuss with the renal team for specialist advice. Patients on a restricted sodium diet should be monitored carefully on both oral and intravenous therapy. Both serum phosphate level and the patient’s clinical condition should guide treatment. Caution should be exercised with replacement in the elderly. Patients with hypocalcaemia should have their calcium corrected before replacing phosphate to prevent further hypocalcaemia. Patients with severe hypercalcaemia who require phosphate replacement should be discussed with clinical chemistry or the renal team for specialist advice. Phosphate replacement in the presence of hypercalcaemia may cause ectopic calcification. The underlying cause of hypophosphataemia must be corrected. Diet Mild hypophosphataemia: phosphate may be replaced by increasing the dietary intake of foods high in phosphate. Dairy products are high in phosphate. Examples include: Milk, yoghurt and cheese. Dairy products also contain calcium, so serum calcium should be checked. Soft tissue calcification can occur if the patient suddenly develops hyperphosphataemia with elevated calcium levels Guideline for the treatment of hypophosphataemia in adults. March 2016 4 Oral replacement therapy: Phosphate Sandoz® effervescent tablets (Sodium Dihydrogen Phosphate anhydrous) - 1 tablet contains 16.1mmol of phosphate, 20.4mmol of sodium and 3.1mmol of potassium. Usual dose is one or two tablets three times a day adjusted according to response. Serum phosphate levels should be checked daily. Treatment may be discontinued once the plasma level is above 0.8mmol/L Oral phosphate supplements are often poorly tolerated due to diarrhoea. If this occurs, consider intravenous replacement. Administration of Phosphate-Sandoz® tablets at the same time as calcium, aluminium or magnesium salts should be avoided as these will bind phosphate and reduce its absorption. Phosphate Sandoz® effervescent tablets should be dissolved in 1/3 to 1/2 a tumblerful of water and taken orally. For patients who are nil by mouth, have diarrhoea, ileostomy, at risk of refeeding or a short bowel consider IV replacement. If patient is at risk of refeeding refer to trust refeeding guideline http://nuhnet/nuh_documents/Guidelines/Trust%20Wide/Nutrition/1881.pdf For IV replacement therapy: (Please note: Previously the product used for IV replacement was labelled as potassium acid phosphate 13.6% 9mmol in 250ml bag. It is now labelled as potassium dihydrogen phosphate 9mmol in 250ml) 9-27 mmol Potassium Dihydrogen Phosphate in 250-750 ml sodium chloride 0.9% should be infused over 12-24 hours The infusion should be repeated every 24 hours if needed until phosphate level is above 0.8mmol/L. Consider changing to oral phosphate if appropriate Ready-made bags are available from pharmacy as - 9mmol Potassium Dihydrogen Phosphate in 250mls sodium chloride 0.9%. Guideline for the treatment of hypophosphataemia in adults. March 2016 5 - If 18mmols is required 2 bags of 9mmols in 250ml will be prescribed, each bag should be given over 6 hours - If 27mmols is required 3 bags of 9mmols in 250mls will be prescribed each bag should be given over 4 - 8 hours (i.e. 27 mmols over 12- 24hrs) They are supplied from pharmacy in hours and via the on call pharmacist out of hours These bags are held only on designated ward areas only. Under no circumstances may wards borrow Potassium Dihydrogen Phosphate 9mmol bags from each other. All orders must be made through pharmacy. Monitor phosphate levels daily. Please note potassium dihydrogen phosphate is unlicensed. Use should be in accordance with the Trusts ULM policy If patient is hyperkalaemic, Sodium glycerophosphate 9mmol can be used instead of potassium dihydrogen phosphate 9mmol. Please note sodium glycerophosphate is unlicensed. This is made up on the ward. (Contact pharmacy for further advice) Doses for intravenous phosphate vary in the literature and suggested regimens have included 0.2-0.5mmol/kg/day up to a maximum of 50mmol/day. Administration of IV Phosphate The rate and concentration recommended for potassium infusions must never be exceeded (see separate Potassium guideline) Potassium dihydrogen phosphate should be administered using a volumetric pump. The dose and rate of phosphate infusion must be adhered to as stated in this guideline. Any deviations may result in harm to the patient. Guideline for the treatment of hypophosphataemia in adults. March 2016 6 Summary of treatment Phosphate level 0.32 - 0.6 mmol/L Asymptomatic <0.32 mmol/L Symptomatic *If refeeding risk see refeeding guideline Give oral Phosphate Sandoz ® one or two tablets three times a day. Adjust according to response Check level daily. Stop once level in normal range i.e. >0.8mmol/L Poor oral absorption or one of the below: Nil by mouth Short bowel syndrome Diarrhoea Ileostomy Give intravenous phosphate: Mild: 