* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Treatment Options for Dementia
Survey
Document related concepts
Transcript
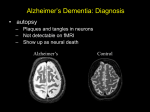
Treatment Options for Dementia Deb Bynum, MD Division of Geriatric Medicine University of North Carolina Objectives 1. Understand the use of cholinesterase inhibitors in the treatment of alzheimer type, vascular and mixed dementias 2. Review the current literature regarding the use of Memantine for severe dementia 3.Understand the appropriate use of nonpharmacologic strategies for behavioral problems with dementia 4. Review the appropriate use of antipsychotics for psychosis and behavioral symptoms in dementia 5. Discuss possible means of preventing dementia Overview 1. Cholinesterase inhibitors in the treatment of AD, vascular and overlap dementias 2. Memantine 3. Treatment of behavioral symptoms 4. ?Prevention 5. Future Directions The Cholinergic Hypothesis Depletion of acetylcholine and nicotinic receptors thought to occur early and relate to memory impairment with AD Focus on AD treatment with Acetylcholinesterase inhibitors: Recommended as first line treatment for patients with mild to moderate AD Cholinesterase Inhibitors Trials in patients with mild to moderate disease (10-24 on MMSE) On average these drugs seem to stabilize cognitive function and activities of daily living and may have benefits with QOL and behavioral disturbances for at least one year Side Effects: GI Tacrine Trials demonstrating delay of cognitive decline by 6 months Delayed time to nursing home placement: At 800 days, 45% in low dose or no tacrine underwent placement vs 21% in high dose tacrine group Evidence for long term cost effectiveness Reversible hepatotoxicity in 50% Donepezil (Aricept) Three large RCT demonstrate modest effectiveness in stabilizing cognitive function Well tolerated (no difference in adverse events compared to placebo) Not hepatoxic, no significant drug-drug interactions Single bedtime dose: start 5 mg, increase to 10 mg after 4-6 weeks Most common side effects: sleep disturbance, GI Rivastigmine May have increased selectivity for hippocampus and neocortex (areas affected by AD) Modestly effective in treatment of mild to moderate AD (but only at high doses of 6-12 mg/day) Recommended starting dose: 1.5 mg BID with breakfast and dinner Minimize GI side effects with 4-6 week titration, increasing to 3 mg BID, 4.5 mg BID, 6 mg BID More GI side effects, weight loss (dose dependent) Galantamine Potential second mechanism: modulator at nicotinic cholinergic receptor Three large RCTs indicate effectiveness in mild to moderate AD (same degree as other agents) at doses of 16, 24, 32 mg/day Open label 6 month extension of US trial: Possible disease modifying effect Starting dose: 4mg BID with meals, increase by 4mg BID every 4-6 weeks Cholinesterase inhibitors in moderate to severe AD RCT of donepezil vs placebo: 24 week international trial of 290 patients (MMSE 518) 63 % of donepezil treated patients were stable/better vs 42% in placebo group Comparison of Cholinesterase Inhibitors… Cochrane Dementia Group: 3 systematic reviews on efficacy of donepezil, rivastigmine, and galantamine Each drug seems to have similar treatment effect at 6 months on global and cognitive rating scales No double blind head to head trial Cholinesterase Inhibitors and AD: Summary Approved for treatment of mild to moderate AD Probably effective in treatment of more severe AD Goal: stabilization (not miracle drugs) Delay in nursing home placement, decline in ADLS Probably benefits behavioral and functional status as well Data suggest no big difference in efficacy among the 3 agents, although donepezil is easier to titrate and better tolerated Cholinesterase Inhibitors and Other Dementias… Vascular dementia and Dementia with Lewy Bodies each account for 10-15% cases Prominence of mixed pathology (especially vascular and AD in older population) Galantamine: Vascular and AD/Vascular Dementia Placebo controlled trial, 6 months, 592 patients 50% in study had AD plus radiological evidence of CVD, 41% had probable vascular dementia, 9% indeterminant Results for the whole group were similar to previous trials in typical AD : 74% galantamine groupwere improved/stable vs 59% in placebo group AD-CVD subgroup similar effects to prior trials with AD patients Summary of Galantamine and Vascular dementia Patients with typical features of AD mixed with features of CVD or evidence of CVD on radiological tests seem to respond similarly to patients with AD alone Subgroup with CVD alone does better over long term (even with placebo) Surprise: patients with what appears to be only CVD also seem to have some benefit (these patients not traditionally felt to have specific degeneration of cortical cholinergic pathways) Cholinesterase Inhibitors and Other dementias Lewy Body Dementia: may respond even more than AD patients Frontal Lobe Dementia: often respond adversely to cholinesterase