* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download lklklklk - BC Centre for Epidemiologic and International Ophthalmology
Vision therapy wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Dry eye syndrome wikipedia , lookup
Corneal transplantation wikipedia , lookup
Visual impairment wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
PPO
OPPU
UL
LA
AT
TIIO
ON
NS
SUURRVVEEYY AANNDD
PPRRO
OG
GR
RA
AM
ME
EVVAALLUUAATTIIO
ON
NO
OFF T
TH
HE
EE
EYYEE C
CAARREE SSEERRVVIICCEESS IINN N
NEEPPAALL
N
NAARRAAYYAANNII &
&L
LUUM
MB
BIIN
NII
22000066
Principal Investigator:
Program Advisor:
Investigator:
Bio-statistician:
Study Ophthalmologist:
Dr Anil Shechan
Dr Ken Bassett, Dr Praveen Nirmalan, YD Sapkota,
Dr. Ram Prasad Pokhrel, Jaafar Aghajanian
RP Kandel, Dr Bal K. KC
Karthik Prakash
Dr Anil Sherchan, Dr. R.P.Shah
1. BACKGROUND
1
2. GOALS AND OBJECTIVES
2
2.1 Goal
2.2 Objectives
2
2
3. LOGISTICS
3
3.1 Infrastructure
3.2 Study Administration
3.3 Study staffing
A. Field Office Level
B. Field Level
3.4 Study co-ordination committee
3.5 Technical Advisory Committee
4. STUDY DESIGN
4.1 Introduction of Study area
4.2 Program Evaluation Methodology
4.3 Cost analysis
4.4 Sample Size
4.5 Sample population
4.6 Sampling Methodology
5. TRAINING AND PILOT STUDY
5.1 Training of Study Staff
5.2 Training of Enumeration Team:
5.3 Training of Ophthalmic Assistants
5.4 Training of Data Entry Staff, Data Manager/Bio-Statistician
5.5 Pre-Pilot Study and Pilot Study
5.5.1 Purposes of pre-Pilot Study are as follow:
5.5.2 Purpose of Pilot Study
6. SUMMARY OF FIELD PROCEDURE
6.1 Field Team Composition
6.2 Eye Examination Site Selections and Examination Procedure
6.3 Field Logistics
6.4 Barriers to up take a cataract surgery
6.5 Overall Study Schedule
6.6 List of Equipment and supplies
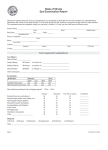
7. GUIDELINES FOR FILLING THE FORMS
7.1 Guidelines to fill Site Summary Form 1 (Enumeration team)
Village Details:
Survey Summary:
7.2 Guidelines to fill Household Form 2 (Enumerators)
7.3 Guidelines to fill Eye Examination Form3
Section A - Demographic information
3
3
3
3
4
4
4
5
5
5
5
6
6
6
7
7
7
8
8
9
9
9
9
10
11
12
13
13
14
15
15
15
15
16
17
17
Section B - Vision - This section is to be filled in by Ophthalmic Assistants.
Section C - Cataract Surgery History
Section D - Refraction with Retinoscopy
Section E - Basic Eye Examination
Section F - Intra ocular pressure
Section G - Anterior Chamber
Section H - Pupil dilation
Section I - Lens Status Lens:
Section J - Cataract surgery details
Section K - Fundus
Section L - Principal Cause for Low Vision or Blindness
Section M - Current Action Needed
Section N - Remarks
8. DATA ENTRY & MANAGEMENT
8.1 Data Collection:
8.2 Data Forms management:
8.3 Data Editing:
8.4 Data Entry & Quality Control:
8.5 Data consistency and validity:
8.6 Data Security
8.7 Data Storage
8.8 Data Analysis
8.8.1
Software:
8.8.2
Hardware requirement:
8.8 Overall Data Entry Flow:
9. QUALITY ASSURANCE
9.1 Inter & Intra observer agreement:
9.2 Quality Assurance in the field:
18
18
18
19
19
19
20
20
20
21
22
22
23
23
23
24
24
24
25
25
25
25
25
25
26
26
26
27
10. SERVICE DELIVERY & ETHICAL CONSIDERATIONS
28
ANNEXURE - A
29
ANNEXURE - B
30
ANNEXURE – C
31
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
1. BACKGROUND
Blindness and severe visual impairment remain leading causes of suffering and disability in the world. In
1995 World Health Organisation (WHO) made a global estimate that there are over 37 million persons
blind (bilateral blindness) and another 124 million persons with low vision who are at great risk of
becoming blind (Bulletin of world Health Organization;82:844 – 851), with ninety percent of them
distributed in the developing countries. It is estimated that over 0.84% (200,000 of the 25 million) of the
Nepalese are blind* of which over 70% are due to cataract (year 2005 projection). More than half of the
remaining 15% are also either preventable or curable with the available technology.
Prior to 1980, there were three ophthalmologists for a population of less than 14 million outside the
national capital Kathmandu, and only 16 hospital beds were dedicated to eye patients. In 1981, with
support from a wide variety of national and international organizations, a national program for the
prevention and control of blindness was established with the following three main objectives:
Achievement of national self-reliance in ophthalmic care
90% reduction in the prevalence of curable blindness
90% reduction in the prevalence of preventable blindness
The program was preceded by a national epidemiological sample survey, financed by the Netherlands
Government through the WHO voluntary fund for Health Promotion, aiming to determine the amount,
cause, and location of blindness.
*
Blindness as defined by the World Health Organization is visual acuity of less than 3/60 in better eye.
Different categories of blindness are outlined in Table 1:
Table 1
Socially blind
Economically blind
Unilaterally blind
Vision impaired
Normal
< 3/60 in best eyes
< 6/60 in best eye
< 6/60 in worst eye and > 6/60 in other eye
< 6/18 & > 6/60 in worst eye
> 6/18 in worst eye
From the results of the Nepal Blindness Survey 1981, it was estimated that there were more than
117,000 blind in both eyes (0.8%), over 233,000 blind in one eye (1.7%), and 260,000 with low vision;
92% of these blind resided in rural areas of the country; 80% of these blindness were avoidable
(preventable and curable) in the context of a blindness program.
Based on the survey result, specific program objectives were established, and accordingly Nepal began to
build the physical and human infrastructure necessary to address the problem. Primary, secondary, and
tertiary care facilities dedicated to the prevention and treatment of eye diseases were established in the
areas of the country with greatest need. The program simultaneously implemented a strategy for training
eye care professionals at all levels in the hospitals and in the clinics as they become operative. The efforts
of a wide range of international and national non-governmental organizations were solicited and
coordinated to implement this national strategy for reducing blindness. As a result, there are now over 120
ophthalmologists, assisted by 350 ophthalmic assistants and supporting administrative staff, working in the
country. 18 eye hospitals and 46 district eye clinics have been established. Mobile surgical eye camps have
served remote areas. Some of the eye hospitals have started self-reliance program charging fee for service
for those who can afford to pay.
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Netra Jyoti Sangh (NNJS), a Non Governmental Organization, has been responsible for the coordination
and implementation of the eye care programs in Nepal.
The major effort of the eye care programs in Nepal has been to address the problem of cataract blindness,
which accounts for 72% of all blindness. As a rule of thumb: the incidence of cataract in general
population is taken as 1 in 1000 population per year leading to blindness (WHO definition). The National
Program performed 167,000 cataract surgeries in 2005. Although, a significant portions of these patients
(70%) were from India.
Lumbini Rana Ambika Eye Hospital started in early 1984. The base eye hospital was established in
Bhairahawa along with district eye clinics. And it has been functioning fully in all five districts of the zone.
The 1995 Lumbini Survey concluded that the rate of blindness remained challengingly high: the cataract
surgery outcome was poor with 30% under 6/60, and surgical coverage was low, only 40%. Another
survey with similar protocol, conducted in a adjacent zone “Gandaki”, in 2005, showed a slight reduction
on prevalence of blindness, an increase in cataract surgical coverage within 35 km radius, and a better
visual outcome after cataract surgery, compared to the 1995 Lumbini survey. The challengingly high rate
of blindness could be the affect of increased life expectancy in cataract blind persons. The result of the
currently designed survey will be interesting, especially in comparison to the 1995 findings and the 2005
projection, in terms of the visual acuity, quality of services, and patient satisfaction.
Extensive community outreach such as screening camp, village health post visit, surgical eye camp, and
school health program have been conducted in targeted area extensively. In the year 2005 the hospital and
its community service able to render surgical service to 26,020 Nepalese, with 4,678 of them blind due to
cataract.
In the last twenty years, demographic and socio-economic factors in Nepal have been changing rapidly:
1) The population is aging and consequently, the proportion of persons above the age of fifty has been
increasing rapidly which has resulted in an increasing number of cases of age related blindness
requiring treatment.
2) Similarly the infant mortality rate has decreased from over 170 per thousand to less than 100.
3) The per Capita GNP has increased from US$ 160 to over 200.
This protocol and manual of operations for this survey is based on the experiences of similar studies in
Nepal, China, and India which was conducted in accordance with the World Health Organization (WHO)
Secretariate Committee on Research Involving Human Subject and Ethical Review Committee of Nepal
Netra Jyoti Sangh (National Society for prevention of Blindness of Nepal).
