* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Is there Evidence to Support the use of Enteric Coated (EC) Aspirin
Survey
Document related concepts
Transcript
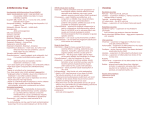
Medicines Q&As Is there Evidence to Support the use of Enteric Coated (EC) Aspirin to Reduce Gastrointestinal Side Effects in Cardiovascular Patients? Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Before using this Q&A, read the disclaimer at https://www.sps.nhs.uk/articles/about-ukmi-medicines-qas/ Date prepared: 31/3/2016 Background The use of low dose aspirin is part of the standard management plan for the prevention of cardiovascular events (1). Aspirin irreversibly inhibits cyclo-oxygenase (COX), an enzyme which controls the conversion of arachadonic acid to prostaglandins and thromboxanes. In platelets, this will reduce the formation of thromboxane A2 (TBX2), which is a vasoconstrictor and platelet aggregant. It also reduces the formation of prostacyclin in the vascular endothelium which acts as a potent vasodilator and anti-aggregant (2). Dyspepsia, gastrointestinal (GI) ulceration and haemorrhage are known adverse effects of aspirin therapy, potentially through a combination of direct damage and inhibition of prostaglandin synthesis in the gut mucosa (2). The enteric coated (EC) formulation of aspirin was developed and marketed in an effort to reduce GI adverse effects associated with aspirin therapy. EC aspirin has an outer layer designed to prevent aspirin from dissolving in the acidic environment of the stomach, but instead releasing its contents in the higher pH of the duodenum. Theoretically this should help protect the gastric mucosa from local irritation (although damage to the duodenum can still occur) (2). Thus EC aspirin is being prescribed in the belief that it will help reduce GI side effects in patients. There are reports however, that EC does not significantly reduce the risk of GI bleeding when compared to standard formulations of aspirin. There is also speculation that enteric coating may reduce the anti-platelet effect of aspirin due to a reduction in bioavailability, thereby reducing its clinical efficacy in prevention of cardiovascular events (3). This Q&A reviews the evidence on the use of EC aspirin to prevent GI damage, and also the effect of the enteric coating on the anti-platelet effect of aspirin. Answer Evidence surrounding the use of EC aspirin to reduce GI effects According to a Clinical Knowledge Summary (CKS) on anti-platelet therapy, available evidence does not demonstrate that EC preparations of aspirin reduce the risk of GI bleeding when compared to standard formulations (4). Walker et al. (2007) reviewed the published literature and identified one review, three large case control and cohort studies and five randomised controlled trials in healthy volunteers. Patients were randomised to either plain or EC aspirin (one study randomised to either EC, plain, or buffered Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As aspirin). Outcome measures included assessing mucosal damage by endoscopy, or incidences of GI bleeding. They concluded that overall the data were not robust enough to indicate a clinical benefit with regards to reduction of GI side effects with the use of EC aspirin (5). The review also concluded that the use of EC aspirin was associated with less mucosal damage. However, limitations of this research included only using a Medline search, no reported search strategy, no details given of the papers reviewed, and no attempt to aggregate data. The RCT’s reviewed by Walker et al. were small scale studies conducted in healthy volunteers, with study observation times ranging from 5 days to a maximum of 3 months, thus not directly applicable to the real life situation. Doses used were also much higher than that used in cardiovascular disease (CVD). The incidence of GI side effects with long term use of aspirin could therefore not be assessed from these trials. Additional studies have been identified that were not included in Walker et al 2007 literature review but these are also small scale trials conducted in healthy volunteers, with short observation periods. Outcome measures included estimation of faecal blood loss by measurement of radio-labelled erythrocytes within the faeces, or observation of the mucosal state using endoscopic methods. These studies indicated reduced blood loss or decreased GI ulceration with EC aspirin. However, these findings are based on weak evidence that cannot be used to definitively demonstrate the gastroprotective effects of EC