* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
inflammatory bowel diseases
Ulcerative colitis
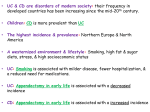
Ulcerative colitis (UC) is a chronic idiopathic inflammatory disease of the gastrointestinal tract that
affects the large bowel and is a major disorder under the broad group of conditions termed
inflammatory bowel diseases (IBDs).
UC can occur at any age, although diagnosis before the age of five years or after 75 years is uncommon.
The peak incidence of UC occurs in the second and third decades of life. and a male-to-female ratio of
nearly 1 : 1 applies to all age groups.
At the time of initial presentation, approximately 45% of patients with UC have disease limited to the
rectosigmoid, 35% have disease extending beyond the sigmoid but not involving the entire colon, and
20% of patients have pancolitis.The disease typically is most severe distally and progressively less severe
more proximally. In contrast to Crohn's disease, continuous and symmetrical involvement is the hallmark
of UC , with a sharp transition between diseased and uninvolved segments of the colon.
Macroscopically, the mucosa in UC appears hyperemic, edematous, and granular in mild disease. As
disease progresses, the mucosa becomes hemorrhagic, with visible punctate ulcers.
Epithelial regeneration with recurrent attacks results in the formation of pseudopolyps,
which is typical of long-standing UC but which also may be seen in acute disease . Another
characteristic appearance of long-standing disease is atrophic and featureless colonic
mucosa, associated with shortening and narrowing of the colon. Patients with severe disease
can develop acute dilatation of the colon.
Microscopically, Neutrophilic infiltration of colonic crypts gives rise to cryptitis and
ultimately to crypt abscesses with neutrophilic accumulations in crypt lumens. the acute
inflammatory infiltration results in the characteristic histopathology of goblet cell mucin
depletion, formation of exudates, and epithelial cell necrosis. Inflammation in UC
characteristically is confined to the mucosa, in contrast to the transmural involvement of
Crohn's disease. A classic histologic feature of chronic UC is crypt architectural distortion .
Most of these pathologic findings are not specific for UC. Features that reflect chronicity
and thus argue against a diagnosis of infectious or acute self-limited colitis include distorted
crypt architecture, crypt atrophy, increased intercrypt spacing to fewer than six crypts per
millimeter, an irregular mucosal surface, basal lymphoid aggregates, and a chronic
inflammatory infiltrate.
CLINICAL FEATURES
Patients with UC can present with a variety of symptoms. Common symptoms include diarrhea,
rectal bleeding, passage of mucus, tenesmus, urgency, and abdominal pain. In more-severe
cases, fever and weight loss may be prominent. The onset of UC typically is slow and insidious.
Symptoms usually have been present for weeks or months by the time the typical patient seeks
medical attention. Most (80%) patients with UC have a disease course characterized by
intermittent flares interposed between variable periods of remission.
EXTRAINTESTINAL MANIFESTATIONS:
1-CUTANEOUS/ORAL:The most common dermatologic manifestations of UC are
complications of drug treatment. These include hypersensitivity, photosensitivity, and
urticarial rashes related to sulfasalazine and less commonly to mesalamine. Patients
receiving glucocorticoids often develop acne, which can be distressing cosmetically.
Other common dermatologic manifestations associated with UC are erythema nodosum
and pyoderma gangrenosum. Erythema nodosum classically manifests as single or
multiple tender, raised, erythematous nodules on the extensor surfaces of the lower
extremities while Pyoderma gangrenosum may be single or multiple and usually occur
on the trunk or extremities but can develop on the face, breast, or sites of trauma,
including stoma and intravenous sites. The classic lesion begins as erythematous
pustules or nodules that break down, ulcerate, and coalesce into a larger, tender,
burrowing ulcer .
2-OPHTHALMOLOGIC:The two most common ocular manifestations associated with UC
are episcleritis and uveitis, occurring in 5% to 8% of patients. Episcleritis is
characterized by painless hyperemia of the sclera and conjunctiva without loss of
vision. In contrast, uveitis presents as an acute or subacute painful eye with visual
blurring often accompanied by photophobia and headache.
