* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Standard Precautions - Thalassemia Center
Survey
Document related concepts
Transcript
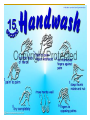
STANDARD PRECAUTIONS Infection Control TeamThalassemia Center -Dr. Maisam -SN Samar -SN Suhair INTRODUCTION: In the year 1990, the Centers for Disease Control & prevention (CDC) and Occupational Safety & Hospital Administration (OSHA) formulated new guidelines for Isolation precautions in Hospitals known as Standard Precautions. Definition: All blood and body fluids, secretions, excretions except sweat with or without visible blood are to be handled as infectious to blood borne pathogens regardless of the infectious state/ diagnosis of the patient. It also applies to non-intact skin and mucous membrane. Hand Hygiene: The hands of staff are the most common vehicle by which micro-organisms are transmitted between patients and hands. Remember: Hand washing is the Single most important measure in preventing the transmission of infection. Objective of Hand washing: Hand washing removes dirt, transient and some resident microorganisms as quickly and completely as possible, from hands, wrists and forearms. Definition: Hand washing – vigorous, brief rubbing together of all surfaces of the hands for 10 – 15 seconds. classified in two ways : v Mechanical removal of microorganisms by the use of basic soaps or detergents, to suspend the flora from the skin and allow them to be rinsed off. v Chemical removal of microorganisms by using anti microbial products to kill or inhibit the growth of microorganisms. Types of hand washing: v v v v Social Hand washing Hygienic hand washing or Antiseptic hand washing Surgical Hand washing Alcohol hand rub Efficacy of Hand Hygiene Preparations in Killing Bacteria Good Better Plain Soap Antimicrobial soap Best Alcohol-based hand rub CDC Bacterial Reduction Ability of Hand Hygiene Agents to Reduce Bacteria on Hands % 99.9 Time After Disinfection log 0 60 180 minutes 3.0 99.0 2.0 90.0 1.0 Alcohol-based handrub Antimicrobial soap (4% Chlorhexidine) 0.0 0.0 Baseline Plain soap Adapted from: Hosp Epidemiol Infect Control, 2nd Edition, 1999. Light patches indicate germs carried on the hands • Your hands carry many germs even if you can’t see them. • Many people don’t wash their hands because they look clean or because they are wearing gloves Alcohol Hand rub Solutions: Alcohol hand rubs can be applied more quickly (15 – 20 seconds) without the need for a hand wash basin and will remove both transient and resident bacteria. Should not be used if your hands are visibly soiled. Its useful during aseptic technique, outside isolation rooms, in intensive care settings where hands may need washing frequently and ,where access to hand washing facilities may be difficult. Ethyl Alcohol 62% moisturizer Vit E Personal Protective Equip. (PPE): Many excretions and secretions of the body are a major source of hospital acquired infections. Protective clothing should be worn for any direct contact with these body fluids. This helps to interrupt the transmission of microorganisms between patients and staff. Gloves: Gloves should be worn for any activity where blood and body fluid or substances may contaminate the hands Hands must be washed after removal because gloves may be punctured and your hands are easily contaminated as the gloves are taken off. To prevent transmission of infection gloves must be discarded after each procedure. Masks & Eye Protection: Eye protection and mask should be worn for any activity where there is a risk of body fluid splashing into the face. Gowns or Aprons: Since the front of the body is the part frequently contaminated by body fluid, plastic, disposable aprons provide adequate protection ,(e.g. dealing with body fluid spills,, dressing wounds). Gowns protect the skin of the health care worker from contamination by infected body fluid and reduce the risk of cross-infection to other patients via your clothing. Work practice controls : Refers to practical technique that reduce the likelihood of contamination by changing the way a task is performed. Proper Hand washing - Gloves Are Not A Substitute For Hand washing . Handling of used needles, & Contaminated sharps. One hand scoop method Retractable Needle Safety shield Work practice controls : Collection & laundering of soiled/contaminated linen. Collecting and transporting specimens Collection and disposal of waste Blood / Body Fluid Spill Management Care of Linen: Used linen is an infection risk for all those who are involved in its handling especially if it is contaminated with blood or body fluid substances. Render the linen “safe” by heat disinfection (usually the linen is thermally disinfected at the highest temperature the material will withstand 65º C for at least 10 minutes or 71 º C for at least 3 minutes). Waste Disposal: YELLOW BAG : For Disposing Pathological Wastes Blood and Body Fluids Catheters Wound Syringes IV Tubings /Sets IV Dressings Central Lines Gloves Dressings