2. Goals and objectives
2.1 Goal
To evaluate the Eye Care program in Lumbini zone of Nepal with a strong focus on the cataract services.
2.2 Objectives
To estimate the prevalence of blindness with a strong focus on the cataract among those fifty years of
age or older
To investigate the cataract surgical coverage rate under the current eye care services
Page 2
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
To assess the outcome of surgical treatment, including visual acuity and intra and post surgery
complications
To evaluate the cost effectiveness of community outreach strategies
To identify issues related to the gender and blindness
To identify the barriers to uptake the cataract surgeries
To evaluate the current eye care programs
3. Logistics
3.1 Infrastructure
Lumbini Eye Institute (LEI), with the help of Seva Foundation USA/Seva Canada society will carry out the
study, including the fieldwork. It will also provide the clinical personnel, the space, and other necessary
infrastructure support. Some non-clinical study personnel would be hired specifically for this study. At
different levels, appropriate staff will be either hired by or deputed from LEI and will be provided specific
training as required.
3.2 Study Administration
The field Office, located at the LEI, Bhairahawa, will be provided for the duration of the study. The data
management will take place in this field office and in the SEVA office in Kathmandu.
The Principal Investigator, Dr Anil Shechan, would be responsible for the day to day operation and
management of the study. The Data Monitoring, Management and Analysis Committee would be
responsible for overall management of the data from entry to analysis of the study. This committee will
consist of the following members:
Program Advisor:
Dr Ken Bassett; Dr Praveen Nirmalan; Mr YD Sapkota, Mr Jaafar Aghajanian
Investigator:
Mr RP Kandel, Dr Bal K. KC
Bio-statistician:
Mr Karthik Prakash, YD Sapkota
3.3 Study staffing
A. Field Office Level
Title
Program Advisor:
Responsibility
preparation of the protocol and providing the necessary direction and
guidance
Principal Investigator:
coordination of all activities at the field office level including,
enumeration, clinical examination, data collection, and data entry.
Investigator:
Will work directly with the Program Director and will assist in developing
the field protocol; responsible for the recruitment, selection and training
of the different category of study staff; ensuring the availability of
required equipment and supplies; developing the schedules for various
activities, such as staff selection, training, pre-pilot, pilot, field work and
data analysis; assisting in the development of the forms, collection of data
and its analysis; responsible for the budgeting in terms of ensuring cash
flow, expenses and the accounting.
Bio-statistician/Data manager: ensuring accuracy in the entry, storage, cleaning, analysis, and security of
the data
Data Entry:
Will crosscheck and verify all the forms with the electronic version of the
data
Page 3
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
B. Field Level
The field staff will be organised as two enumeration teams and one clinical team:
Enumeration team (2teams)
Clinical Team:
Enumerator & Supervisor
1 (total 2)
Ophthalmologist
Enumerator/Mapper
2 (total 4)
Ophthalmic Assistant
Helper/Village volunteer
1 per site
Driver
The local volunteers will also assist during the clinical examination
1
2
1
The workflow and detailed logistics are described in Section 6. In order to achieve a higher response rate
among the female in the community, the enumeration and clinical teams will employ some female staff to
accommodate the needs of those women who may be unwilling to be examined or interviewed by male
staff.
3.4 Study co-ordination committee
The Coordinating Committee will work towards structuring the interactions and support among different
teams and components:
Program Advisor:
Dr Ken Bassett, Dr Praveen Nirmalan, Mr YD Sapkota, Mr Jaafar
Aghajani
Principal Investigator:
Dr Anil Sherchan
Investigator:
Mr. R.P Kandel, Dr Bal K KC
Bio-statistician:
Mr Karthik Prakash, YD Sapkota
Study Ophthalmologist (1):
Dr Anil Sherchan
Study Ophthalmologist (2)
Dr. R.P.Shah
3.5 Technical Advisory Committee
The Technical Advisory Committee will consist of the international experts who would study and approve
the protocol, monitor implementation, ensure the quality of the collected data, and assist with the analysis.
The members are Dr Ken Bassett, Dr Praveen Kumar Nirmalan, Mr YD Sapkota, Mr Karthik Prakash and
Mr. Jaafar Aghajani.
Page 4
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
4. Study design
4.1 Introduction of Study area
The study will be conducted in seven districts of Gulmi, Palpa, Argakhanchi, Rupendehi, Nawal, parashi,
and Chitawan, in Narayani and Lumbini zone of Nepal. These seven districts cover both terrain, such as
valleys, hills, mountains, and the plane areas. More than 90% of the in-country service recipients of LEI
and its eye care service network are from these districts.
KMMEH was established in 2003 and began its outreach programs. As a result, the primary eye care
facilities became more active, quality of care improved, and surgical rate increased. Currently there are
several eHealth facilities in this zone include a Medical College, one regional general hospital, seven
district hospitals, 10 Primary Health Centres, 68 health posts, and 447 sub health posts. There are three eye
hospitals in these two zones: in Bhairawa, in Chitawan, and in palpa. LEI’s satellite clinics are the only eye
care service providers in these areas.
4.2 Program Evaluation Methodology
Program evaluation methodology will be based on the original proposal; it will use the data collected in the
past three years; and it will have the following components:
Program quality
based on the assessment of the ongoing eye care programs and services
(e.g. the assessment of the cataract surgeries), patient satisfaction,
ongoing training of the administrative and the clinical staff, ongoing
collection of comprehensive data, and acceptance rate for surgery
compare to that of the survey program
Quantity (eye target)
Number of treated eyes during the survey
Cost as the budget sustainability
Cost effectiveness
Above components will be evaluated in relation to one another, so that for instance, cost effectiveness does
not negatively affect the quality of care.
4.3 Cost analysis
The cost-effectiveness of community ophthalmology strategies in the study area will be determined based
on the following components:
Baseline community ophthalmology featured in each district, buildings, equipments, staff, programs,
and their associated costs;
Annual yield of people utilizing eye care services by age and sex in each district or groups of
districts, for instance, comparing hills with plains in Chitwan and Narwal Parasi;
The actual or an estimate of the fees paid by people;
Compare overall cost of program delivery per person found annually, for instance, the cost of finding
a blind man or women of a certain age in certain area.
The service delivery during the survey is somewhat similar to that of during the regular screening camp,
except for some additional survey specific activities listed below:
1) The enumerator will go house to house and fill out the house detail form.
2) The people arriving at the survey camp are already filtered by the enumerator. Therefore, the
survey camp will have less but more serious cases where as in the regular eye camp any person
can show up.
3) The survey will follow a more scientific methodology, for instance the use of the slit lamp
4) The Ophthalmologist will visit the field. He will visit the disabled in their home
Page 5
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
5) The survey will have a more comprehensive data collection
6) The cost will differ in terms of the landscape, hills versus plain area.
There are additional costs associated with each of the survey specific activities listed above. Adding these
additional costs to the cost of the current regular eye camps will give us an estimate of the total cost per
case.
4.4 Sample Size
The following assumptions were made in calculating the sample size appropriate to estimate the
prevalence of cataract blindness in persons of age 50 years and over.
Estimated prevalence of cataract blindness (VA<6/60)
8% (p=0.08)
Confidence Interval
95% (Z=1.96)
Error bound (precision)
15% {= p (0.08) X error (15%) = 0.012}
The sample size formula to estimate prevalence with specified relative precision is N = z2 (1-p) p2
Substituting the values in the formula
N = (1. 96) 2 (1- 0.08) (0.08) = 1,963(0.012)2
In simple random sampling, the sample size is scattered across the population. Cluster sampling makes the
survey more practical and has the benefit of both reducing the cost of the survey as well as improving
response rate through better rapport in a cluster. It has a cost in terms of sampling inefficiency, which is
usually determined by design effect. In cluster sampling, the design effect is an indication of the variation
due to clustering. So the sample sizes have to be adjusted for the cluster design effect. It is estimated by
the ratio of the variance when cluster sampling is used to the variance when simple random sampling is
used. Based on the few surveys conducted so far, we have information on design effects for varying cluster
sizes. Considering average village sizes and operational factors a cluster size of 200 is appropriate with
an associated design effect of 2.0. Assuming a design effect of 2.0 for clusters of 200 and a response rate
of 85%:
Sample needed by cluster sampling (1,963 x 2.0 0.85)
4,619 persons of age 50
Rounding off the sample size required
5,000
The proportion of the population 50 in this area
12.75% (2001 census)
The total population (all ages) to be surveyed
39,216
Based on a cluster size of 850 to 1,700, the number of clusters required
32
4.5 Sample population
The demographic data of 2001 Census will become the frame of sampling design. Tables showing
population of each ward in the study area will be prepared.
4.6 Sampling Methodology
The selection of the study clusters will follow the following steps:
List the wards and their population based on the census estimates.
A) Identifying the areas that constitute the sampling frames: The target area must have minimum of 60,000
persons of age 50 while it is preferable that it would be less than 100,000. Thus the target area should
have a minimum population (all ages) of 800,000. This will constitute the sampling frame.