inhibitors with increased agitation and insomnia Memantine NMDA (glutamate) receptor activation thought to be involved in neurodegeneration Memantine: NMDA antagonist aimed at protecting neurons from glutamate mediated excitotoxicity Approved in Europe in 2002 for treatment of severe AD (MMSE 3-14) Memantine Randomized, double blind, placebo controlled study: 166 patients with severe dementia (AD and vascular, MMSE <10) Cognitive and Behavioral Rating Scale significantly better with treatment, regardless of dementia type Other European studies have looked at treatment for moderate-severe Vascular Dementia, demonstrating similar efficacy Memantine 28 week RCT of 252 patients with severe AD (MMSE 3-14) in NEJM: memantine associated with less deterioration in cognitive and functional measures than placebo Problem: small numbers, high drop out rate Preliminary study: 400 patients with severe AD, 6 months RCT of memantine plus donepezil vs placebo plus donepezil: memantine group had significant benefit in comparison Memantine: Summary Approved for treatment of moderate-severe AD Likely of benefit also in severe vascular and mixed dementias as well Likely will be used in combination with donepezil or other cholinesterase inhibitors Cochrane Dementia Group: “memantine is a safe drug and may be useful for treating AD, vascular and mixed dementia, although most of the trials so far reported have been small and not long enough to detect clinically important benefit” Behavioral Symptoms: Nonpharmacologic Treatment Depression, agitation, aggression, wandering, sleep disturbance, paranoia, anxiety Assess for/treat depression Assess cause for increased symptoms (caregiver, environmental changes, medications, infection) Assess for caregiver depression ID and avoid triggers of negative behavior Redirection Environmental modification for wandering Sleep hygiene Use of Atypical Antipsychotics Older, “typical” agents such as haloperidol and thioridazine (mellaril) associated with significant extrapyramidal symptoms Theoretically combination of dopamine and serotonin effects of atypical agents allow treatment of positive and negative psychotic symptoms with less EPS Risperidone Evidence demonstrates efficacy in treatment of psychotic and behavior symptoms in patients with dementia Exacerbates movement disorder in patients with Parkinson’s Start .25/day, average daily dose 1-1.5mg/day EPS in dose dependent manner (6mg/day) Insomnia, hypotension, weight gain Elevation of prolactin levels Olanzapine Evidence that it is effective in AD patients Increases motor symptoms in PD patients Recommended not to use with PD Start: 1.25-2.5/day, increase to 5/day (dosages of 10-15/day are not more effective!) More sedating than others (more anticholinergic effects) Sedation, weight gain, orthostatic hypotension, seizures, glucose intolerance Quetiapine (Seroquel) Showing promise in patients with AD and PD Does not exacerbate movement disorder of PD May be first line for PD patients with psychosis 12.5 QHS, titrate every 3-5 days Sedation, HA, orthostatic hypotension ?Cataract formation Ziprasidone (Geodon) New, clinical data lacking Non dose-dependent QT prolongation Clozapine Very effective in treating psychosis in PD patients The most effective agent in treatment of drug induced psychosis in PD Some efficacy with AD patients Start: 6.5mg/day Agranulocytosis, frequent monitoring limits use Antipsychotics in Dementia: Summary Start very low, monitor for hypotension, P450 effects, sedation, EPS Monitor and avoid use as “chemical restraint” Avoid if at all possible in Dementia with Lewy Bodies ?Prevention of Dementia HTN and Hyperlipidemia – – Observational studies show less risk of AD in patients on statin agents (RCTs do not show effect) Original HTN in Elderly studies: patients initially on placebo with systolic HTN had persistent elevation in risk of dementia Vascular risk factors seem to play role even for AD! Evidence lacking for Vit E, Estrogen, NSAIDS Future Directions Amyloid B peptide (plaque component) vaccination Amyloid modulators ?Anti-inflammatory drugs Treatment with statins ?Low flow VP shunting Take Home Points Cholinesterase Inhibitors are MODESTLY effective in treatment of mild to moderate AD Cholinesterase Inhibitors are probably effective in more severe AD No large difference in efficacy between agents, but Donepezil more easily titrated and tolerated Evidence to support use of cholinesterase inhibitors for vascular and vascular/AD dementia Memantine looks to be effective for more severe AD and vascular dementia, will likely be used in combination with cholinesterase inhibitors Take Home Points Behavioral symptoms common, first line of treatment is nonpharmacologic Atypical antipsychotics can be effective, but use in low doses and watch carefully for problems (especially EPS, hypotension) For PD, quetiapine (seroquel) may be first line for psychotic symptoms Avoid antipsychotics with Lewy Body Disease!