aspirin. It should be borne in mind that EC will not protect against the systemic effect that aspirin has on prostaglandin synthesis, which increases the risk of gastric mucosal damage and ulceration irrespective of the formulation used. Evidence surrounding the anti-platelet effectiveness of EC aspirin compared to standard release Enteric coating of aspirin tablets delays the absorption time across the GI tract (6), and there is speculation that the bioavailability of EC aspirin is reduced compared to standard release tablets, resulting in reduced efficacy. The evidence for this issue consists of small randomised controlled trials conducted over 7-14 days and larger cohort studies. Participants were in the most part healthy volunteers, and outcome measures consisted of in vitro measurement of the bleeding times, extent of platelet aggregation, or inhibition of chemical mediators such as thromboxane and PGI2. Results of these studies were conflicting; with some showing that standard and EC formulations of aspirin were equally efficacious, and others showing the EC formulation to be less effective than standard release aspirin. Haastrup et al recently reviewed evidence from 7 articles: 4 studies compared EC with plain aspirin; 2 studies looked at responses following EC aspirin administration (no comparator); and 1 study compared EC with plain or with combination dypridamole + plain aspirin. Outcome measures were reductions in COX activity (namely by measuring TXB2 levels). There were 2 pharmacokinetic focused studies, one of which looked at plasma concentrations of aspirin and another looking at the acetylation of COX alongside TXB2 levels. Haastrup et al concluded that EC formulations can decrease the anti-platelet activity/effect of aspirin. They suggested that the formulation may also affect its pharmacokinetics. The potential pharmacokinetic pseudoresistance can mean it is necessary to administer higher doses of EC aspirin (in comparison to plain aspirin) over a longer duration to achieve sufficient and comparable effects (18). Limitations of Haastrup et al review were differences in populations studied (5 trials used healthy volunteers, 2 trials used patients with stable CVD) and differing definitions of insufficient anti-platelet effect with regards to COX inhibition. All studies included were short term studies (up to 2 weeks of treatment) and 3 of the studies had relatively small study populations (n=<25). Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As A summary of the studies on EC aspirin can be found in Tables 1 and 2. In addition, the clinical significance of these surrogate markers assessed are unknown. Summary Low dose EC aspirin tablets were developed and marketed in an effort to reduce the incidence of GI side effects in patients using it for prevention of CVD. Enteric coating prevents aspirin from dissolving in the stomach, which is instead released in the higher pH of the duodenum, theoretically protecting the gastric mucosa from local irritation. The available evidence is not robust enough to support a gastro-protective role of EC aspirin compared to standard release (plain) aspirin. There is speculation that enteric coating reduces the anti-platelet effect of aspirin, and thus its efficacy in the prevention of cardiovascular events. The available evidence for this is however conflicting. There is a theory of pseudoresistance reflecting delayed and reduced drug absorption with EC aspirin over normal plain aspirin. Additionally the studies employed the use of surrogate rather than clinical outcome measures to evaluate the anti-platelet efficacy of standard and EC formulations and the significance of these findings in practice is thus not known Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As Table 1: Evidence surrounding use of EC aspirin to reduce GI symptoms Author , Date and Study type Savon JJ et al. 7 Patient group Intervention Measurement of GI blood loss by obtaining 24 hour stool collections and measuring chromium-51 labelled erythrocyte loss. GI blood loss 1.12 ml (+/- 0.31)/ day with EC aspirin vs 2.6ml (+/- 0.68)/ day with plain aspirin. Reduced GI blood loss with EC compared to plain aspirin. Outcome measures were not correlated to actual clinical outcomes of the participants. 20 volunteers (aged 20-29) Each volunteer received 5 different treatments separated by a 10 day washout period: plain aspirin 300mg OD, EC aspirin 300mg daily, plain aspirin 600mg QDS, EC aspirin 600mg QDS Gastric damaged assessed endoscopically, and GI mucosal bleeding measured. No gastric mucosal injury seen with 300mg EC aspirin, and less GI mucosal injury seen with 600mg QDS EC aspirin compared to high dose plain aspirin. Small sample size and short follow up period. Volunteers were healthy and young. 