B) Create sampling clusters to yield about 175 (108 to 216) persons 50 years. Thus the total population
in the cluster will be between 850 and 1,700. The sampling clusters are to be created by grouping villages
with the less than 850 population, or subdividing villages with more than 1,700 population into segments
as A, B, C, etc. For example: two wards with the population of 800 and 750 will be combined into one
cluster for the purpose of sampling. Vice versa, a large ward of 6,000 will be subdivided into 4 clusters as
Page 6
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
A, B, C, and D. The actual geographic boundaries of these segments based on local layouts will be defined
only for such segments that are chosen.
C) 32 clusters will be selected using a simple random sampling of clusters. The principle is to ensure that
each village resident has an equal chance of being selected regardless of village size. One approach is to
proceed as follow: 1) Order the sample frames by geographic location of village or alphabetically; 2)
Generate random numbers between one and the total number of clusters until 25 clusters are selected
without replacement.
SR .no:
Format for building the sample frame:
Village/Ward Name
Population
5. Training and Pilot Study
5.1 Training of Study Staff
The primary investigator will hire and assign qualified applicants to the project teams at least one month
prior to the start date of the pilot study. Intensive training will be provided for two weeks which will
include the following:
Purpose of evaluation:
A briefing on the present eye care programs both in Nepal and in the study area;
A brief introduction to the previous surveys and their outcome in order to increase the teams’ awareness of
the magnitude of the major blinding conditions such as, cataract, glaucoma, and trachoma.
The outline of the goals of the program
Survey forms:
Survey questionnaires are discussed in detail. Why the question is being asked? How it will make
difference? All these points are discussed in detail question by question with the individuals who will be
responsible for the data collection.
Survey techniques:
Sociologist will be trained on how to approach and interview the subjects. Different types of customs will
be discussed and appropriate behaviour will be suggested.
5.2 Training of Enumeration Team:
The enumeration team is responsible for listing all the individuals above 50 years of age and ensuring that
they come to the central examination site. The enumeration gives the denominator, based on which many
of the results are computed. Hence accuracy of the survey depends largely on the complete account and
examination of the enumeration.
One member of each enumeration team will be responsible for mapping the cluster. The “mapper” will be
trained to map the clusters, outline the boundaries, and all the important landmarks _streets and houses.
The map will be used as a guide by the enumerators to ensure that all the households in all the clusters are
covered.
Page 7
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
The enumerators will be trained to enumerate all households in the area mapped by the mappers.
Additionally, since they will be making the first contact with the subjects during the survey process, they
will be also trained to build rapport and create an inviting and comfortable climate for the subjects.
The program Advisor and Co-Investigator will give this training with the support from a statistician who
has in depth expertise in the survey and enumeration methodologies. The training will be held for one
week in the institution and for one week in the field to ensure familiarity with field situations.
5.3 Training of Ophthalmic Assistants
The Ophthalmologist and the ophthalmic assistants will attend training sessions in the Eye Hospitals for
one week and in the field for an additional week, and will become familiar with the field activities. This
will be especially valuable to those who have not been exposed to the fieldwork before.
They will discuss the overall purpose and the details of the fieldwork; study the field action manual;
discuss the clinical examination form in detail. As part of the training, they will fill out the Eye
Examination Forms for fifty hospital outpatients in order to familiarize themselves with the form’s format
and content.
In addition to above discussions, ophthalmic assistants will be further trained on vision testing, in field
environment. Taking intra-ocular pressures using applanation tonometer, refraction, and dilating the pupils
are practiced on outpatients in the Hospital. Additional responsibilities in the field such as care and
maintenance of equipment will also be discussed in detail.
5.4 Training of Data Entry Staff, Data Manager/Bio-Statistician
A software developed by the Lions Aravind Institute of Community Ophthalmology (LAICO), Madurai,
India will be used for data entry, data cleaning and archiving. Intensive data entry training will be given to
the data entry staff by the exports that are currently using this software. The data entry staff will enter
dummy data for the practice purpose and refinement of their skills. This will reduce the data entry errors
when entering the Pre-pilot and Pilot study data. The Bio-Statistician should become familiar with all
aspects of Data management and data organisation to avoid data entry backlog.
Page 8
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
5.5 Pre-Pilot Study and Pilot Study
After training is completed, the Pre-Pilot Study will begin in a small village with a population of
approximately 500 to 750. Two days will be allotted for enumeration and two days for examination. Since
the main emphasis will be on training, the Pre-Pilot village will be chosen outside the study area.
After Pre-Pilot Study is complete, Pilot Study will begin in two clusters: one in the rural cluster and one in
the urban ward _if urban areas are also included. This will be done in the study district in two of the nonstudy wards and the cluster should be preferably be one that is divided from a large ward. Two days will
be allotted for enumeration and two days for examination in each site. The Ophthalmologist and the
Ophthalmic Assistants will conduct a quality assurance program during the Pilot survey.
All the field staff will participate in the Pre-Pilot Study and Pilot Study. In addition, the Program Director,
Dr Anil Sercher and the Program Manager, Mr. Kandel RP will observe the study and sort out any
difficulties and provide directions when necessary.
5.5.1 Purposes of pre-Pilot Study are as follow:
To test the entire survey procedure and to train the survey team
To test the instruments of measurements - forms & equipment
To test all the field procedures, arrangements and logistics involved in enumeration and eye examination
To get a feel for response rates and how it can be improved
To observe whether the training to enumerators, ophthalmic assistants, and ophthalmologist is adequate
To provide more practice to the field staff
To observe inter-observer reliability agreement among ophthalmic assistants in VA screening and
ophthalmologists on clinical findings and diagnosis
5.5.2 Purpose of Pilot Study
It is similar to that of the Pre-pilot study. The Pilot study is done incorporating the lessons learnt in the
Pre-pilot study. It also serves as the “dress rehearsal” for the main study and gives one more opportunity to
fine-tune the procedures.
The importance of training and standardisation can not be emphasised enough. It forms the foundation for
quality in data collection, efficiency in study implementation and getting the study done on schedule.
6. Summary of Field Procedure
The population-based survey in Lumbini and Narayani Zones of Nepal will be carried out in 32 clusters.
Each cluster will have approximately 175 persons who are 50 years or older. Data will be collected at
Cluster level (village/ward), household level and individual level. Quality assurance data in a prescribed
format will be collected at individual level.
A letter of introduction describing activities will be sent to the community and political leaders of Towns
and Villages prior to the visit. Necessary permissions from the concerned health authorities will be
obtained. A personal meeting between the community leaders and the enumeration supervisor will follow,
to describe the proposed survey and seek their co-operation. A central site will be identified _preferably
school, village offices, health post/sub-health station_ and permission will be obtained to use it on the
scheduled dates for eye examination of individuals 50 yrs from the selected cluster.
Page 9
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
A mapper will be part of the enumeration team whose primary responsibility will be to map the cluster
boundaries with details such as schools, temples, health centers, other land marks, streets, houses etc. The
map will then be given to the enumerators who will use this as a reference to check the households that
ensure that all the houses in the map have been enumerated. For larger villages the segmentation will be
done using the map and the segment labels will be assigned randomly. The first randomly selected segment
will be called as ‘A” the second “B” and so on. On completion of mapping the mapper will join the
enumeration team and assist in all their other activities.
At the household level, enumerators complete the household folder (Form No.2). All those 50 years will
be requested to come to the central site for examination by the ophthalmologist. Each household is given a
ticket with list of person’s 50 years and date and time for examination by the clinical team. For each
person 50 years, the person's identification data is filled in the Eye Examination Record (Section A of
Form-3) and is kept inside the household folder. At the end, the enumeration supervisor will fill the Survey
Summary details in Form-1.
Prior to the arrival of the clinical team, the enumeration team will prepare the central village site for eye
examination. The clinical team arrives on the day as per prior communication. All enumerated persons
50 years are tested for VA by the ophthalmic assistant and examined by ophthalmologist as per the
protocol and Eye Examination Record (Form No.3) is completed. Persons who don’t present themselves at
the central examination site in spite of repeated efforts will be visited in their homes towards the end of the
work in the site. All the forms will be checked and crosschecked by the other enumerators, and the
ophthalmologists to ensure that it is complete.
People outside the study area presenting with eye problem will also be examined and treated at the end,
after finishing the examination of enumerated persons.
6.1 Field Team Composition
There will be two enumeration teams and one clinical team as listed below:
Enumeration team (2teams)
Mapper
Enumerators
Helper/Village volunteer
(The volunteers will also help in
the eye examination)
1 (total 2)
2 (total 4)
1 per site
Clinical Team :
Ophthalmologist
Ophthalmic Assistant
Driver
1
2
1
Page 10
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
6.2 Eye Examination Site Selections and Examination Procedure
The enumeration team will select a suitable site within each ward/cluster for ophthalmic examination. A
location(s) will be selected preferably within an hour walk of their households. Arrangements for
examination space, queues, tables, benches, and a place for equipment, forms and medicines must also be
made. The enumerator will consult with the village/ward leader in deciding the venue.