3-MUSCULOSKELETAL:Peripheral arthropathy occurs in 5% to 20% of patients with UC.
The risk of arthropathy increases with the extent of colonic disease. Peripheral
arthropathy can be classified into two distinct types , Type 1 is asymmetrical and
pauciarticular, affecting fewer than five joints and typically involving the large joints
(knees, elbows, ankles). It usually manifests with acute, self-limited episodes that
parallel the underlying bowel disease activity. Type 2 arthropathy is symmetrical and
polyarticular, affecting five or more joints and typically involving the small joints.Axial
arthropathy occurs less often than does peripheral arthropathy in patients with UC and
includes sacroiliitis and spondylitis. Most patients with sacroiliitis are HLA-B27
negative and do not progress to ankylosing spondylitis.Ankylosing spondylitis occurs in
1% to 2% of patients with UC, and most of these patients are HLA-B27 positive.
Symptoms of ankylosing spondylitis can appear long before or after the onset of the
intestinal symptoms and are independent of the activity of colitis.
4-HEPATOBILIARY:The most important hepatobiliary complication associated with UC is
PSC, which occurs in approximately 3% of patients . PSC should be excluded in patients
with UC who have persistently abnormal liver biochemical tests or evidence of chronic
liver disease. PSC is independent of the underlying colitis.
Truelove and Witts Classification of the Severity of Ulcerative Colitis
Mild
<4 stools/day, without or with only small amounts of blood
No fever
No tachycardia
Mild anemia
ESR < 30 mm/hr
Moderate
Intermediate between mild and severe
Severe
>6 stools/day, with blood
Fever > 37.5?C
Heart rate > 90 beats/min
Anemia with hemoglobin level < 75% of normal
ESR > 30 mm/h
ENDOSCOPY
The diagnosis of UC can be strongly suggested by sigmoidoscopy in most cases. In patients
presenting with their first attack of UC, sigmoidoscopy with biopsies usually is sufficient to
confirm the diagnosis, thereby allowing initiation of therapy. In patients with active flares,
sigmoidoscopy is best performed in unprepared bowel so the earliest signs of UC can be
detected without the hyperemia that is often present because of preparative enemas.
Colonoscopy is not recommended in patients with severely active disease for fear of
perforation.The hallmark of UC is symmetrical and continuous inflammation that begins in the
rectum and extends proximally without interruption for the entire extent of disease. The
earliest endoscopic sign of UC is a decrease or loss of the normal vascular pattern, with
mucosal erythema and edema ; distortion or loss of vascular markings may be the only
endoscopic evidence of UC in patients with quiescent disease. As disease progresses, the
mucosa becomes granular and friable. With more-severe inflammation, the mucosa may be
covered by yellow-brown mucopurulent exudates associated with mucosal ulcerations. Finally,
severe UC is associated with mucosa that bleeds spontaneously. In patients with long-standing
UC, pseudopolyps may be present. There is a loss of normal colonic architecture with longstanding inflammation that is characterized by muscular hypertrophy, loss of the normal
haustral fold pattern, decreased luminal diameter, and shortening of the colon; a resultant
featureless appearance of the colon in chronic UC gives rise to the lead pipe appearance seen
on barium enema. Strictures can occur in patients with chronic UC and result from focal
muscular hypertrophy associated with inflammation. Malignancy must be excluded in patients
with UC who have strictures, particularly long strictures without associated inflammation and
strictures proximal to the splenic flexure.
Endoscopic Assessment :
0 Normal mucosa
1 Loss of vascular pattern
2 Granular, nonfriable mucosa
3 Friability on rubbing
4 Spontaneous bleeding, ulceration
TREATMENT:
The goals of therapy of UC are to induce remission, to maintain remission, to maintain adequate nutrition, to
minimize disease- and treatment-related complications, and to improve the patient's quality of life. Current
management strategy focuses on using appropriate medical therapy and optimizing timing of surgery.
