* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Thank you for your assistance. - Southern Health NHS Foundation
Survey
Document related concepts
Neglected tropical diseases wikipedia , lookup
Trichinosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Transcript
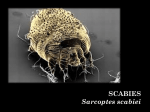
Appendix 6.1: Scabies Outbreak Pack (To be completed by Health Care Professional) Location of Outbreak: Date Outbreak Identified: Brief History: Name of Index Case: Date of confirmed diagnosis: Classical or Crusted Scabies: Please tick Classical Date & Time IPCT informed: Name of staff member informing IPCT Crusted Signature of IPCN : Initial Assessment of potential scabies cases Name of Person affected Service user or Staff DOB Description of Symptoms Investigations of Possible Source (include date symptoms (include details of rash, itching, dry flaky skin, previous diagnosis or treatment) first noticed, recent admission to hospital, attendance at day centres, contact with others with symptoms) Scabies Management Author: Angela Roberts Infection Prevention and Control Nurse Version: 2 September 2014 Communication, Diagnosis & Treatment Action Date & Time Signature Infection Prevention and Control Team informed Name of IPCN: Name of staff member who contacted IPCT: Manager/Senior Nurse informed Name: Medical staff/GP(s) informed Name(s): Dermatology advice sought: YES/NO Name of Dermatologist: Scabies Diagnosed: YES/NO Diagnosed by: Skin Scrapings Taken: YES/NO Results: Wessex Public Health England Centre informed Name: Other: Treatment Treatment to be used: (as advised by medical doctor/GP/dermatologist) Approach to Treatment: (As agreed between IPCT, Medical Dr, GP(s), Dermatologist (if involved) and the WESSEX PUBLIC HEALTH ENGLAND CENTRE) Treatment Options Advised by: Advice recorded by: (Name, date and sign) Planned date of first treatment: Planned date of second treatment: Targeted Treatment For symptomatic service users and staff only e.g. 1 identified service user or staff member and no other cases. Observe closely for any other cases Mass Treatment 2 or more cases of classical scabies 1 case of Crusted/Atypical scabies All service users’ and all staff contacts of diagnosed scabies case i.e. those that help out with personal care or have Scabies Management Author: Angela Roberts Infection Prevention and Control Nurse Version: 2 September 2014 2 prolonged hand holding / skin to skin contact. Scabies Management Author: Angela Roberts Infection Prevention and Control Nurse Version: 2 September 2014 3 Complete List of Symptomatic Cases: Those diagnosed with scabies Name DOB Bay / Room No. Date Admitted Date of Onset of Rash Diagnosis Confirmed & By Whom Date 1st Treatment Received Date 2nd Treatment received Date declared symptom free Monitoring Record for treated diagnosed cases of scabies. Name Detail rash & start date Type of 1st treatment & date Type of 2nd treatment & date Week 1 Date: Week 2 Date: Week 3 Date: Week 4 Date: Week 5 Date: Week 6 Date: Checked by – sign & progress comment Checked by – sign & progress comment Checked by – sign & progress comment Checked by – sign & progress comment Checked by – sign & progress comment Checked by – sign & progress comment Mon Mon Mon Mon Mon Mon Wed Fri Wed Fri Wed Fri Wed Fri Wed Fri Wed Fri Progress Comment Key Rash and/or Itching are: W – Worse I – Improving A – Absent NC – No Change Please NB: If symptoms DO NOT settle within 4 weeks, inform medical doctor / GP who may wish to re-treat or refer to a dermatologist. 5 Complete Service User Contact Tracing List: Those without a rash who have had prolonged skin to skin contact with affected case/s. Name of Index Case: Date of confirmed diagnosis: Location: Please record names of service users’ that have been in contact (prolonged skin-to-skin contacts of several minutes in past 8 weeks) with the index case. No 1 2 3 4 5 6 7 8 9 10 Name DOB Bay / room no. Date of 1st Treatment Date of 2nd Treatment (7 days later) Comments Complete Staff Contact Tracing List: Those without a rash who have had prolonged skin to skin contact with affected case/s. Name of Index Case: Date of confirmed diagnosis: Location: Please record names of service users’ that have been in contact (prolonged skin-to-skin contacts of several minutes in past 8 weeks) with the index case. No 1 2 3 4 5 6 7 8 9 10 Name DOB Date of 1st Treatment Date of 2nd Treatment (7 days later) Comments Checklist: Targeted Treatment ACTION Date completed Put up notice for visitors (Important Notice for Visitors) – Refer to outbreak pack appendix 6.1 Ensure all staff are aware of the outbreak, the infection control measures required and the symptoms to observe for in themselves, service users or family members. You may wish to distribute the information leaflets in this policy appendix 6.2 & 6.3 Identify all potential cases - check all service users for symptoms of scabies Inform any other care area that symptomatic service users or staff may have visited, so they can check for possible cases (include any staff agencies used) Ensure symptomatic staff obtain 2 treatments for themselves. Symptomatic household contacts only,can obtain treatment from their own GP. Obtain 2 treatments for symptomatic service users’ Treat symptomatic cases as soon as possible and retreat 7 days later 1st Treatment: 