An ideal examination site will have the following characteristics:
Equipped with electricity
A waiting area outside the building
Two doors to facilitate entry and exit
An examination room, dark enough for examination _with the use of curtains, and light enough for
record keeping
A room for ophthalmic assistants to provide ocular treatment as advised by the ophthalmologist, dilate
the eyes, perform refraction and other needed activities
The arrangement of each examination site will depend on the layout of the building, number of rooms, and
the furniture available. The sketch below will be taken as a guideline in preparing the site.
(3)
Visual Acuity
&
Refraction
(1)
Waiting Area
(2)
Registration
(5)
Eye Examination
(4)
Dilation
(7)
Referral
And
Record keeping
(6)
Treatment
Suggested Floor Plan for the Central Eye Examination Site in Each Cluster
The numbers in the diagram refer to the following stations:
(2) Registration: Enumerator identifies the person from the referral slip and verfies the age, name of
the head of the household against that in the Eye Examination Record (Form-3) in the household
folder. The household folder then is given to the participant, who then will proceed to the visual
acuity station. Those who will show up for examination without being belonged to the survey
cluster, will be asked to wait in a separate queue and examined later when the enumerated persons
presenting at the examination site have all been examined.
Page 11
(3)
(4)
(5)
(6)
(7)
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Visual acuity assessment & Refraction: The ophthalmic assistant determines the visual acuity by
using a back illuminated ETDRS chart at a distance of 4 meters. The details of this are given in
Chapter 8 on forms filling. The presenting VA is measured first and if the person wears glasses
then the VA is measured again without glasses. After this the ophthalmic assistant enquires and
checks if the person has had cataract surgery and examines both eyes by torchlight. Deep anterior
chamber, jet-black pupil, presence of IOL, iridodonesis are signs of cataract surgery. Slit lamp will
be used to confirm the cataract surgery when necessary. If the person has undergone cataract
surgery in either eye, the details as in section-C of the form 3 will be filled. After the visual acuity
and examination for cataract surgery, the ophthalmic assistant records it and sends the person to
refraction or to the ophthalmologist. All persons with presenting VA <6/18 and those operated for
cataract in either eye will be sent for refraction and the rest will proceed directly to the
ophthalmologist for a detailed eye examination. Refraction will be done on all patients with
presenting VA < 6/18 in either eye. Special care will be taken while refracting aphakics and
pseudophakics as the visual outcome in this group is of interest. Those who are blind due to
refractive error (presenting visual acuity < 6/60) and aphakics and psuedoaphakics are provided
free glasses (the actual details and modalities of when, where and how the glasses will be given
will be worked out later).
Dilation: Those with best corrected vision < 6/18 in either eye and not due to corneal causes, or
those suspected to have cataract, open angle glaucoma, retinal or disc abnormalities, will have
their pupil dilated for ophthalmoscopy and slit lamp examination. The ophthalmologist will use his
or her judgment as to whether to dilate the person.
Examination: The Ophthalmologist will perform basic examination using the slit lamp, torch light;
he carries out ophthalmoscope and fills out the form further.
Treatment: the ophthalmic assistant provides treatment for ocular illnesses as advised by
ophthalmologist.
Persons who have completed the examination leave the area. Those needing further treatment are
provided with an explanation and referral slip for treatment to Lumbini eye Institute, where those
with curable cataract and VA < 6/60 in either eye will be offered free surgery.
6.3 Field Logistics
The field staff will consist of two teams: Enumeration and clinical team. The enumeration team will do the
mapping, informing the village elders, enumerating the screened individuals and prepare a central
examination site. This is immediately followed by the clinical team examining the participants. There are
two days assigned for the enumeration team and two days for the clinical team. Two days are assigned for
these activities mainly to increase the response rate. During the two clinical days, the enumeration team
will stay and continue with the registration, assist the clinical team to ensure the orderly flow of and
mobilizing the enumerated persons to increase the response rate to the desired level. Therefore, for each
site the enumeration team will spend four days while the clinical team will spend two days. Since there are
two enumeration teams for the clinical team, with proper coordination and necessary arrangements, it will
be possible to cover three clusters per week, and the entire field work can be completed in about 12 weeks
giving allowance of festivals and monsoons which can slow down the work. The following table illustrates
the movement and activities of the field teams over a two-week period in which six clusters are completed.
Logistics planning and scheduling cluster visits will take into account local activities, such as marriages,
festivals, etc, and will ensure that the schedule timeline can be met. Midway through the survey there will
be a meeting to discuss and address issues that may arise.
Day
Enumeration Team 1
Enumeration Team 2
Clinical Team
1.
2.
Enumeration in cluster 10
Assist Clinical Team in cluster 9
(enumeration already done)
Eye examination in
cluster 9
Page 12
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Assist Clinical Team in cluster 10
Enumeration in cluster 11
Eye examination in
cluster 10
Enumeration in cluster 12
Assist Clinical Team in
Eye examination in
cluster 11
cluster 11
------ Rest Day -----Assist Clinical Team in cluster 12
Enumeration in cluster 13
Eye examination in
cluster 12
Enumeration in cluster 14
Assist Clinical Team in cluster 13
Eye examination in
cluster 13
Assist Clinical Team in cluster 14
Enumeration in cluster 15
Eye examination in
cluster 14
------ Rest Day ------
6.4 Barriers to up take a cataract surgery
Interview will be taking to all 32 clusters among the study population having VA < 6/60 due to cataract in
one or both eyes. Right after registration, refraction and visual acuity test will be done by the Ophthalmic
assistant, followed by a complete ocular examination by the Ophthalmologist. Those who are diagnosed as
blind due to cataract will be requesting for the interview. Structured questionnaire will be administered
either by the principal investigator or investigators.
For the qualitative data, sixteen focus group discussions will be organized. In each focus group there will
be 4-6 person with cataract blind (< 6/60 Vision due to cataract). These 4-6 persons will be invited for the
discussion. Separate room will be arranging for the discussion where they can share their feeling freely.
Tea/Coffee will be served during the focus group discussion. Interview guideline and guideline for the
focus group will be developed. Moderator and investigator will be facilitating the focus group discussion.
Tape recording, note taking will be done for the future references.
Patient satisfaction /visual function/ after surgery:
To learn more about the level of satisfaction, quality of life of the patient after surgery, and their over all
functional vision, a separate questionnaire will be administered. To assess the functional vision and quality
of life, Doctors Ellwein and Fletcher reviewed IND- VFQ 33 and NEI- VFQ 25 and prepared 20 items
visual functioning questionnaires. This VFQ-20 addresses the following dimensions of visual functioning:
general vision, distance vision, near vision, colour vision, role limitation, glare, light/dark adaptation,
ocular pain/discomfort, social functioning, mental well being and dependency. This questionnaire already
we received from Ellweing National Eye Institute.
6.5 Overall Study Schedule
Based on experience of the earlier studies the study is scheduled with the following timeline:
2)
Pre-survey activities:
4
weeks
Procurement, Staff appointment & Training
3)
4)
5)
Organization of Study office space
Training & Pre-pilot study
Data analysis & re-training
Pilot study
Data analysis & re-training
Printing of forms
Field Data Collection
1 week
1 week
12 weeks
Page 13
6)
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Data entry
Data cleaning, analysis & report writing
2 weeks
Total Study Duration
20 weeks
Proposed Study Schedule:
Months
Period
Activity
The actual start date of the study would depend on getting necessary approval and funding. The study
schedule will change accordingly. However, the duration of the entire study would be about 5.0 months
expecting that it would start on August 2006.
6.6 List of Equipment and supplies
Equipments:
Portable Slitlamp (Kowa)
Illuminated ETDRS chart
Direct Ophthalmoscope
Streak Retinoscope
Torch light
Trial set
Applanation Tonometer
Power Generator
BP Set
Stethoscope
Stapler
Computers, Printers & UPS
1
3
1
1
2
2
1
1
1
1
4
2
Medicines per site:
Antibiotic drops
Methyl cellulose drop
Pilocarpine 2"/0 drop
Tetracycline ointment
2% Fluorescein strips
Atropine drop
Tropicamide drop
Gentamicin 0.3% drop
Tab. Diamox
Xylocaine 4%
50 units
10 units
5 units
100 tubes
20 strips
5 units
5 bottles
30 units
20 tabs
1 bottle
Page 14
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Antibiotic tablet
100 tabs
Antidiarrhoeal tablets
100 tabs
Supplies
Cotton roll
Methylated Spirit 450 ml
Povidone Iodine 10 % (200 ML)
Soap
Hand Towel
1 roll
1 bottle
1 bottle
10 PCS
2 PCS
Any increase in the above or other items required but not listed above will be procured for use as and when
required. All medicine may not be used in one cluster so only the medicines used are replenished.
7. Guidelines for filling the forms
7.1 Guidelines to fill Site Summary Form 1 (Enumeration team)
There are two parts to the form: the village details; and the survey summary. The Enumerator will first fill
out the village details, by asking the village chairman or any other well-informed person, and then fill out
the survey summary, which will be checked by the Ophthalmologist.
Village Details:
The Enumerator time will enter the following information related to the village:
A) cluster name and cluster number from the list of the clusters.
B) most reliable estimate for the number of households in the village after doing necessary cross checks
C) total population, from the census book or from the village head
D) distance (in Km or in hours of walking) to the nearest motorable road where public transport is
available
E) health Facility: If available mark the "yes" box, if not the "No" box.
