* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Path Lecture 2: Disease of the Ureters, Bladder, and Urethra
Urinary tract infection wikipedia , lookup
Kidney transplantation wikipedia , lookup
Interstitial cystitis wikipedia , lookup
Chronic kidney disease wikipedia , lookup
Kidney stone disease wikipedia , lookup
IgA nephropathy wikipedia , lookup
Autosomal dominant polycystic kidney disease wikipedia , lookup
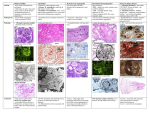
Path Lecture 2: Disease of the Ureters, Bladder, and Urethra Ureters o Congenital anomalies Ureteral duplication: most common anomaly of UT Ureterocele – a congenital saccular dilation of the terminal portion of the ureter and often assoc. w/complete ureteral duplication Inflammation o Ureteritis cystica Different names based on location Rare Morph: Von Brunn’s Nests Von Brunn’s Nests = solid nodules in transitional epithelium Imaging: multiple, small constant filling defects most numerous in upper ureter w/ “PUNCHED OUT DEFECTS IN LUMEN” Obstructive Lesions o Retroperitoneal fibrosis Define: extensive fibrosis throughout the retroperitoneum, often centered over the anterior surface of 4th and 5th LUMBAR VERTEBRAE Fibrosis entrapment & obstruction Men Most common cause = use of particular drugs Can be 2nd to malignant or infections or from sclerosing effects of radiation, or autoimmune Micro: fibroblastic proliferation & sclerosis and inflammatory cell infiltrate (+HLA-DR) Urinary Bladder o Congenital anomalies Bladder diverticula Mostly acquired b/c persistent urethral obstruction Can have urinary stasis infection & bladder calculi Extrophy Severe defect Define: anterior midline defect of abdominal wall, pelvis, UT, genitalia due to overall deficiency of mesoderm to infraumbilical region Epispadias – mildest. Urethra opens as groove on dorsal penis w/urinary incontinence Classic bladder extrophy – MOST COMMON. Bladder open to lower abd. Cloacal extrophy – omphalocele. Severe Risk of malignancy = 700 x higher for bladder carcinoma Inflammation o Acute & chronic Cystitis Most common UTI – E.coli! Risk factors for young women: hx of previous episodes of cystitis & frequent/recent sexual activity & use of spermicide use Risk factors for men: bladder outlet obstruction b/c prostatic hyperplasia, catheters Triad of ssx: lower abd. Pain, dysuria, micturition w/voids every 15-20 min Micro: Acute: stromal edema, hemorrhage, neutrophilic infiltrate Chronic: NO INFLAMMATION, mostly lymphocytes & fibrosis of lamina prop. o Painful Bladder Syndrome/Intestinal cystitis (PBS-IC) Define: suprapubic pain w/bladder filing assoc. w/increased urinary frequency in absence of proven UTI Female 40 yo Etiology: Infection, leaky urothelium (def. GAG layer), immunological response (SLE, Scleroderma, Sjogren w/most having anti-bladder Ab, ANA Ab), mast cell involvement Dx: cystoscopy w/overdistention Morph: ulcerative (Hunner ulcer = hallmark of classic cystitis), non-ulcerative (raspberry-like lesions) o Malacoplakia Define: rare granulomatous disease due to E.coli Middle aged women More common w/DM & immunocompromised Gross hematuria Etiology: E.coli w/impaired host defenses & defective phagocystosis MichaelisGutmann bodies Morph: soft, flat yellow-brown plaques or nodules, papillary lesions, hemorrhagic masses, necrotic ulcerations Micro: Von Hansemann cells(aggregates of granular histocytes) w/M-G bodies Urethra o Inflammation Urethritis Assoc. w/Reiter syndrome o Triad: arthritis, conjunctivitis, urethritis Urethral caruncle Define: inflammatory lesion that is small, red, painful mass at external urethral