19 healthy male volunteers Plain vs EC aspirin at a dose of 2.925g/day in divided doses. Estimation of faecal blood content by measurement of sodium chromate radioactive labelled RBC in stools. Measurement made prior to drug administration, then through days 4-7 of aspirin administration. Blood loss lower with EC aspirin use compared to plain aspirin 1.54ml vs 4.33ml, respectively. Small sample size of healthy volunteers only. Short term follow up (7 days). Outcome measures were not correlated to actual clinical outcomes of the participants. High dose aspirin used. 1991 RCT 1984 Study Weaknesses Plain aspirin (325mg) vs EC aspirin RCT Robbins DC et al.8 Key results 47 healthy volunteers 1995 Hawthorne AB et al.9 Outcome measures RCT Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As Table 2: Evidence for anti-platelet effectiveness Study Grosser et al.19 2013 Interventional Phase 1 study Patient group 400 healthy volunteers aged 18-55 years (median 26 years) Intervention Phase 1: Single dose 325mg EC aspirin vs single dose of 325mg plain aspirin. Phase 2: 14 day washout period, then repeat single dose test. Outcome measures Key results Study Weaknesses >50% reduction in COX activity (TXB2 levels and arachadonic acid induced platelet aggregation) – measured 4 and 8 hours post-dose administration. 83% had sufficient responses after singledose 325 mg EC Aspirin (apparent resistance) vs 100% after single-dose 325 mg plain aspirin. After 1 week of treatment, 98% had a sufficient response in individuals previously not responding to single-dose treatment. Healthy, relatively young volunteers. Limited drug exposure in vivo (single dose administration; phase 3 one week exposure): unreliability of basing a diagnosis of “aspirin resistance” on a single measurement of platelet aggregation. Phase 3: Non-responders for both phases, given repeated low-dose 81mg EC aspirin or 75mg clopidogrel for 1 week (cross-over design). EC aspirin “non-responders” after 4 hours: 49%, 8 hours: 17%. Pseudoresistance shown rather than a true drug resistance reflecting delayed and reduced drug absorption with EC aspirin over normal plain aspirin. Peace et al.20 2010 Cohort (Prospective) Cox D et al.10 2006 RCT Karha J et al. 2 236 patients with stable CVD (mean age 65yrs; mean weight 80kg) EC 75mg (n=148) vs plain 75mg aspirin (n=88). EC non-responders trialled on plain aspirin. If still non-responsive, doses were increased to 150mg. COX activity: TXB2 levels (goldstandard) and arachadonic acid induced platelet aggregation Observational study. Non-probability sampling method. Short follow up time of 14 days for each treatment group. Compliance issues. 71 healthy volunteers aged 20-50 years Each volunteer took 2 different aspirin preparations. Five preparations in total: 3 different EC formulations, dispersible and combined aspirin with dipyridamole TXB2 levels and arachadonic acid induced platelet aggregation. Treatment failure classified as <95% serum inhibition TXB2 Dispersible aspirin superior to other preparations in inhibiting TXB2. Treatment failure occurred in 3% of EC preparations, but not with dispersible aspirin Healthy, young volunteers used. Short follow up time of 14 days. No indication of actual clinical outcomes of participants. Low numbers of volunteers. 50 healthy volunteers > 18 7 day course of standard aspirin followed by 7 day course of EC aspirin (separated Platelet function using optical No difference in platelet inhibition between Excluded patients with cardiovascular disease, hypertension and hyperlipidaemia. 4.2% in the EC aspirin group had insufficient responses. Of these patients, once switched to plain aspirin, 70% showed responses. 2 weeks treatment in each group Available through Specialist Pharmacy Service at www.sps.nhs.uk Overall, 44/236 (19%), were found to have an inadequate responses (defined by insufficiently reduced TBX2 levels) to aspirin (both plain and EC). Medicines Q&As 2006 years by 3 week washout period). aggregometry. standard and EC aspirin. No indication of actual clinical outcomes of participants. 36 healthy male volunteers Comparison of 40mg plain aspirin, 100mg plain aspirin, 100mg EC aspirin. Platelet aggregation, platelet TXB2 release, serum TXB2, 6-keto-PGF1 alpha levels at baseline and 7 days after each medication Plain and EC 100mg tablets are equally effective in inhibition of platelet aggregation Small numbers of healthy volunteers used.. Short study time. No indication of actual clinical outcomes of participants. 