* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download AH Renal I
Urethroplasty wikipedia , lookup
Kidney transplantation wikipedia , lookup
Kidney stone disease wikipedia , lookup
Urinary tract infection wikipedia , lookup
Chronic kidney disease wikipedia , lookup
IgA nephropathy wikipedia , lookup
Interstitial cystitis wikipedia , lookup
Autosomal dominant polycystic kidney disease wikipedia , lookup
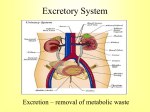
The Urinary System Primary Functions • In addition: 1. Regulates – Control BP volume & – Erythropoietin composition of – Activates Vitamin D extracellular – Regulates acid-base fluid (ECF) balance 2. Excrete waste Brief A&P Review • Macro: – Cortex – Medulla – Renal Pelvis Brief A&P Review • Micro – Nephron (Cortex) • Glomerulus • Bowman’s Capsule • Proximal & Distal Tubule – Nephron (Medulla) • Loop of Henle • Collecting Tubules Blood Supply • 2 Renal arteries off main aorta • 1200ml/min flows through kidneys ~25% of cardiac output Urine Formation • Filtration • Reabsorption – Tubules to capillaries • Secretion – Capillaries to tubules • Excretion • Glomerular Function – Selective Filtration – Semipermeable membrane – Hydrostatic pressure of the blood within the glomerular capillaries • GFR – Normal 125ml/min. – Only 1ml/min excreted due to reabsorption Ultrafiltrate • What passes through the glomerulus: – Is similar in composition to blood – But it lacks cells, platelets, and large plasma proteins – Normally: capillary pores are too small to allow the loss of these large blood components – Many renal diseases: capillary permeability is increased • permitting plasma proteins and blood cells to pass into the urine Tubular Function • Proximal tubule – Reabsorbs 80% of electrolytes & H2O – Reabsorbs all the glucose and amino acids, HCO3 – Secretion of H+ and Cr • Collecting Duct – Reabsorption of H2O • ADH required • Loop Of Henle – Reabsorption of Na+ and Cl- in ascending – Reabsorption of H20 in descending • Distal tubule – Secretion of K+, H+, Ammonia, – Reabsorption of H2O, (by ADH), HCO3, – Regulation of Ca++, PO4 (by PTH) – Regulation of Na+, K+ (by Aldosterone) ADH (Antidiuretic Hormone) • Makes distal tubules & collecting ducts permeable to H2O (reabsorption) • Without ADH (impermeable) • Any H2O left in the tubule will be excreted Aldosterone (from adrenal cortex) • Reabsorption of Na+ and H2O • In exchange for Na+, K+ ions are excreted • Secretion of Aldosterone is influenced by: – circulating blood volume – plasma concentrations of Na+ and K+ Acid-Base Regulation • Reabsorption of most of the HCO3 • Secreting excess H+ • pH 7.35-7.45 ANP (Atrial natriuretic peptide) • Hormone from Right Atrium – Response from atrial distention • Increases Na+ excretion • Inhibits renin, ADH, Angiotensin II – Thereby suppresses Aldosterone secretion • Results in large volume of dilute urine • Increases GFR Ca++ Balance • PTH secreted in response to low serum Ca++ • Increases reabsorption of Ca++ ions • Decreases reabsorption of PO4 Erythropoeitin • Produced in response to hypoxia and decreased renal flow • Stimulates bone marrow to produce more RBCs • Deficiency occurs in renal failure Vitamin D • Hormone obtained: 1. either in diet 2. or synthesized by ultraviolet radiation on cholesterol in the skin • These forms of Vitamin D are inactive – To become metabolically active: must be activated by the liver and the kidneys Renin • Regulates BP • Secreted by juxtaglomerular cells of kidney • In response to: – – – – – Decreased renal perfusion Decreased arterial blood pressure Decreased ECF Decreased Na+ ion concentration Increased urinary Na+ concentration Renin…how it works • Catalyzes the splitting of the plasma protein angiotensinogen (from the liver) • Converts it to Angiotensin I • Which is converted to Angiotensin II by ACE (Angiotensin-converting enzyme) • ACE is located in all blood vessels (and more concentrated in vessels in lungs) • Renin is inhibited when BP is up, plasma Na+ is up Diagnostic Studies • UA (0-trace protein) • Creatinine Clearance (24hr) – Approximates the GFR (Normal 85-135) • Serum BUN (10-30mg/dl) – Some non-renal factors for elevation: GI bleed, trauma, fever, infections, steroids, etc. • Serum Creatinine (0.5-1.5mg/dl – Best indicator of renal function – Higher in men (normal) Diagnostic Studies, cont… • • • • Serum K+ (3.5-5.0 mEq/l) Serum Ca++ (9-11 mg/dl) Serum Phosphorus (2.8-4.5 mg/dl) Bicarbonate (HCO3 22-26 mEq/L) Potentially Nephrotoxic Agents • Gent, Tobra, Ibuprofen, Contrast medium… The rest is just plumbing… • • • • Ureters Bladder Urethra Meatus ℞ for Break? Problems of Urinary Function Predisposing Factors For UTI’s • Urinary Stasis – Stones, urethral strictures, BPH, tumors, neurogenic bladder, renal impairment • Foreign Bodies – Calculi, catheters, ureteral stents, nephrostomy tubes, cystoscopy • Anatomic Factors – Congenital defects (eg shorter urethras, meatus in vagina), fistula formation, obesity Predisposing Factors, con’t… • Factors compromising immune response – Aging, HIV, DM, etc. • Functional Disorders – Constipation, voiding dysfunction • Pregnancy, low estrogen, multiple sex partners, spermicidal agents, diaphragm, poor hygiene Urinary Tract Infection Diagnostic Studies • Urine for c and s – Clean-catch sample preferred – Specimen by catheterization or suprapubic needle aspiration more accurate • Imaging studies – IVP or abdominal CT when obstruction suspected Causative Microorganisms • • • • • E. coli (80%)* Enterococcus Klebsiella Enterobacter Proteus • • • • Pseudomonas* Staphylococcus Serratia Candida * Nosocomial (31% of all NI are UTIs) Collaborative Care Drug Therapy • Antibiotics – Selected on empiric therapy or results of sensitivity testing – Uncomplicated cystitis • Short-term course (1 to 3 days) – Complicated UTIs • Requires longer-term treatment (7 to 14 days) Acute Pyelonephritis Inflammation of the renal parenchyma & collecting system Symptoms? • Sudden onset of chills, fever, vomiting, malaise, flank pain, dysuria, urgency, frequency…can lead to urosepsis (15% die) • Can subside within a few days, even if untreated, but bacteriuria and bacteremia persist Management • AB treatment • Fluids (8-10 glasses of water/day) • Rest • Pain control • Prevention Education Chronic Pyelonephritis • Characterized by small, atrophic, shrunken kidney r/t scarring or fibrosis • Decreased renal function • Leads to ESRD when both kidneys are involved (even if underlying infection is resolved) Urethritis • • • • • • • Trichomonas Monilial infection Chlamydia Trichomonas Gonorrhea Bubble baths Poor hygiene • • • • • Flagyl Clotrimazole Diflucan Doxycycline Mycostatin • Refrain from sex Interstitial Cystitis • Chronic painful inflammatory disease of the bladder • Characterized by urgency/frequency/pain – PBS (Painful Bladder Syndrome) (700,000 Americans) • Suprapubic pain in absence of UTI or other path. • Unknown etiology • Treatment: pain control, dietary/lifestyle changes to diminish voiding problems – Low acidic foods, no coffee, tea, carbonation, ETOH – Stress Reduction, antidepressants – May distill DMSO, Lidocaine into bladder DMSO (Dimethyl Sulfoxide) • DRUG INFORMATIONDMSO is a widely used treatment for interstitial cystitis (IC). It has both anti-inflammatory and analgesic properties. It is believed to inhibit freeradical production, thus reducing pain and inflammation. • It also aids in the absorption of other bladder-instilled medication. Its liquid form, Rimso-50, was approved by the FDA for use in treating IC in 1978. Oral and topical forms of DMSO have not been formally studied in the treatment of IC and should therefore be used with caution. INSTILLATIONSA 50% solution of DMSO is instilled intravesically, meaning that the drug is placed, via catheter, directly into the bladder. It is then held in the bladder for 10-20 minutes. This procedure is typically performed in a physician’s office. Renal TB • Usually 2ndary to Pulmonary TB • Asymptomatic (5-8yrs) • Then, low-grade fever, lesions ulcerate, infection spreads Glomerulonephritis • 3rd leading cause of renal failure – Affects BOTH kidneys equally – Can spread to tubules, interstitial, vascular areas • Divided into classifications: – Diffuse or