2nd Treatment: Observe and record progress of each case following treatment (at least 3 times a week) until they no longer have symptoms If symptoms do not settle within 4 weeks, inform medical doctor / GP who may wish to retreat or refer to a dermatologist Report any new cases to medical doctor /GP to be diagnosed and treated as for previous cases If there are a number of new cases, a mass treatment approach may need to be considered in liaison with the IPCT SHFT and WESSEX PUBLIC HEALTH ENGLAND CENTRE if appropriate. Ensure the list of cases is completed and keep records in case of further outbreak. Signature Checklist: Mass Treatment MASS TREATMENT Put up notice for visitors (Important notice for visitors) – refer to outbreak pack appendix 6.1 Ensure all staff are aware of the outbreak, the infection control measures required and the symptoms to observe for in themselves, service users or family members. You may wish to distribute the information leaflets in this policy appendix 6.2 & 6.3 Identify all potential cases - check all service users for symptoms of scabies Inform any other care area that symptomatic service users or staff may have visited, so they can check for possible cases (include any staffing agencies used). Identify a date and time (usually evening) when the first treatment will take place, allowing enough time to obtain the treatments and organise staff rotas (approximately a week in advance) Organise staff rotas to ensure that there are sufficient staff on duty on the treatment days, to be able to apply treatments to the service users’ and assist with washing treatments off at the specified time – see further down regarding how staff on duty will need to undertake their own treatments. Inform all staff and service users (and any visitors with very close contact i.e. those that undertake personal care) about the outbreak, the proposed action, how to obtain treatment and the dates planned for treatment. Ensure all staff (and any very close contacts of residents) obtain 2 treatments for themselves and ensure symptomatic staff have also obtained 2 treatments for each of their household contacts from a pharmacy or via their own GPs. Alternatively, identify the required amount for everyone and place an order with a local pharmacy. Obtain 2 treatments for all service users via medical doctor/GP. Ensure staff on duty on the treatment days (during the application of the treatment) are aware of the need to undertake their own treatment at home at the end of their shift. Ensure staff on duty during the removal of the treatment are aware of the need to complete their own treatment at home before starting their shift. Ensure there are sufficient amounts of clean clothes, linen and towels Date Completed Signature to use following treatment. Ensure everyone is treated on the treatment day (apart from those on duty during the application of treatment who will treat themselves at the end of their shift) and ensure this is repeated 7 days later. 1st Treatment: 2nd Treatment: Observe and record progress of each case following treatment (at least 3 times a week) If symptoms do not settle within 4 weeks, inform GP who may wish to retreat or refer to a dermatologist Report any new cases to GP(s) to be diagnosed and treated as a single case If there are a number of new cases, liaise with the GP(s) and WESSEX PUBLIC HEALTH ENGLAND CENTRE Ensure the list of affected people is completed and keep records in case of further outbreak. 10 PLEASE READ: IMPORTANT NOTICE FOR VISITORS Case(s) of scabies have been identified within this health care facility. Scabies is a skin problem caused by tiny mites that burrow into the skin, it is spread by prolonged skin to skin contact. Scabies is not a serious disease and the affected individuals will receive the appropriate treatment to eradicate the infestation. We would like to assure all visitors and relatives that expert advice has been sought and all appropriate actions are being undertaken. Scabies should be suspected if an itchy rash develops anywhere on the body, often symmetrical (present on both sides of the body) and particularly itchy at night and after bathing. Should you develop signs of scabies, you should inform the nurse / manager in charge, and make an appointment to see your GP. If you would like to know more about scabies infection, an information leaflet is available from staff who are happy to discuss any concerns you may have. Please continue to wash your hands on arrival and before leaving as a matter of routine. We assure you that we are taking all necessary action to prevent further cases. Thank you for your assistance.