* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Parkinson`s Disease: How Pharmacists Can
Survey
Document related concepts
Transcript
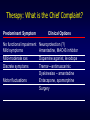
Parkinson’s Disease: How Pharmacists Can Make a Difference Marsha K. Millonig, MBA, RPh President & CEO Catalyst Enterprises, LCC Disclosure Information Parkinson’s Disease Marsha K. Millonig I have no financial relationship to disclose. AND I may discuss off-label/investigational use in my presentation. Objectives • Identify the visual and clinical testing tools used to diagnose PD • Identify the classes of medications used to treat PD • Understand the pros and cons of each class of medications and when to use these medications • Understand how concomitant disease states and medications that could lead to further exacerbation of PD symptoms and how to avoid these situations • Understand ways that pharmacists can assist PD patients, their caregivers, and physicians to properly manage their condition What is Parkinson’s Disease? • Chronic, progressive condition • Motor symptom disorders • Dysfunction/degeneration of dopaminergic neurons • Domaminergic neurons in the substantia nigra control proper coordination and muscle group movement Pathophysiology Lewy body: Dense Core with Halo • Lewy body structures also • Inclusions of αsynuclein • Disrupts normal neuronal function Pathophysiology • Cell death due to dopaminergic neuron degeneration may be occurring up to 6 years before symptoms appear • When symptoms appear, about 70% to 80% of the neurons have been lost • Autonomic, cognitive, other non-motor symptoms usually appear before the motor symptoms Autonomic Dysfunctions • • • • • • • Constipation Dry mouth Urinary retention/incontinence Erectile dysfunction/decreased libido Orthostatic hypertension Drooling Heat/cold intolerance Cognitive Impairments • Apathy • Anxiety – Occurs in 20% to 40% patients • Depression – Occurs in 40% of patients • Psychosis Other Non-Motor Symptoms • • • • • • Unilateral aches and pains Fatigue Restlessness Paresthesias Sensation of internal tremor Continue as the disease progresses Causes… Aging Genes PARK 1-10 -synuclein Nurr-1 Parkin UCH-L1 Pathogenic Cascade Failure of UPS Protein aggregation Mitochondrial dysfunction Oxidative stress Excitotoxicity Neuroinflammation Environment Pesticides Agricultural toxins Other (?) Spreading Apoptosis (cell death) UCH-L1 = ubiquitin hydrolase L1 UPS = ubiquitin proteosome system Drawing by Jack Chen, Western University, Adapted from: McNaught K St P et al. Ann Neurol. 2003; Olanow CW, Tatton WG. Annu Rev Neurosci. 1999; Steece-Collier K et al. Proc Natl Acad Sci USA. 2002; Vila, Przedborski. Nat Rev Neurosci. 2003. May be Some Protective Factors Alcoholism Coffee Smoking OR = 0.41 OR = 0.35 OR = 0.69 (0.19-0.89) (0.16-0.78) (0.45-1.08) Ragonese et al. Neuroepidemiology 2003 From Chen/Fagan 2005. Ascherio et al. Am J Epidemiol 2004 Tanner et al. Neurology 2002 Quik M. Trends Neurosci 2004 Wirdefeldt et al. Ann Neurol 2005 Scope of the Problem • 1 million Americans • 2nd most common neurodegenerative disease • Average age of onset: 60 years • 5%-10% cases in people under 50 years • Slightly more men than women • Lifetime risk: 1 in 45 • Progression: 10-20 years or more Cost of the Problem • • • • $6 billion Direct and indirect costs Treatment Psycho-social care Does anyone have a family or friend with PD? Impact • Reduced quality of life • Worse than CHF, CVA, back pain, OA, DM, CHD • Trouble with daily routines • May trigger frustration, anger, stress • Higher susceptibility to anxiety and depression • Personal, family, societal costs Impact • Increased medical expenses (physician visits and emergency care) • Caregiver burden • Risk of early nursing home placement Diagnosis •No definitive imaging techniques or biomarkers •Diagnosis relies on physical and neurological exam •Most common criteria: UK PD Society Brain Bank Classic Cardinal Symptom Tetrad Resting Tremor Bradykinesia Rigidity Postural Instability From: Chen/Fagan 2005 