F) define the type of Health Facility:
1 = Primary Health Centre
2 = Health Sub-Centre
3 = Community Health Centre
4 = Private health facility - Doctor, clinic, hospital, nursing home, etc.
G) distance of the nearest Health facility (in KM or in hours of walking). If answer to item 5 is "no"
specify the type of nearest Health facility using the codes as in 5a.
H) distance to the nearest Eye Hospital/Clinic (in KM or in hours of walking). If one is available in the
cluster itself, mark the distance in KMs.
I) eye Camp details: If any eye camp has been conducted within one year mark the "Yes" box (7) and
give the distance in KM (7a) and the place where the eye camp was held (7b).
Survey Summary:
Cluster Summary:
Number of Forms:
Total Households:
Total enumerated:
Total number of forms for each category
Total number of households enumerated in the cluster. The households
where there are no persons aged 50 years will also be included.
Total number of the subjects above 50 years of age in the cluster.
Persons living or working away from their clusters for more than six
months will not be included. Persons living or working in the cluster for
less than six months will not be enumerated.
Page 15
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Total number of persons who are present in the village at the time of
examination and could have been examined.
Number of cases examined:
Total number of persons who underwent the eye examination.
Response Rate:
(Total examined x 100) / (Total enumerated).
Start Date:
Date on which the enumeration in the cluster started
Finish Date:
Date on which the eye examination was completed
Service Provided:
Consult the individual Eye Examination Records (Form-3) and
consolidate the service provided under different categories.
Total cases:
7.2 Guidelines to fill Household Form 2 (Enumerators)
Contact at the Household: There are two stages to the introduction of the survey to the household, although
you may find that they blend into a single stage. The first stage occurs at the doorstep and is somewhat
more formal and courteous than the other. The second stage is in the household after you have established
your identity and your reason for being there.
In the first stage, the person whom you talk to will probably be curious about you and the survey. Establish
your identity with your identification card to alleviate any anxiety that you are a stranger whom they do not
wish to speak to. Make the notebook you carry prominent as another symbol of your legitimacy.
The doorstep is not usually a convenient or a comfortable place to conduct an interview, although it may
be in some communities. Try to make the doorstep interview brief and move inside. You will be able to
convince the members of the household about the importance of their co-operation from inside the
household. Do not ask permission to enter since they may refuse quickly. Instead, state that you want to
move inside, as "I would like to come in and talk with you more about the survey." Assume that the
household members have time to be interviewed, but if they really do not have the time, arrange for
another time when you can return for an interview. Be firm, but polite during these introductory
conversations. Do not press too hard since we want their co-operation later.
Once inside the household, most people will be quite willing to be interviewed and only need a brief
explanation of what the survey is about and what they need to do. Although it may be a new experience for
them, their curiosity generally leads them to be receptive to answering the survey questions. Do not be too
specific about the nature of the questions, to avoid introducing bias into their answers. General remarks
such as "we are interested in finding out about the eye health of people who live here" will be sufficient.
Some people may be uncooperative or have some reasonable concerns about the survey. You must respond
in a positive and confident manner to their questions, always maintaining a courteous manner. Remember
that you are a stranger to them, probably of a different caste or tribe. Their concerns and questions are
legitimate and require your careful attention. The following are the instructions for filling out the
Household Form (Form No.2)
Cluster Name and No: Copy from the list of clusters.
Enumerators:
Fill in the name and ID number of the enumerator.
Household No:
Copy from the number written on the wall or door, which had been previously
painted by Enumerator Supervisor. A household unit will consist of a family who
shares food cooked in one kitchen. If the head of the household gives consent for
interview go ahead and complete the interview. If he refuses terminate the
interview. With proper introduction and permission of village elders, we expect
that this will happen very rarely.
Visit Date:
Record the date, month and year at each visit to the household.
Time:
Record the time of each visit.
Name:
Fill in the name of all person’s 50 years in the household.
Page 16
Age:
Other columns:
Wearing glasses:
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Enter completed years of age. If you have any suspicion regarding age of the
person list his name but further enquiries should be made. In such cases local
event calendar would be useful. E.g.: 2010 Year. You can ascertain if the person
was born before or after that year. All persons born before 2010 will be 50 years
of age and this is the age group of interest to us.
For other information such as relationship of Head of Household, Sex, Literacy,
Type of resident, Education and Occupation, details to be filled in as per the table
given below in Form 2.
At the time of filling the household form the enumerator observes whether the
person is wearing glasses or not, and enters the information in the corresponding
column. If the person is not present, they will enquire from the respondent if the
person normally wears glasses.
Details of Respondent:
Respondent:
Name, Age and sex of the respondent to be filled in.
Relationship to the Head of Household:
The relationship of the respondent is to be filled by entering in the box the
alphabet corresponding to wife, household member, the neighbor, or others.
7.3 Guidelines to fill Eye Examination Form3
All subjects are tested at the examination site. The Eye Examination Record comprises of twelve sections
as listed below:
A. Demographic (Name, ID and personal information)
B. Vision & details of cataract surgery if any
C. Cataract Surgery History
D. Refraction with Retinoscopy
E. Basic Eye Examination
F. Intra ocular Pressure
G. Anterior Chamber
H. Pupils dilatation
I. Lens Status
Cataract Surgery Details
K. Fundus
L. Causes for Low vision or blindness.
M. Current Action needed
N Remarks
Section A - Demographic information
Enumerators fill section-A at the time of enumeration for all person’s 50 years of age which includes the
following fields:
Name:
The name of the person to be examined
Cluster:
The serial number of the survey cluster, expressed in two digits. If the serial number is
"5", it should be filled as "05" in the box and not as "5 ".
HH:
The number of the household expressed in three digits with leading zeroes when the
number is less than 100. If the serial number of the household is " 5 ", "005 "should be
filled in the box. Start with "001 " for each cluster
Pers.No:
The serial number of the person as listed in the household Form-2.
Page 17
QA:
Age:
Sex:
Month:
Date:
Year:
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
This box has a number already filled in –1 for the first examination and 2 for the second
examination if performed for the purpose of quality assurance.
The age of the person to be examined to be expressed in number of years.
Gender of the person: 1 = Male, 2 = Female.
The month of clinical examination
The date of clinical examination
Four digits of the year (YYYY): 2000 instead of 00.
Section B - Vision - This section is to be filled in by Ophthalmic Assistants.
Ophthalmic Assistant ID:
Presenting vision:
Wearing glass:
Cannot be tested:
The ophthalmic assistant will enter the OA ID assigned to them after
entering the subjects’ vision information.
The ophthalmic assistant determines the visual acuity by using a back
illuminated ETDRS chart at a distance of 4 metres. Visual acuity is tested
separately for each eye (one at a time) using the person's usual distance
correction glasses, if any. Visual acuity is recorded as the smallest line read
with one or fewer errors. Those unable to read the largest line of the chart at
four meters will be asked to read the chart at 1 meter distance. If the person
is unable to read the largest letters in the chart even at 1 meter, then finger
counting is done at 1 meter for hand movements and light perception. Care
will be taken to ensure that the unexamined eye is adequately covered with
the palm or cloth and not pressed. For details of measuring VA using the
ETDRS, refer to Annexure - A.
Record 1 or 2 depending on whether the person is wearing glasses or not. If
person is wearing glasses the unaided vision is recorded. Whether the
person can be tested: In a dumb/deaf or mentally retarded person, it may not
be possible to record visual acuity. Hence record in box a value of 1 or 2.
1 = The visual acuity can't be tested;
2 = The visual acuity can be tested
In conditions where vision cannot be tested the ophthalmic assistant will
mark on the boxes "Cannot be tested". In such cases the ophthalmologist has
to make a subjective determination of visual acuity which can be done at the
end of examination, and record one of the three possible values listed below:
1 =Believed blind;
2=Believed not blind;
3=Undetermined
Section C - Cataract Surgery History
Did you have cataract surgery:
1 = No (did not have cataract surgery); 2 = Yes (had cataract surgery)
If Yes, record the place of surgery as given below:
1 = Govt. Hospital; 2 = Private & NGO hospital, 3 = Private Practitioner (operating in a clinic or
Nursing Home), 4 = Eye camp
Enter the month and the year in the space provided.
Use only numerals. E.g.: Jan 2000 should be recorded as 1/2000 and Name of Hospital/Camp:
For each eye, record the name of the hospital or the place of eye camp, in the space provided.
Section D - Refraction with Retinoscopy
The ophthalmic assistant will record subject’s ID in the box provided prior to refraction. All persons
whose presenting vision in either eye is < 6/19 and those with aphakia or psuedoaphakia in either eye
will undergo refraction. Special care is taken to refract aphakics and Pseudophakics using a retinoscope
Page 18
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
if necessary. Best corrected VA and the corresponding refraction values for each eye is noted down.
Refraction with dilation is not done at this moment. Presbyopic and those with vision 6/60 or better will
be given glass prescription if they request.
Section E - Basic Eye Examination
From this section onwards all the examination are to be carried out by Ophthalmologist, while
ophthalmic assistants could do IOP measurement and dilation. The ophthalmologist should enter their
ID number in the space provided before conducting the examination. The basic eye examination consists
of examination of eyelid, and globe and papillary reflex using torchlight slit lamp and ophthalmoscope.