focal – Initial causes: systemic lupus, systemic sclerosis or scleroderma, streptococcal infection, hepatitis, Goodpasture Syndrome, etc. – Extent of changes: minimal or widespread Glomerulonephritis, Symptoms • • • Hypertension/Edema? RBC’s, WBC’s, casts, and protein in urine Elevated serum BUN, Creatinine 1. Expect a full recovery in MOST acute cases (not with Goodpastures) 2. If progressive involvement…destruction of renal tissue and thus renal insufficiency Glomerulonephritis, Treatment • Prompt diagnosis • Correction of fluid overload, hypertension, uremia, inflammatory injury • Viral (fluids) • Bacterial (AB) • Autoimmune (corticosteroids, cytotoxic agents, plasmapheresis) Chronic Glomerulonephritis • • • • Acute Rapidly Progressive Chronic Mostly leads to ESRD Often found “by coincidence” Pt will have no recollection of nephritis hx • Diagnostics: Ultrasound, CT, Renal biopsy • Treatment: Supportive and Symptomatic Nephrotic Syndrome • Characterized by the glomerulus being excessively permeable to plasma protein • Thus tissue edema, ascites, anasarca (massive generalized edema) • Hypertension • Hyperlipidemia • Hypoalbuminemia • Hypercoagulability (thrombus usually forms in renal vein) Nursing Management • • • • • • Daily weights I&O Meticulous skin care Maintain a low to moderate protein diet Small frequent meals (pt often anorexic) Emotional support HIV and ESRD • 10% of HIV—highest among IV drug users Common Causes of Obstruction Obstruction complications • Hydroureter (reflux) • Hydronephrosis pyelo, atrophy • Nephrolithiasis (calculi) • The higher the pH—the less soluble are Ca++ PO3 • The lower the pH—the less soluble are uric acid & cystine Nutritional Therapy (Calculi) • Purine (Uric acid is a waste product of this) – Sardines, herring, mussels, liver, kidney, goose, venison, meat soups, sweetbreads • Calcium (Phosphate) – Dairy, all beans (except green beans), lentils, fish with fine bones (sardines, kippers, herring, salmon), dried fruits & nuts, chocolate • Oxalate (Calcium) – Dark roughage, spinach, rhubarb, asparagus, cabbage, tomatoes, beets, nuts, celery, parsley, chocolate, coffee, tea, Worcestershire sauce Renal Calculi • Diagnostics: U/A, C&S, IVP, Retrograde pyelogram, Ultrasound, Cystoscopy • Manage pain, treat infection, pass spontaneously (if < 4 mm), high fld intake (output at least 2 L/day) 1. Evaluation of cause, further prevention 2. Endo, Lithotripsy, Surgery = too large, unable to contain infection, impaired renal function, pain control, ineffective medical approach, pt with only 1 kidney Renal Vascular Problems • Renal Trauma (Symptomology) • Nephrosclerosis (BP control) • Renal Artery Stenosis (BP control, perfusion control, revascularization) • Renal Vein Thrombosis (anticoags, steroids, thrombectomy) Polycystic Kidney Disease • The most common life-threatening genetic disease in the world • 2 types (Childhood and Adult) • Adult type—50% chance of child having it. PKD Metabolic & Connective Tissue Diseases • Diabetic Nephropathy – Primary cause of ESRD – Microangiopathic changes, diffuse glomerulosclerosis • Gout – Hyperuricemia (deposits of uric acid crystals) • Amyloidosis – Infiltration of tissues with a hyaline substance (amyloid) • Systemic Lupus Erythematosus – Connective tissue disorder (similar to glomerulonephritis) • Systemic Sclerosis (Scleroderma) – Vascular lesions Cancer • Kidney Adenocarcinoma (Renal cell) most common type – – Will need nephrectomy, chemo Risk factors: smoking, genetics, obesity, hypertension, asbestos, cadmium, gasoline, polycystic disease • Bladder Transitional and Squamous cell (rad + chemo) 1. 2. 3. 4. – Transurethral Resection (with cauterization) Laser photocoagulation Open loop resection (snaring of polyp types of lesions) Partial or Radical Cystectomy (if invasive) Risk factors: Smoking, dyes, rubber industry, phenacetin-containing analgesics (1st NSAID) Urinary Incontinence and Retention • Types: – Stress – Urge – Overflow – Reflex – Trauma – Functional Catheters • Urethral • Ureteral (Cystoscopic or surgical placement) • Suprapubic • Nephrostomy Tubes Urinary Diversion Devices