adapted from Gelb DJ, Oliver E, Gilman S. Arch Neurol 1999; 56:33-39. Diagnosis • Drug history—some drugs can cause side effects mistaken with early PD –Dopamine Receptor Blockers –Conventional & Atypical Antipsychotics (except clozapine) –Metoclopramide –Antiemetics (droperidol, prochlorperazine, promethazine) –Pimozide (Orap), amoxapine Diagnosis • Bradykinesia plus: – Rest tremor or rigidity • Unilateral onset • Insidious onset • Absence of early falls, dementia • Good response to dopamine • Unmistakable in advanced disease • Difficult to differentiate in early disease Scans • CT or MRIs • Assess damage to s. nigra in later stages of PD • Rule out tumors, strokes, other disorders: – Supranuclear Palsy – Shy-Dager Syndrome – Wilson’s Disease Self-Assessment Question One A definitive diagnosis of PD includes which of the following: A. A complete physical and neurological assessment B. A blood test C. MRI and CT scans D. All of the above E. A and C only Self-Assessment Question One A definitive diagnosis of PD includes which of the following: A. A complete physical and neurological assessment B. A blood test C. MRI and CT scans D. All of the above E. A and C only Things to look for… – Gait disturbances – Lack of manual dexterity – Reduced arm swing – Postural instability – Rigidity – Tremor Additional Motor/Non-Motor Features of Parkinson’s From: Chen et. al. JMCP 15:3:S1-21 PD Classification • Uses a 5-stage classification system • Called Hoehn and Yahr after creators • UPDRS is another system – Unified PD Rating Scale that measures mental functioning on a scale from 0 to 199 (total disability) – Used most in clinical trials Hoehn & Yahr Staging Stage 1: Unilateral disease Stage 2: Mild bilateral disease; good balance Stage 3: Mild/moderate bilateral; some postural instability; still independent Stage 4: Severe disability; Unable to function independently Stage 5: Wheel chair bound Hoehn MM, Yahr MD. Neurology 1967;17:427-442 Self-Assessment Question Two What is the most common means used to determine the stage of a person’s PD? A. Unified Parkinson Disease Rating Scale (UPDRS) B. Parkinson’s staging scale C. Hoehn and Yahr system D. DSM-IV Self-Assessment Question Two What is the most common means used to determine the stage of a person’s PD? A. Unified Parkinson Disease Rating Scale (UPDRS) B. Parkinson’s staging scale C. Hoehn and Yahr system D. DSM-IV Treatment Guidelines • • • • • American Academy of Neurology www.aan.org 2006 Neurology 2006;66:7:983-995 http://neurology.jwatch.org/cgi/content /full/2006/801/1 Recommendations From: Chen et. al. JMCP 15:3:S1-21 Quality Indicators for PD From: Chen et. al. JMCP 15:3:S1-21 Treatment Options • Dopamine precursor • Dopamine agonists • Preservation of dopamine in brain – COMT inhibitors – MAO-B inhibitors • Regulation of muscle movement – Anticholinergics Therapeutic Agents From: Chen et. al. JMCP 15:3:S1-21 Anticholinergics/Precursors • Benztropine (Cogentin) • Trihexyphenidyl (Apo-Trihex) • Procyclidine (DSC in US) • Carbidopa/Levadopa (Sinemet CR) COMT Inhibitors • Entacapone (Comtan) • Tolcapone (Tasmar) MAO-B Inhibitors • Rasagiline (Azilect) • Selegiline (Eldepryl, Emsam, Zelapar) Dopamine Receptor Agonists • • • • • Apomorphine (Apokyn) Bromocriptine (Parlodel) Pramipexole (Mirapex) Ropinirole (Requip) Rotigotine (Neupro, recalled in 4/2008) NMDA Receptor Inhibitor • Amantadine (Symmetrel) Symptomatic Treatment Substantia Nigra Selegiline Rasagiline Amantadine Levodopa BBB Dopamine agonists: apomorphine bromocriptine pergolide pramipexole ropinirole GABA DA ACh DDC COMT dopamine levodopa 3-OMD Carbidopa Striatum Trihexiphenidyl Benztropine Entacapone Tolcapone From Chen/Fagan 2005. Adapted from www.wemove.org Therapy: What is the Chief Complaint? Predominant Symptom No functional impairment Mild symptoms Mild-moderate sxs Discrete symptoms Motor fluctuations Clinical Options Neuroprotection (?) Amantadine, MAO-B inhibitor Dopamine agonist, levodopa Tremor—antimuscarinic Dyskinesias – amantadine Entacapone, apomorphine Surgery