The examination includes the determination of type of cataract surgery and any obvious surgical
complications. In the sections under "Eye lid & Globe" mark all the boxes that apply. The findings will
be marked as 1, 2 or 9 as the case may be, where 1 indicates the finding is not present, 2 indicates
present and 9 indicates undetermined cases
Defective eyelid Closure:
When a person is asked to close the eyes the upper and lower lid
should come in contact and globe is not visible But in cases of
lagophthalmos, ectropion, loss of lid margin, etc, the lid may not come
into apposition. In such conditions eye boxes adjacent to "Defective
closure" is to be marked.
Inturned margin/trichiasis:
Look at the lid margin by torchlight and note whether lashes are
touching the globe or not. If even one lash is touching the globe, then
mark the box adjacent to inturned margin/trichiasis. Evidence of recent
removal of lashes will also be coded as trichiasis.
Globe:
Conjunctiva, cornea and eyeball are examined externally with the help
of a torchlight and slit lamp.
Phthisical/disorganised/absent: Include staphyloma as a type of disorganised globe.
Conjunctivitis:
Red eye & discharge
Central Corneal Opacity:
Only if it is within the pupillary area or obstructs vision.
Corneal ulcer:
Mark if active ulcer is present. If corneal ulcer is suspected the ulcer is
stained with fluorescein and examined with blue light.
Pterygium:
If pterygium has progressed onto cornea, pterygium is marked. If not,
the box is marked as not present.
Other (specify):
If there is any other findings mark the box and describe in the space
provided. All corneal oedema / bullous keratopathy should be marked
in the cataract surgical complications. If the eye is not operated, then
include in this section.
Pupillary reflex:
Assess Pupillary Reflex and Mark 1, 2, 3 or 9 where 1 is reactive
pupil. 2 is sluggish pupil, 3 is non reactive pupil and 9 is
undetermined.
Section F - Intra ocular pressure
IOP measurement will be done by Ophthalmologist on persons who are suspected to have Glaucoma or
in those patients where the anterior chamber is shallow. Drops of 4% Xylocaine will be instilled in both
eyes and after five minutes, IOP will be measured using a Tonometer. If IOP is not done mark 1 in the
box and if done mark 2 in the box. Three measurements will be taken and the average will be recorded
within the boxes provided for each eye.
Section G - Anterior Chamber
AC Depth:
The depth of anterior chamber can be estimated both with oblique illumination and if in
doubt from the slitlamp appearance of the anterior chamber. In the technique described by
Page 19
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Van Herrick, et al, a thin slit beam is focussed on the cornea and anterior chamber, at and
perpendicular to the temporal limbus and the optical section is viewed at a 60 angle. The
AC depth is graded against the corneal thickness as “normal, shallow, deep and
undetermined”. The findings are categorised as 1, 2, 3 and 9, where 1 is normal depth, 2 is
shallow depth, 3 is deep chamber and 9 is undetermined. Any person who is suspected to
have glaucoma will be referred to the hospital for further examination.
Section H - Pupil dilation
Protocol for pupil dilatation for detail examination: Those whose vision does not improve to 6/19 or
better with refraction in either eye, and all aphakics and psuedoaphakics will have a detailed
examination of media and fundus after dilating the pupil. Also if the ophthalmologist suspects that
individuals whose vision 6/19 to have open angle glaucoma, retinal or disc abnormalities, their
pupils will also be dilated. Intra Ocular Pressure will be measured using Tonometer wherever possible.
Based on the results of the Intra ocular Pressure and after assessing the AC Depth, the individual will be
judged by the ophthalmologist to see if the pupil can be dilated for further examination. In cases where
obvious cataract (white, brown) can be confirmed by oblique light examination (with no red reflex) and
slitlamp, and anterior chamber is shallow, there may not be a need for dilation and this could also
prevent possible angle closure glaucoma.
Pupils are dilated using 1%. Tropicamide until a minimal pupillary diameter of 6 mm is achieved. In a
semi dark condition distant direct ophthalmoscopy is performed to examine the red reflex. After pupil
dilation, media (aqueous, lens, vitreous) and fundus are examined with the slit lamp and direct
ophthalmoscope.
If pupil was not dilated, record 1 in the box provided and if dilated record 2. Also record whether the
dilation was 6 mm. If no, mark 1 and if yes mark 2.
Section I - Lens Status Lens:
There are nine possibilities. Ophthalmologist determines the right one for each eye and enters the
corresponding code (1 to 9) in the appropriate box. The lens status is determined by distant direct
Ophthalmoscopy and Slit lamp. In case dilated examination is required, follow the protocol for dilation
as detailed under Section H. In a semi dark condition distant direct ophthalmoscopy is performed to
examine the red reflex. Ophthalmoscope is held at 50 cms from the person who is asked not to look
directly at the examiner (usually asked to look at distance slightly to the left or right) and red glow on
the pupillary area is examined. If the glow is bright, the lens is clear and cataract has not developed. If
the red reflex is present but reduced, early cataractous changes/posterior sub-capsular cataract may be
present. If there is no red reflex, one of the causes is cataract. In such cases, there is low vision or
blindness for which slit lamp examination and fundus examination by ophthalmoscope will be carried
out to rule out posterior segment pathology like vitreous haemorrhage or retinal detachment.
Section J - Cataract surgery details
Type of Cataract Surgery: The ophthalmologist will enter the type according to the following list:
1 = ICCE
2 = ICCE- AC IOL
3 = ECCE
4 = ECCE - AC IOL
Intra Capsular Cataract Extraction
Intra Capsular Cataract Extraction with Anterior
Chamber Intra-Ocular Lens Implant.
Extra Capsular Cataract Extraction
Extra Capsular Cataract Extraction with Anterior
Chamber Intra-Ocular Lens Implant
Page 20
Incision:
Iridectomy:
Complication:
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
5 = ECCE- PC IOL
Extra Capsular Cataract Extraction with
Posterior-Chamber Intra Ocular Lens Implant.
6 = Others (specify)
9 = Undetermined
The type of incision will be determined by the ophthalmologist as one of the
following, and the code number against it will be entered in the appropriate box.
1=
Corneal:
Obvious corneal scar is present anterior to
limbus.
2=
Corneoscleral/limbal: Scar is seen at limbus or posterior to limbus.
3=
Tunnel:
Tunnel Incision(SICS)
9=
Undetermined:
Cannot be distinguished.
The type of Iridectomy is to be determined by the ophthalmologist as one of the
following and the code number against it will be entered in the appropriate box.
1=
Peripheral:
Opening is visible peripherally.
2=
Sectoral:
Sectoral/complete Iridectomy is visible.
3=
None:
No Iridectomy is visible.
9=
Undetermined
If any of the following complications are found in the operated eye, the
ophthalmologist will mark, 1 not present, 2 if present and 9 undetermined as the
case may be. If the eye cannot be examined because of the complications, the
reason must be given.
Iris prolapse:
Vitreous in AC/Wound:
Corneal decompensation:
Pupillary capture by IOL:
Subluxated IOL:
Dislocated IOL:
CME:
Post-operative Glaucoma:
Uveitis:
Other (specify):
Iris is seen bulging or captured in the wound.
Many times in ICCE, even in uncomplicated
cases vitreous herniates through the pupil. If the
vitreous is touching cornea or captured in the
wound then only it will it be marked as
complication.
Cornea is oedematous, or bullae are seen on the
surface and it is hazy. If late, deep
vascularization might have occurred.
Pupil is distorted physically by IOL AC or PC
IOL is not in place but part of it is still visible
through undilated pupil.
IOL is not visible through undilated pupil.
Cystoid Macular Oedema due to intra
operative/postoperative reasons.
Increased intraocular pressure due to intraoperative/post-operative reasons.
Signs of uveitis: redness, keratic precipitates,
cells, flare, hypopyon. One or all may be present.
In this case specify any other complication,
which has not been listed
Section K - Fundus
The fundus examination is done using direct ophthalmoscope by the ophthalmologist in a dim room.
In cases of very dense cataracts, or if more detailed examination is necessary, the person will be referred
to the base hospital where indirect ophthalmoscopy can be performed.
Page 21
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
The fundus examination is marked as 1 if the lesion is not present, 2 if it is present, and 9 if
undetermined for either eye.
Normally in community screening, if the vision is 6/18 r better in the particular eye no further
examination is necessary. But as we are examining older population and we are collecting data for a
survey, the optic disc has to be examined by direct ophthalmoscope in all cases. If best corrected VA is
< 6/18in either eye, a dilated examination is to be performed if indicated by the ophthalmologist. Refer
to Section H for guidelines relating to pupil dilation.
Section L - Principal Cause for Low Vision or Blindness
Low vision is defined, as walking around vision is less than 6/19. Using the best judgment, the
Ophthalmologist will determine one cause for each eye thought to be the principal cause. The code
against this will be entered in the box provided. While diagnosing cataract, the lens opacity should
commensurate with the loss of vision.
Examples:
1.
If a person presents with glasses and his vision is 6/19 or better, no diagnoses should be marked.