meatus Path Lecture 3: Cystic Diseases of the Kidney Cystic Kidney Diseases o Multicystic Renal Dysplasia Cause: persistence of abnormal structures in kidney Kidney enlarged, extremely irregular, multicystic Histo: flattened epithelium, islands of undiff. Mesenchyme, often w/cartilage and immature collecting ducts o ADPKD Most common inherited kidney disease One parent usually affected Basic defect is a disruption in the regulation of intracellular Ca levels due to mutation in the genes Morph: HALLMARK – massively enlarged kidneys caused by sustained expansion of innumerable fluid-filled cysts Surgical removal of cysts improves HTN Polycystic liver disease: MOST COMMON extrarenal manif. Vascular: berry aneurysms Cardiac: mitral valve prolapse Diverticular: colonic diverticulosis & diverticulitis o ARPKD MOST COMMON heritable cystic renal dz in infancy & childhood Parents unaffected Defect in PKDHD1 (fibrocystin/polyductin) ciliary dysfxn Morph: non-obstructive, B/L, symmetric dilation & elongation of renal collecting ducts and B/L enlargement of kidneys Pathogenesis: hyperplasia of epithelial change from absorptive to secretory Kidney & renal involvement Cystic Diseases of the Renal Medulla o Medullary Sponge Kidney Define: multiple cystic dilations of collecting ducts in medulla Renal fxn norm, found often incidentally Papillary ducts in medulla dilated o Nephrolithiasis – Medullary Cystic Kidney Dz Complex Define: inherited, B/L small cysts in medulla, usually concentrated at corticomedullary jxn Kidneys normal or small w/tubulointerstitial sclerosis ESRD Nephrolithiasis (NPH) AR Juvenile – (NPH1) o MOST COMMON FORM o Onset ESRD 13 yo Infantile (NPH2) o Onset ESRD 1-3 yo Adolescent (NPH3) o Onset ESRD 19 yo MCKD AD Presents 3rd-4th decades w/terminal renal failure in adult o Acquired (Dialysis-assoc) Kidney Disease Pts w/prolonged dialysis develop cortical & medullary cysts Cysts contain calcium oxalate crystals Most severe complication: RCC Path Lecture 4: Renal Calculi Hydronephrosis Urinary tract stones o Crystalline components and organic matrix o Calcareous stones – most Calcium oxalate = dark brown, jagged, extremely hard Calcium oxalate + calcium phosphate = dirty white, smooth, easily break o Struvite stones “infection stones” Magnesium ammonium phosphate o Uric Acid stones = yellow or pink Common in pts w/hyperuricemia o Crystaline stones Genetic defect in renal absorption of cysteine o Stone formation Supersaturation Urine pH o Acidic pH – cysteine, uric acid, calcium oxalate stone o Alkaline pH – calcium carbonate, calcium phosphate, magnesium phosphate stones Hypercalciuria: ex. Hyperparathyroidism Low urine citrate: calcium citrate acts as an inhibitor of crystallization Metastability Precipitation Crystal growth Crystal aggregation Nephrolithiasis o Hypercalciuric nephrolithiasis Idiopathic Renal hypercalciuria Hormonal hypercalciuria o Hyperuricosuric calcium nephrolithiasis >800 mg uric acid per day uricosuria + urine pH 5.5 calcium oxalate o Hyperoxaluric calcium nephrolithiasis Calcium oxalate insoluble & MOST COMMON chemical compound found in kidney stones o Hypocitraturic calcium nephrolithiasis Citrate is inhibitor of stone formation o Hypomagnesiuric calciumnephrolithiasis Mg & citrate important inhibitors of stone formation in UT o Uric Acid nephrolithiasis Caused by hyperuricemia and gout. Persistent acidic urine o Struvite nephrolithiasis UT infected w/proteus, klebsiella, or providentia (urease bacteria) NO E.COLI Staghorn calculi = upper UT stones that extend into at least 2 calices o Cysteine stones