10 volunteers EC aspirin vs. normal aspirin Bleeding times 4 hours after ingestion. Defined >8 minutes as abnormal bleeding time 10% of EC group developed abnormal bleeding times vs. 80% of normal aspirin. Low participant numbers. No indication of actual clinical outcomes of participants. 40 healthy male participants Standard and EC aspirin at doses of 81mg and 325mg. Adenosine diphosphate and epinephrine induce platelet aggregation at rest and after exercise. Measurements taken at baseline and 7 days post therapy. Equal inhibition of adenosine diphosphate and epinephrine induce platelet aggregation by standard and EC preparations. EC preparations caused less inhibition of 6-ketoprostaglandin F1 alpha. Short study time of 7 days. No indication of actual clinical outcomes of participants. 12 healthy volunteers aged 20-32 years Plain aspirin 300mg vs. plain aspirin 75mg vs. EC aspirin 300mg Measurement of platelet aggregation in response to different agonists Plain aspirin achieved its maximal effect after one dose. EC aspirin produced a sub maximal effect after one dose. No difference in extent of platelet after 2 doses. Small sample size of young, healthy volunteers. Short follow up time. No indication of actual clinical outcomes of participants 22 healthy volunteers 100mg alternate day dosing of plain aspirin vs. EC aspirin Platelet aggregation induced by arachadonic acid, adenosine diphosphate and epinephrine over 2 No difference found between regular and EC formulations Small sample size and short follow up time. No indication of actual clinical outcomes of participants. RCT Bode-Boger et a.l11 1998 RCT Gantt AJ et al. 12 1998 RCT Feng D et al. 13 1997 RCT May JA et al. 16 1997 RCT Ridiker P et al. 15 1996 Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As RCT weeks Gow JA et al. 17 1993 RCT 52 healthy male volunteers 80mg or 325 mg of plain aspirin daily, or 325mg EC aspirin daily. Bleeding times prior to therapy, day 1 and day 14 of aspirin therapy No significant difference between bleeding times of EC aspirin and plain aspirin No indication of actual clinical outcomes of participants Stampfer MJ et al.14 33 volunteers Randomised to plain aspirin 325mg, one of two EC aspirin preparations 325mg, or placebo. Tablets were taken every other day Bleeding times, platelet aggregation and TXA2 levels before and after a single dose, and after seven alternateday doses Plain and EC aspirin were equally efficacious in prolonging bleeding time, inhibition of platelet aggregation and suppression of TXA2. Short study time of 7 days. Alternate day dosing used. No indication of actual clinical outcomes of participants 1986 RCT Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As Limitations The majority of the included trials involved small numbers of subjects, use of healthy volunteers (some studies actively excluded patients with risk factors for cardiovascular disease), short study observation periods, and the use of surrogate outcome measures. In addition, evidence is conflicting between studies for anti-platelet efficacy. Furthermore, the data analysed came only from studies using plain aspirin as a comparator and not other formulations (i.e. buffered aspirin). A definitive conclusion therefore cannot be made from the available data regarding the GI safety of EC formulations compared to standard release aspirin References 1. Joint Formulary Committee. British National Formulary. [60th] ed. London: British Medical Association and Royal Pharmaceutical Society; [2016] 2. Anon. Which Prophylactic Aspirin? Drugs and Therapeutics Bulletin 1997 Vol 35;1 3. Karha J, Rajagopal V, Kottke-Marchant K et al. Lack of effect of enteric coating on aspirin-induced inhibition of platelet aggregation in healthy volunteers. American Heart Journal 2006; 151/5 (976.e7-11). 4. Anti-platelet treatment (Management) How should I manage someone at high risk of gastrointestinal bleeds? CKS [Clinical knowledge Summaries] last revised July 2009, accessed online via http://www.cks.nhs.uk/antiplatelet_treatment/management/quick_answers/scenario_anti-platelet_treatment#-385356 on 09/02/2016 5. Walker J, Robinson J, Stewart J et al. Does enteric-coated aspirin result in a lower incidence of gastrointestinal complications compared to normal aspirin? Interactive Cardiovascular & Thoracic Surgery 2007; 6: 519-22. 6. Drugdex® Consults, Non-steroidal anti-inflammatory agents effects on platelet function (2005). Thomson Micromedex, Greenwood village, Colorado USA. Accessed online via www.thomsonhc.com on 03/02/2011. 