His vision may be 6/60 without glasses
2.
Red glow is diminished, but his vision is 6/19 or better no cause to be marked.
3.
Red glow is diminished, presenting vision is 6/24, 6/60 or 3/60, but vision improves to 6/19 with
pinhole or refraction. Principal cause in such case is Refractive Error even if cataract is present.
4.
Glaucomatous cupping with cataract: If the lens opacity does not explain visual loss, then mark
GIaucoma. Same is the case in presence of maculopathy.
Only one condition has to be marked as the principal cause of low vision/blindness in either eye.
If there are any other contributory causes, record 1 and if yes, record 2 in the box provided. If yes, the
two main causes may be marked in the appropriate order as per the list given under principal causes.
Section M - Current Action Needed
This section relates mainly to the intervention necessary for the individual. If no action is needed, record
1 in the box provided. If action is needed, record 2 and also tick the appropriate boxes. Those who are <
6/60 because of high refractive error in either eye will be given glasses free of charge from the hospital,
and those who have vision > 6/60, glasses will be prescribed on request.
In the following cases make a referral to the hospital:
Cataract:
refer to the hospital for cataract surgery by providing a
referral slip. It is presumed that cataract surgery is marked
only if there is satisfactory light perception, accurate
projection of light and pupillary reflex. All patients with
visual acuity less than 6/60 in either eye and diagnosed with
cataract will be referred for cataract extraction surgery.
Eye lid surgery:
Refer to the hospital
Glaucoma surgery:
Refer to the hospital
For Posterior Capsule Opacification in Aphakes/Psuedoaphakes:
Refer to hospital for YAG laser.
For uncorrected Aphakia:
Provide the most suitable aphakic glasses.
Others:
Specify under remarks.
Indicate if further investigations or treatments are required while in the hospital
Page 22
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Section N - Remarks
Make diagrams of conditions not listed that you want to illustrate and write down description or
comments.
Ophthalmic Assistant Quality Assurance: Form No. 4
This form is to be filled for monitoring inter-observer agreement as part of quality control. This form
will be filled as per the guidelines given under section A, B, and D in Form 3. The pre-printed value of 2
in the box labeled A. In section-A indicates that this person needs to be examined by the second
ophthalmic assistant.
8. Data Entry & Management
In summary the following table shows the data collection system:
Form No:
Form Description
Respondent
Form No: 1
Cluster level form Based on secondary data and summary
of individual forms
Form No: 2
Household form
All the households from the sampled
cluster
Form No: 3
Eye Examination All individuals from the sampled cluster
record
with age 45yrs
Form No: 4
Quality assurance Individuals as per the protocol from the
5 randomly selected clusters for
ophthalmic assistant quality assurance
Person responsible
Enumerator
Enumerator
Ophthalmologist &
Ophthalmic Assistant
Ophthalmic assistants
8.1 Data Collection:
As per the study design and the data requirements, all the data will be collected in the field. There are four
different forms in total for data collection. Form 1 and 2 will be filled out by the enumerator at the end of
the data collection in a cluster. The clinical team will visit to the central site to examine all the enumerated
persons 45 years and the findings will be recorded in Form 3, Eye Examination Record. The ophthalmic
assistants will fill in the vision, intra ocular pressure and refraction data in Form 3; the rest will be filled in
by the ophthalmologist. In addition to the above three forms, there is a form 4, which is for inter observer
agreement between ophthalmic assistants as part of the quality assurance and will be administered only in
five randomly selected clusters.
Page 23
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
In summary the following table shows the data collection system:
Form
No:
1
Form Description
Respondent
Person responsible
Cluster level
Enumerator
2
Household
3
Eye Examination
4
Quality assurance
Based on secondary data
and
summary of individual forms
All the households from the sampled
cluster
All individuals from the sampled
cluster with age 45yrs
Individuals as per the protocol from
the 5 randomly selected clusters for
ophthalmic assistant quality assurance
Enumerator
Ophthalmologist &
Ophthalmic Assistant
Ophthalmic assistants
8.2 Data Forms management:
During the enumeration process, as each household is completed, the enumerator will do a quick check to
see that all data is collected and is accurate. Similarly during the eye examination at the central site also as
each person completes the eye exam, one of the enumeration staff assigned will check to ensure that allrelevant data has been collected. Missing data and mistakes are rectified after consultation with the
concerned person.
At the end of the day the data forms are checked again for completeness and accuracy by the team. When
the data collection at a survey cluster has been completed, the forms will be arranged for each cluster by
household number and person number. These will be well packed in the same sequence in a water proofed
plastic bag for transportation to the central office. In central office, the forms will be unpacked and
checked to ensure that all forms have been received as in the cluster summary form (Form-I) and will be
signed by the Data Manager.
8.3 Data Editing:
Before data entry, the forms will be edited and crosschecked for completeness and consistency. If the
forms are not filled completely, the concerned person will be consulted to fill in the missing data or clarify
the inconsistent data. It is recognized that this process is done with minimum time delay. Most of the
variables have the codes mentioned in the forms itself. However some of the fields (with descriptive data)
may require coding and this will be done after the entire data collection and entry is completed. All
changes and coding made either in the field or in the central office will be made in ink by crossing out the
original data and recording the new data beside it. It will be signed and dated by the person making the
changes. Over writing shall be avoided.
8.4 Data Entry & Quality Control:
The data entry centre will have access to at least one and ideally two computers preferably networked. One
is for data entry and another for archiving and analysis. A data entry clerk in Lumbini hospital will enter
the majority of the survey data into a custom designed data management program developed by the
Aravand team. It features programs for data entry, data cleaning and archiving. A complementary program
will be developed to enter the additional data. The data from both programs will be extracted into a
statistical software for the analysis. The data in the Aravand will be used for the subsequent long term
follow up as part of the patient records.
Page 24
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
8.5 Data consistency and validity:
A data entry operator enters the forms. At the time of entry the computer will flag any inconsistency and
corrections will be made after consultation with the persons collecting the data. Through range checks and
proper branching, the data entry software ensures to a large extent that there are no inconsistencies or
invalid data.
However the data now free of entry errors should still be checked for consistency. For example, a person
cannot have in the same eye a vision of 6/6 and the lens status as mature cataract with no red reflex.
Software has been developed for checking such inconsistencies. The software will create an error file with
relevant data such as the form identification, field names and the data. The data manager will then consult
the forms, resolve the inconsistency and enter the correct data. The corrected consistency error file will
then be electronically merged with the full database to give the corrected file. The above data cleaning
steps will be done as and when the data entry is complete for a cluster.
8.6 Data Security
Hardcopy:
In the field, patient records will be stored temporarily in metal cabinets that can be locked. In the
hospital, the data will be locked in a secure room in the hospital. The room is both fire and water proof.
Electronic:
All data will be on a secure server. The server is on site in the Lumbini hospital and it is backed up
daily. Access to data will be password protected and can be accessed only by the research team. Only
aggregated data will be presented to the outside research team.
8.7 Data Storage
After completing data entry for the day, the operator will take backup copy of the data in floppy or in pen
drive and he will keep 3 back-up sets at any point of time. The floppies/pen drive will be labeled by day of
the week form Monday to Sunday. The floppies marked “Monday” will be used to back-up data on
Mondays. The data in the main computer will be backed-up daily and there will at least 3 sets of back up at
any particular time. All the back-up files will be kept in a place different from the computer centre.
8.8 Data Analysis
The data will be entered into the Lumbini software for the most part. Additional software will be designed
to enter the additional fields. Entering the survey data in the Lumbini software will allow for the
longitudinal studies as well as the long term follow up of patients who will visit Lumbini hospital in the
coming years. The data can be easily imported into standard Statistical Packages such as SAS, SPSS,
STATA, for the analysis.
8.8.1
Software:
Details of the software, data organisation operations manual is given separately in the software manual.
Operating System : Windows 95, 98, ME, 2000 and XP.
8.8.2
Hardware requirement:
The following are the minimum requirements:
Processor
: Pentiums IV
RAM
: 128 MB
Floppy Drive
: 3.5" Drive
USB port
: for Hi Speed Pen drive
Page 25
Hard Disk
Number of systems
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
: 40 GB
: 2 Desktop
8.8 Overall Data Entry Flow:
Data
Collection
Data entry in
the field
in field
Site completed
Forms and
Floppy sent to
central office
Forms are
received in
central office
Validity and
consistency
checks and
correction
Data analysis
9. Quality Assurance
9.1 Inter & Intra observer agreement:
Assessing the consistency and inter-observer agreements of measurements is a central part of quality
assurance. While it may not be necessary or practical to do this on each and every variable it should be
done on all critical variables. The critical variables in clinical examination are as follow:
Ophthalmic Assistants: Visual acuity and refraction
Ophthalmologists:
Diagnosis of lens status
Diagnosis of Cause of low vision/blindness
As part of the training and standardisation the study ophthalmologists and a senior ophthalmologist
considered the gold standard will independently examine about hundred persons (fifty persons have
visual acuity 6/19, other fifty persons have visual acuity is < 6/19). One ophthalmologist does not
know what other ophthalmologist has diagnosed. The clinical forms will be then matched and analysed
using the Kappa statistic to see the inter observer agreement. Similarly the two ophthalmic assistants will
independently examine the visual acuity in about hundred persons (fifty persons have visual acuity
6/19, other fifty persons have visual acuity < 6/19). The inter-examiners repeatability will be analysed,
again using the Kappa statistic. These can be patients from the hospital itself and those in the pilot
studies.