Suction Tubings Blood Transfusion sets Sealed Sharp Safe Boxes Redivac Drains Nasogastric Tubes Sanitary pads Soiled Diapers Secretions / Excretions Laboratory specimens Waste Disposal: BLACK BAG : For Disposing all types of General Wastes (non pathological wastes ): Papers Tissue papers Paper Towels Wrappers of hospital supplies Bottles Tin cans; Food wastes Communication Controls: Refers to information systems that reduce exposure to blood borne pathogens. Labeling and color marking of items or areas helps to communicate the potential hazards in the environment. Eg: Bio-hazardous labels to mark contaminated equipment. Engineering Controls: Sharp Safe containers Safe needle devices Needle less IV connectors Sharp injury Sharp Safe Policy: Used sharps should be handled as little as possible to minimize the risk of injury. Needles must not be re-sheathed. If a needle and syringe needs to be disassembled then it should first be re-sheathed using a single handed technique. Sharps must be discarded immediately after use into a designated sharps container. Sharps must never be carried in the hand to the point of disposal, but either carried in a tray or a sharps container brought to the point of use. They should not be passed by hand between staff. Needles should not be removed from syringes but discarded as a single unit. The bins must never be more than ¾ filled. Bins must be securely closed and labeled with the date, before being sent for disposal. What to do… In the Event of a Sharps Injury: Wash the area thoroughly with soap and water. Cover with a waterproof dressing. Inform your In Charge or Supervisor. Document the injury on an incident form. If known – note the details of the patient on whom the object has been used. Report to the Employee Health Department (staff clinic) or Emergency room. Conjunctiva/ Mucous Membrane: If splashed with blood/ body fluids irrigate with copious amounts of water; follow steps 4 – 6 above Concentration of HBV in Body Fluids High Blood Serum Wound exudates Moderate Semen Vaginal Fluid Saliva Low/Not Detectable Urine Feces Sweat Tears Breast Milk CDC Transmission based precautions: Air borne Droplet Contact Additional Precaution: NEUTROPENIC PRECAUTIONS Methods of transmission: Airborne route – this involves the transmission of infecting organisms in airborne droplet nuclei (5 nm or smaller in size) whose residue of evaporated droplets contained microorganisms remain suspended in the air for long periods of time, or dust particles containing the infectious agent (e.g. Mycobacterium tuberculosis and varicella virus). Droplet route – the infectious agent may come in contact with conjunctiva, nasal mucosa or the mouth of a susceptible host (e.g. Droplets are generated from the source person primarily during coughing, sneezing and during procedures such as suctioning and bronchoscopy). Contd….. Contact transmission – This is the most important and frequent means of transmission and can be sub-divided into the following groups: Direct Contact – direct physical transfer of organisms through direct personal contact (e.g. via hands). Indirect contact – contact of susceptible host with a contaminated object (e.g. contaminated equipment, instruments). Other routes of transmission: Vehicle transmission – this involves the transmission of infecting organisms via contaminated items (e.g. Food, water, medications). Vector borne transmission – the transmission of infection via insects (mosquitoes, rats, and other vermin). NEUTROPENIC PATIENTS: Immunocompromised patients vary in their susceptibility to hospital acquired infections, depending on the severity and duration of immunosuppression. Thalassemia Center policyHandling Patients Who Are Mildly Immunocompromised Post Bone Marrow Transplantation Environmental hygiene: Cleaning and disinfection of the environment: Concurrent cleaning – all surfaces should be cleaned using the approved disinfectant. Terminal cleaning – after discharge of the patient with infection, room should be disinfected using approved disinfectant. Blood spill kit and Mercury spill kit: These are available with the domestic staff and they are trained to use these kits. Environmental hygiene, contd: CSSD (central sterilization splay department): Items that undergo sterilization are sent to CSSD (situated outside the hospital complex). After the sterilization process the items are Packed and returned to the respective areas, ready for use. EMC (Equipment Maintenance Center): All equipments are sent to EMC for cleaning and disinfection . SINGLE PATIENT USE DEVICES Environmental hygiene, contd : Screening of water supply is done on weekly basis through Engineering Dept. Environmental screening is done as per schedule e.g. Air-conditioning. Screening and Immunization: New Employees: All new employees are screened by Staff Clinic for Hep B and HIV. Chest X-ray will be done to rule out pulmonary Tuberculosis. PREVENTION IS PRIMARY! Protect patients…protect healthcare personnel… promote quality healthcare!