Aminosalicylates
Oral:
Sulfasalazine consists of an antibacterial component, sulfapyridine, bonded by an azo bond to a salicylate, 5aminosalicylic acid (5-ASA, mesalamine),given at a dose of 3 to 6 g/day.
Topical:
Topical aminosalicylates can be administered in the form of 5-ASA enemas, 5-ASA suppositories, and, in
Europe, 5-ASA foam. The use of enemas allows the medication to be delivered up to the level of the splenic
flexure in about 95% of patients, and suppositories can be used to treat disease up to 15 to 20 cm from the
anal verge.
Glucocorticoids:
Systemic:
At doses equivalent to 40 to 60 mg/day of oral prednisone, glucocorticoids are effective firstline therapy for moderate or severe flares of UC.
Topical:
Topical glucocorticoids in liquid and foam formulations are effective short-term therapy for
active UC distal to the splenic flexure.Foam preparations often are tolerated better by
patients and may be easier to retain than liquid preparations. Topical glucocorticoids have
been found to be less effective than topical mesalamine for inducing remission of distal UC;
however, the combination of topical corticosteroids and topical mesalamine has been more
efficacious than either alone in the short-term treatment of distal UC.
Immunomodulators:
Azathioprine and 6-Mercaptopurine:
the use of azathioprine for maintenance of remission in UC for any case that need steroid for
induction treatment.
Cyclosporine:
Cyclosporine A is a potent inhibitor of cell-mediated immunity. Its use in UC is primarily in
patients with severe, steroid-refractory disease.
Biological Therapy(Anti-Tumor Necrosis Factor Antibodies):
TNF is a key proinflammatory cytokine that has been demonstrated to play a role in several disease states, including
IBD. Elevated TNF concentrations have been found in inflamed intestine in patients with Crohn's disease and UC,
and stool and mucosal concentrations of TNF in patients with IBD have been shown to correlate with clinical disease
activity. Infliximab (Remicade) is a chimeric monoclonal antibody of IgG1 subclass directed against human TNF-α. It
consists of 75% human and 25% murine components. Infliximab is now accepted as part of the standard treatment
options in patients with UC. Two other anti-TNF agents, adalimumab and certolizumab pegol, have shown efficacy
for the induction and maintenance of remission in Crohn's disease but have not yet been studied in patients with
UC.
Induction Therapy for Ulcerative Colitis Based on Disease Severity:
Mild Disease
5-Aminosalicylates { Topical (distal colitis), Oral (distal/extensive colitis), Combination}
Moderate Disease
5-Aminosalicylates { Topical (distal colitis), Oral (distal/extensive colitis) , Combination}
Glucocorticoids { Topical (distal colitis) , Oral (distal/extensive colitis) , Combination}
Azathioprine or 6-mercaptopurine
Severe Disease
IV glucocorticoids
IV cyclosporine
IV infliximab
Maintenance Therapy for Ulcerative Colitis:
5-Aminosalicylates { Topical (distal colitis), Oral (distal/extensive colitis) }}
Azathioprine or 6-mercaptopurine
Infliximab
COMPLICATIONS:
1-TOXIC MEGACOLON:
Toxic megacolon is defined as acute colonic dilatation with a transverse colon diameter of greater than 6 cm
(on radiologic examination) and loss of haustration in a patient with a severe attack of colitis.Maximal colonic
dilatation most commonly is observed in the transverse colon.
2-STRICTURES:
Colonic strictures complicate UC in approximately 5% of patients, most commonly in those with extensive and
long-standing colitis. Patients with colonic strictures usually present with alterations in bowel habits, both
constipation and diarrhea. Clinically significant obstruction is rare. Colonic strictures complicating UC
typically are short (2 to 3 cm), occur distal to the splenic flexure, and represent hypertrophy and thickening
of muscularis mucosa rather than fibrosis.There needs to be a high index of suspicion of malignancy in
patients with colonic strictures associated with UC, especially when the strictures are located proximal to the
splenic flexure.