` 11 Appendix 16.2: Scabies Information Leaflets An Information Leaflet Advice about Scabies! What is Scabies? Scabies is an infestation of the skin with tiny mites called Sarcoptes scabei var hominis. The pregnant female mites burrow into the top layer of skin and lays about 2 -3 eggs per day before dying after 4 -5 weeks. Eggs hatch and develop into adults, mating occurs the male mite dies and the female life cycle repeats itself. The scabies mite has been associated with humans for thousands of years, and is no more unusual or frightening than head lice, an infestation can be unpleasant until it is treated. What are the symptoms? There may be no symptoms for 2 – 8 weeks in people who have normal immunity after infection, but then an allergy develops to the presence of the mites and their waste products. Usually there are 10 – 20 mites on an affected person. If a person has had scabies before a rash may appear within a few days. The rash is quite variable, but tiny raised red spots / pimples, often occur around the webs of the fingers, armpits, waist and groin. The scabies mites are attracted to thick folded skin but other areas of the body can also be affected. This is associated with intense itching, which is often worse at night or following a hot bath or shower. Sometimes you may be able to see the tiny mite burrows in the skin, seen as a fine dark or silvery line about 2 – 10 mm long commonly seen between the webs of the fingers. If scratching has occurred, the burrows may no longer be visible, reddening and secondary infection may occur. If the service user has an impaired immune system, neurological condition or altered skin sensation, they may develop a condition known as “atypical” or “crusted” scabies (sometimes called Norwegian scabies). They may not have shown any of the typical signs and symptoms of an infestation, but may harbour thousands of mites. This form of scabies is very contagious via direct skin to skin contact and through contact with contaminated clothing, bedding, soft furnishings. The sufferer’s skin thickens and becomes scaly, many mites can be shed on the skin scales, making spread to others much more likely. How might I have caught scabies? Scabies only lives on humans it is passed from person to person, usually by prolonged close skin to skin contact with a person who is infected with scabies e.g. holding hands or helping a resident to stand or walk, it is also spread via sexual skin to skin contact, please note – a quick handshake or hug is unlikely to spread the infection. If a member of your close family or a resident that you have close contact with has a scabies infection, it is possible you could catch it from them. What should I do if I think I have scabies? If you have symptoms that seem to indicate that you or someone you have close contact with may have scabies, you or the affected person should consult a doctor to have the diagnosis confirmed. Scabies Management Author: Angela Roberts Infection Prevention and Control Nurse Version: 2 September 2014 12 How is scabies treated? Use a suitable lotion or cream. LYCLEAR cream or DERBAC-M lotion are recommended. These can be prescribed by a hospital doctor your GP or local chemist shop. You will need two lots of cream or lotion per person as the treatment must be repeated after 7 days. Apply the lotion thinly over the whole body from the top of the head downwards. Don't get it in the mouth, nose or eyes. Make sure you include areas between the toes and fingers, underneath fingernails and around the genitals. Leave the lotion on as advised in the manufacturer’s instructions (usually 8-14 hours) and then wash it off. While the lotion is on, avoid washing, this is easier if the lotion is applied at night. If you wash your hands put on some more lotion afterwards. After the recommended time, have a bath or shower and put on clean clothes and change bed sheets. If you apply the medication correctly and leave it on for the correct length of time, it will kill all the mites after the first treatment. A second application of the lotion or cream is recommended after seven days. The treatment will kill the mites but itching may continue for 2-3 weeks afterwards. Your doctor will be able to advise on a suitable cream to reduce the irritation. There is no need for any special precautions with clothing or bedding other than washing on a hot washing machine cycle. Any items that cannot be washed in this way should be set aside and not used for seven days. Under these conditions mites will quickly become dehydrated and die. In a hospital setting the laundry will be treated as infectious. In crusted or atypical scabies more intensive treatment is necessary which may be continued for some time. Normal hygiene and vacuuming of chairs, beds and soft furnishings will minimise environmental contamination with skin scales. Should I stay away from work Stay away until the first treatment is completed, then return as normal. Service users if isolated can be taken out of their side rooms, if crusted scabies contact the hospital IPCT for further advice. Staff can return back to work. Will scabies spread among family members? It is important that all close family members in the same house are treated even if they do not have any symptoms. Everyone should be treated at the same time to ensure that they do not re-infect each other. As a carer, it is very important that you make sure your matron or manager is aware, if you are diagnosed with scabies as they will need to check if other staff or service users are affected. If you are worried that you may have become re-infected, discuss with your doctor so that if necessary you can be given further treatment. Where can I obtain more information about scabies? Talk to the nursing/medical staff on your ward or your GP if at home. For Infection Prevention and Control nurse advise contact us on: Tel: 02380 87 4291. Scabies Management Author: Angela Roberts Infection Prevention and Control Nurse Version: 2 September 2014 13