In order to assess both inter and intra-observer variation data will be collected during training, pre pilot
and pilot studies. The data will be analysed and presented for review to the Technical Advisory
Committee.
Page 26
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
As part of quality assurance for the main study, five out of the 25 clusters selected for the main study,
will be randomly selected for inter observer agreement between ophthalmic assistants for visual acuity
and refraction. This data will be recorded in Form- 4. This data should be analysed for each of the
variables and presented as shown in the eg. below with the Kappa statistic.
Agreement between ophthalmic assistants on visual acuity assessment.
2nd Examiner
1st Examiner
<3/60
Total
6/19
6/60-<6/19
3/60- <6/60
6/19
6/60 - <6/19
3/60 - <6/60
<3/60
Total
9.2 Quality Assurance in the field:
While training and constant monitoring can achieve the desired quality in the study staff, a similar
approach has to be taken in the case of equipment’s used in the study. These will be of standard quality
and regularly maintained and calibrated.
Visual Acuity: In order to obtain consistent Visual Acuity, back illuminated ETDRS chart boxes will be
used. The distance between the chart and the person being examined must be measured by a tape and
marked for each site, each day.
Measuring Intra-Ocular Pressures: Applanation Tonometer will be used for this study.
3.
Slit lamp & Ophthalmoscope: Standard equipment with good optics and illumination will be used.
These will be checked and cleaned each day, as they will be used in rough conditions in the field.
9.3 Response rate:
The second aspect of quality in a field survey is the response rate. Higher the response rates more valid
the study becomes. This is a challenge when you recognise that a vast majority of the persons who are
required to come for examination will have normal vision. Results from studies with low response rates are
subject to a lot of speculation. Thus getting a high response rate of around 90% should be the aim. Some
of the strategies and steps to achieve this are:
Getting good co-operation from the village elders. Hence the time spent to describe the study and enlist the
support is very important and will be done taking into account the local leadership dynamics and other
factors.
The location of the central examination site and the examination timings must suit the villagers
At the examination site closely monitor who has come and who hasn’t. This can be done by checking the
name in the household folder as a person comes along. All the names not checked indicate non-attendance.
In addition to the enumerator and the village volunteer making frequent visits to bring in the patients, and
we will also elicit the help of neighbours who have come to the examination site.
9.4 Pilot Study
Another aspect of quality is adherence to the protocol. A lot of preparation is required to be able to adhere
to the protocol. This can be felt once the study enters the field where there are many uncertainties and
situations not under our control. If one goes to the field directly, then the first few sites will become the
learning ground and in most instances either the data collected will be unreliable or a lot of logistical
Page 27
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
difficulties would have been encountered. In order to avoid it, a Pilot study is necessary. Following this
time must be taken to formally review the data and the field procedures. In addition to this daily review
meeting in the early stage also helps in the smooth implementation of the study.
10. Service delivery & Ethical Considerations
This is a research project, it is important to meet the ethical considerations. When we come across a blind
person during the survey, it is important that necessary service is provided. Thus during the survey all
persons who are blind (VA < 6/60) in either eye should be thoroughly evaluated and appropriate action
should be taken or arranged. The following may be the causes and the corresponding action is indicated:
Cause of blindness (VA < 6/60) in either eye
Action
Cataract
Refractive error
Incurably blind in both eyes
Other reasons
Refer to hospital and provide free surgery
Provide spectacles free
Refer to rehabilitation services
Refer to hospital for more detailed examination and
further management
Extra efforts will need to be taken in the case of bi-laterally blind, by follow-up visits if necessary, to
ensure that they receive the required services. The following formats will be used for referring patients to
the hospital and for monitoring the service delivery.
For ethical considerations, the protocol will be reviewed and approved by Nepal Netra Jyoti Sangh and
Lumbini eye Institute.
Form for referring patients to an eye hospital for further management given in annex # C.
Page 28
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Annexure - A
The ETDRS (Early Treatment for Diabetic Retinopathy Study) E chart will be used to measure visual
acuity. This chart is made of non-reflective white polystyrene material and is installed in light box
illuminated by fluorescent tube lights. The chart is retro illuminated luminescence of 150 cd/m2 or greater.
This chart is placed at a distance of 4 meters from the measuring eye of the person. There are 5 letters (E)
in each row of the chart. The person undergoing the test must correctly recognize at least 4 letters in order
to get the score for the line. There are 14 (rows) lines in the chart but only the top 11 lines are used for
testing. Being able to read the 11th row from the top is considered as a normal VA of 6/6. This line
represents the minimum angle of resolution that a normal eye should have. When there is a need to test a
person from 1 meter only the top 6 lines are shown for the test and recorded in different fractions such as
1/60, 2/60, HM, FC, PL and NPL.
Room illumination: Ideally, the standard ambient room illumination for the VA screening room is 100
lux.
Distance: In ETDRS, the VA is measured at 4 meters and 1-meter distances. Hence in each examination
site, marking must be made on the floor indicating the position of the chart, 1meter and 4 meters from the
chart position. A chair is positioned from the person so that it is in perfect line with the center of the chart.
Person: Seat the person comfortably in the seat and explain the procedure. Measure the VA in one eye at a
time with the other eye covered. Start with the Right Eye. The other should be covered gently but not
pressed as it can affect the VA measurement of that eye. Please make sure that the person is not squeezing
the eye into a slit as it can produce a pinhole or slit effect.
Procedure: VA measurement is started from the top line (6/60) of the chart in order to familiarize the
person with the chart. If the person can see all the letters of the top line, then jump to the middle line
(6/30). If this line is also recognized correctly, then go to line 6/15 down to 6/6. One letter misread in the
line will be considered complete. If more than one letter is misread, then go up one line, if it happens
again. If a person is unable to read the top line at 4 meters, then move the person close to the 1-meter
position and repeat the test.
Recording the Visual Acuity: Against each line in the ETDRS chart, the visual acuity in different systems
is shown. Since the study is being done in India, following the local convention, “meter equivalent values”
will be used in the study. When measuring the vision from 4 meters, directly record the VA corresponding
to the last line read correctly (minimum of 4 out of 5 letters). If the measurement is done at 1 meter, use
only the top six lines, and depending on the last line read correctly, record the values as 1/60, 1/48, 1/38,
1/30, 1/24 or 1/19 where 1/60 corresponds to the top line and 1/19 corresponds for the 6th line. If a person
is unable to read the first line at 1 meter, perform tests like Finger Counting, Hand Movements, and
Perception of Light and record the findings as FC, HM, PL or NPL.
Page 29
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Annexure - B
Flowchart: Overall workflow in the eye examination site
Start
Presenting & Unaided
Visual Acuity Testing
Is s/he
Aphakic/Pseudophakic
No
No
Is
Presenting VA < 6/19 in
either eye?
Yes
Yes
Is s/he
Aphakic/Pseudophakic
Yes
No
Cataract Surgery
History
Refraction
Basic Eye Exam
IOP Measurement
Yes
Glaucoma Suspect?
No
Is BCVA < 6/19 or
Aphakia/Pseudophakia
Yes
Dilate (Both eyes?)
No
Type of Surgery
Yes
Lens Status
Aphakia/Pseudophakia
No
Details on Incision,
iridectomy and
Surgical Complications
Fundus Examination
Principal Causes of
Low Vision/Blindness
Follow-up
Treatment
Data
Entry
End
Page 30
2006 Population Survey and Program Evaluation of the Eye Care Services in Nepal
Annexure – C
Dear Dr.
for further management.
Referred to:
Patient Name:
Cluster Name:
I am referring the following patient to you
Age:
Cluster No:
Right Eye
Sex:
Household No:
Left Eye
Vision
Diagnosis
Notes on further action required:
Signature & Date
11.2 Format for monitoring service delivery - Cataract surgery:
Fill in details of those who are blind due to cataract (VA < 6/60) in either eye.
Blind eyes
Date
Sl.
Name
Cluster
HH
Referred
One
Both
Status
1.
2.
3.
4.
Under "Blind eyes” tick the column under “one” if unilaterally blind and the column “both” if
bilaterally blind.
11.3 Format for monitoring service delivery - Provision of free Spectacles:
Applies to only those who are blind in either eye due to refractive errors.
Sl.
Name
Cluster
HH
Date
prescribed
Date
Delivered
Signature
of Patient
1
2
3
4
11.4 Service Delivery budget:
Lumbini eye Institute will provides free service to those in need. Under this study patients with
visual acuity < 6/60 but improve with refractive correction will be provided spectacles free. Others who
require spectacles will only be prescribed. For persons advised and requiring cataract surgery, will be
taken to Lumbini eye Institute (Free Section) and operated free. Those requiring treatment and which can
be done at the examination site will be provided. Others needing treatment which cannot be provided at the
examination site or requiring further investigations, will be referred to the base hospital.
Page 31