3-DYSPLASIA AND COLORECTAL CANCER :
Patients with UC have an increased risk of colorectal cancer. This risk depends on several factors, the most
important being the duration( after 8 years of disease age) and extent of the disease. Other risk factors
include PSC, family history of colon cancer, age at diagnosis of disease, severity of inflammation, presence of
pseudopolyps, and possibly backwash ileitis.
Crohn's Disease
Crohn's disease is a condition of chronic inflammation potentially
involving any location of the alimentary tract from mouth to
anus, but with a propensity for the distal small bowel and
proximal large bowel. Inflammation in Crohn's disease often is
discontinuous along the longitudinal axis of the intestine and can
involve all layers from mucosa to serosa. Affected persons
usually experience diarrhea and abdominal pain, often
accompanied by weight loss. Common complications include
strictures and fistulas, which often necessitate surgery. The
presence of granulomas and fissureon histopathology is highly
characteristic of Crohn's disease.
FEATURE
Mucosal lesions
CROHN'S COLITIS
ULCERATIVE COLITIS
Aphthous ulcers are common in
early disease; late disease is
notable for stellate, rake, bearclaw, linear, or serpiginous ulcers
and cobblestoning
Micro-ulcers are more common, but
larger ulcers are possible
Pseudopolyps are more common
Distribution
Continuous, symmetrical, and diffuse,
Often discontinuous and
with granularity or ulceration found in
asymmetrical, with skipped
entire involved segments; however,
segments of normal intervening
periappendiceal inflammation (cecal
mucosa, especially in early disease patch) is common, even when the cecum
is not involved
Rectum
Complete, or more often relative, Typically involved with variable proximal
rectal sparing
distribution
Ileum
Often involved (approximately 75% Not involved, except as backwash ileitis
of cases)
in panulcerative colitis
Depth of inflammation
Mucosal, submucosal, and
transmural
Mucosal; transmural only in fulminant
disease
Rectum
Complete, or more often relative,
rectal sparing
Typically involved with variable
proximal distribution
Ileum
Often involved (approximately 75% of Not involved, except as backwash
cases)
ileitis in panulcerative colitis
Depth of inflammation
Mucosal, submucosal, and transmural
Serosal findings
Marked erythema and creeping fat
Absent except in severe colitis or toxic
(the latter is virtually pathognomonic) megacolon
Perianal complications
Often prominent, including large anal
Not prominent (fissure or fistula if
skin tags, deep fissures, perianal
present, should be uncomplicated)
fistulas, that are often complex
Strictures
Often present
Rarely present; suggests
adenocarcinoma
Fistulas
Perianal, enterocutaneous,
rectovaginal, enterovesicular, and
other fistulas may be present
Absent, except for rare occurrence of
rectovaginal or perianal fistula
Mucosal; transmural only in fulminant
disease
Histopathology
Granulomas are present in 15%-60% of
patients (higher frequency in surgical
specimens than in mucosal pinch
biopsies)
Granulomas should not be present (microgranulomas
may be associated with ruptured crypt abscess)
Crypt abscesses may be present
Crypt abscesses and ulcers are the defining lesion
Focally enhanced inflammation, often on
Ulceration on a background of inflamed mucosa
a normal background, is the hallmark
Serology
pANCA in 20%-25%
ASCA in 41%-76%
pANCA in 60%-65%
ASCA in 5%
Treatment: same as UC in addition to:
Methotrexate:
Methotrexate may be considered as an alternative to the thiopurine analogs,
particularly among patients who do not tolerate these drugs. Some patients who
do not respond to 6-MP might respond to methotrexate. In addition to its proven
role as a glucocorticoid-sparing agent, methotrexate may be considered as a
treatment for active disease, although its value for this indication is less clear.
2-Antibiotics:
Antibiotics have a clear role in treating pyogenic complications of Crohn's
disease. On the basis of relatively little evidence, antibiotics also are used to
treat perineal disease, fistulas, and active luminal Crohn's disease. The largest
reported experience has been with metronidazole. The anaerobic flora affected
by metronidazole might have particular importance in the pathogenesis of
Crohn's disease.