7. Savon JJ, Allen ML, DiMarino AJ Jr. et al. Gastrointestinal blood loss with low dose (325 mg) plain and enteric-coated aspirin administration. American Journal of Gastroenterology 1995; 90: 581-5. 8. Robbins DC, Schwartz RS, Kutny K et al. Comparative effects of aspirin and enteric-coated aspirin on loss of chromium 51-labeled erythrocytes from the gastrointestinal tract. Clinical Therapeutics 1984; 6: 461-6. 9. Hawthorne A.B., Mahida Y.R., Cole A.T et al. Aspirin-induced gastric mucosal damage: Prevention by enteric-coating and relation to prostaglandin synthesis. British Journal of Clinical Pharmacology 1991; 32: 77-83. 10. Cox D, Maree AO, Dooley M et al. Effect of enteric coating on anti-platelet activity of low-dose aspirin in healthy volunteers. British Journal of Clinical Pharmacology 1991; 32: 77-83. 11. Bode-Boger SM, Boger RH, Schubert M, et al. Effects of very low dose and enteric-coated acetylsalicylic acid on prostacyclin and thromboxane formation and on bleeding time in healthy subjects. European Journal of Clinical Pharmacology 1998; 54: 707-14. 12. Gantt AJ, Gantt S. Comparison of enteric-coated aspirin and uncoated aspirin effect on bleeding time. Catheterization & Cardiovascular Diagnosis 1998; 45: 396-9. Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As 13. Feng D, McKenna C, Murillo J et al. Effect of aspirin dosage and enteric coating on platelet reactivity. American Journal of Cardiology 1997; 80: 189-93. 14. Stampfer MJ, Jakubowski JA, Deykin D, et al. Effect of alternate-day regular and enteric-coated aspirin on platelet aggregation, bleeding time, and thromboxane A2 levels in bleeding-time blood. American Journal of Medicine 1986; 81: 400-4. 15. Ridker P.M., Hennekens C.H., Tofler G.H et al. Anti-platelet effects of 100 mg alternate day oral aspirin: A randomized, double-blind, placebo-controlled trial of regular and enteric coated formulations in men and women. Journal of Cardiovascular Risk 1996; 3:209-212. 16. May JA, Heptinstall S, Cole AT et al. Platelet responses to several agonists and combinations of agonists in whole blood: a placebo controlled comparison of the effects of a once daily dose of plain aspirin 300 mg, plain aspirin 75 mg and enteric coated aspirin 300 mg, in man. Thrombosis Research1997; 88: 183-92. 17. Gow JA, Ebbeling L, Gerrard JM. The effect of regular and enteric-coated aspirin on bleeding time, thromboxane, and prostacyclin. Prostaglandins Leukotrienes & Essential Fatty Acids 1993; 49: 515-20 18. Haastrup P.F, Gronlykke T, Jarbol D.E. Enteric coating can lead to reduced anti-platelet effect of low-dose acetylsalicylic acid. Basic and Clinical Pharmacology and Toxicology 2015; 116/3: 212215 19. Grosser T, Fries S, Lawson J et al. Drug resistance and pseudoresistance: An unintended consequence of enteric coating aspirin. Circulation 2013; 127/3: 377-385 20. Peace A, McCall M, Tedesko T et al. The role of weight and enteric coating on aspirin response in cardiovascular patients. Journal of Thrombosis and Haemostasis 2010; 8/10: 2323-2325 Quality Assurance Prepared by Reshma Chhana, Medicines Information, Guy’s and St Thomas’ Hospital, London Date Prepared 31/03/2016 Checked by Yuet Wan, Medicines Information, Guy’s and St Thomas’ Hospital, London Date of check 1/4//2016 Search strategy British National Formulary 70, Sept 2016 Online Edition: 70 September 2016, accessed online via www.bnf.org/bnf/bnf/current/104945.htm Summary of Product Characteristics. Boots Aspirin 75mg enteric coated Tablets, Boots Company PLC. Date of Revision August 2011. accessed online via www.emc.medicines.org.uk Micromedex accessed online via http://www.thomsonhc.com Available through Specialist Pharmacy Service at www.sps.nhs.uk Medicines Q&As Martindale, the Complete Drug reference. Accessed online via www.medicinescomplete.com NICE accessed online via www.nice.org.uk Clinical Knowledge Summaries (CKS) accessed online via www.cks.nhs.uk Scottish Intercollegiate Guideline Network (SIGN) accessed online via www.sign.ac.uk The Cochrane Library accessed via www.library.nhs.uk National Electronic Library for Medicines accessed online via www.nelm.nhs.uk MEDLINE search: exp TABLETS, ENTERIC-COATED/ [Limit to: Humans and English Language]; AND exp *ASPIRIN/ [Limit to: Humans and English Language] EMBASE Search: exp *ACETYLSALICYLIC ACID/ [Limit to: Human and English Language] AND *ENTERIC COATED TABLET/ [Limit to: Human and English Language] Available through Specialist Pharmacy Service at www.sps.nhs.uk