9mmol potassium dihydrogen phosphate Moderate: 18mmol potassium dihydrogen phosphate Severe: 27mmol potassium dihydrogen phosphate Potassium dihydrogen phosphate contains 9 mmol of phosphate in 250ml sodium chloride 0.9%. One, two or three bags may be required over 12-24 hours (see text on prescribing and volumes) Check phosphate and potassium levels daily If phosphate >0.32mmol/L on more than two occasions and patient is asymptomatic consider changing to oral supplementation if appropriate. Guideline for the treatment of hypophosphataemia in adults. March 2016 7 Monitoring Daily serum phosphate, calcium, magnesium and potassium levels. Excessive doses of phosphate may cause hyperkalaemia, hypocalcaemia and metastatic calcification. Patients with hypocalcaemia should have their calcium corrected before replacing phosphate to prevent further hypocalcaemia. Daily renal function Veins should be monitored for thrombophlebitis, especially if IV phosphate is given peripherally. The infusion must be stopped if patient develops adverse effects. Special Precautions and Warnings for Use Phosphate is renally cleared and therefore should be used with caution in patients with renal impairment. Insulin increases cell phosphate uptake and causes hypophosphataemia during treatment of diabetic ketoacidosis (DKA). An endocrinologist’s advice should be sought where appropriate. If the patient is receiving TPN, the potassium and phosphate content of the prescription must be taken into account. Liaise with the nutrition team. Adverse Effects Oral phosphate can cause diarrhoea and gastrointestinal upset. This is usually dose related and may be reduced by dividing the doses. Phosphate preparations are given as the potassium or sodium salts or both and may be associated with hyperkalaemia, hypernatraemia and dehydration. Sodium phosphate may cause hypokalaemia. Management of adverse effects involves withdrawal of phosphate, general supportive measures, and correction of serum electrolyte concentrations, especially calcium. Hazards of intravenous therapy include: hypotension, hyperkalaemia, hypernatraemia, hypocalcaemia, hyperphosphataemia, tetany, cardiac arrhythmias, metastatic calcification, and renal failure. Guideline for the treatment of hypophosphataemia in adults. March 2016 8 References 1. British National Formulary BNF https://www.medicinescomplete.com/mc/bnf/current/ accessed April 2016 2. UKMi Q&A - How is acute hypophosphataemia treated in adults? Accessed from: http://www.medicinesresources.nhs.uk/upload/documents/Evidence/M edicines%20Q%20&%20A/QA371_1_Hypophosphataemia.doc accessed on 10/01/16 3. Phosphate Sandoz®.Summary of Product Characteristics. Available at www.emc.medicines.org.uk.Updated 29/10/15. Accessed 18/01/16 4. R Edwards et al. Hypophosphataemia in the critically ill patientAetiology and management. Care of the critically ill.1998;14:8, 267-27 5. The Renal Drug Handbook, https://www.medicinescomplete.com/mc/renalhandbook/current/ Accessed May 2016 6. Lederer E, Ouseph R.,Mittal D, Deo D. Hyperphosphataemia available at www.emedicine.com/med/topic1135.htm#section~treatment/. Updated March 31st 2015. 7. Worcester Acute Hospital NHS Trust. Acute Treatment of Hypophosphateamia. March 2015 8. Uptodate. Updated 04th January 2016 Accessed 18/01/16 Guideline for the treatment of hypophosphataemia in adults. March 2016 9 Equality Impact Assessment Report 1. Name of Policy or Service Trust wide clinical guidance 2. Responsible Manager Owen Bennett (Clinical Quality, Risk and Safety Manager) 3. Name of person Completing EIA Azma Malik 4. Date EIA Completed 18/01/16 5. Description and Aims of Policy/Service This clinical guideline has been written to assist hospital staff in the management of adult patients with hypophosphateamia 6. Brief Summary of Research and Relevant Data Full references provided on document which include British National Formulary 7. Methods and Outcome of Consultation Drugs and Therapeutics Committee 8. Results of Initial Screening or Full Equality Impact Assessment: Equality Group Assessment of Impact Age No Impact Identified Gender No Impact Identified Race No Impact Identified Sexual Orientation No Impact Identified Religion or belief No Impact Identified Disability No Impact Identified Guideline for the treatment of hypophosphataemia in adults. March 2016 10 Dignity and Human Rights No Impact Identified Working Patterns No Impact Identified Social Deprivation No Impact Identified 9. Decisions and/or Recommendations (including supporting rationale) From the information contained in the procedure, and following the initial screening, it is my decision that a full assessment is not required at the present time. 10. Equality Action Plan (if required) N/A 11. Monitoring and Review Arrangements Review Guideline for the treatment of hypophosphataemia in adults. March 2016 11