Rare, uncommon AR disease – cystinuria Bladder Stones “Vesicle Calculi” o Define: usually assoc. w/urinary stasis from bladder outlet obstruction o Men >50 yo w/enlarged prostates o Morph: struvite + calcium oxalate or calcium phosphate Urinary Tract Obstruction o Morph: possibly a gradually increasing dilation of the renal pelvis & an increase in weight & volume of kidney Weight increased b/c edema Dilation occurs 2-6 hrs post obstruction o Micro: changes in 1-2 mo Sclerotic glomeruli Apoptosis of tubule cells Edema & collage deposition in interstitium Path Lecture 5: Tubulointerstitial Nephritis Define: kidney diseases that involve renal structures outside glomerulus Biopsy req for dx MOST COMMON form: immunologic Most frequent causes: o Drug-induced o Infection-assoc. o Immune-mediated Ssx: renal failure, generalized hypersensitivity syndrome (triad = low grade fever, skin rash, arthralgias) Acute Tubulointerstitial Nephritis o Reactive interstitial nephritis Define: acute inflamm. Of renal interstitum during general infection (scarlet fev) Morph: enlarged kidneys No medulla involvement Clinical: transient acute renal failure, abnormal urinalysis Path: delayed type hypersensitivity or cytokines released during infection o Drug-induced Define: well-organized adverse rxn to drugs NSAIDs, SMX-TPM, PCNs, PPIs, H2 blockers, TZD, tetracycline, allopurinol Enlarged kidneys IF: fibrin in renal interstitium Clinical: transient renal failure, triad of allergic rxn (low-grade fever, skin rash, arthralgia), eosinophilia o Immunologically-mediated Anti-TBM Ab-mediated Autoimmune dz, Abs against tubular BM Linear IgG deposits along tubular BM Immune complex deposits on BM Granular immunoglobulin deposits T-lymphocyte-mediated Granulomas formed in renal interstitium Sarcoidosis Etiology: LUPUS MOST COMMON DZ Clinical: maculopapular rash, fever, eosinophilia, abrupt onset renal dysfxn Chronic Tubulointerstitial Nephritis o Define: common final response pattern of kidney to variety of insults o Clinical: HTN, or asymptomatic o Lab: increased Cr, decreased renal acid secretion/metabolic acidosis, excessive loss of substance in urine, mild proteinuria o Morph: tubular atrophy & dilation and hyalinized casts “thyroidization” Analgesic Nephropathy o Define: MOST COMMON category of chronic interstitial nephritis worldwide o Long-term phenacetin, aspirin, caffeine, phenacetin-acetaminophen, NSAIDs o Associated w/papillary necrosis o Clinical: HTN, renal insufficiency, papillary necrosis (gross hematuria & flank pain) o Kidneys slightly smaller o Cortex w/depressed areas overlying necrotic papillae NSAID Nephropathy o Adverse rxns of NSAIDs by inhibition of prostaglandins o Prostaglandins maintain renal blood flow and GFR o 15% of all cases of drug-induced renal failure Aristolochic Acid Nephropathy (AAN) o Define: rapidly progressive tubulointerstitial nephritis ESRD o Herb: aristolochia fangchi is cause o Proximal tubular cells main target o Shrunken, asymmetric kidneys o Cause of Balkan nephropathy Urate Nephropathy o Acute uric acid nephropathy: pts w/leukemia & lymphomas w/chemo o Chronic uric acid nephropathy: pts w/hyperuricemia & gout. Can induce chronic renal injury independent of crystal formation Hypercalcemia & Nephrocalcinosis o Define: calcification of renal parenchyma o Morph: purplish-blue tinge or stippling on H&E = calcifications Path Lecture 6: Acute Tubular Necrosis (ATN) Define: destruction of tubular epithelial cells & acute diminution of renal fxn Pts die b/c of serious involvement of other systems – NOT KIDNEY Acute renal failure o Pre-Renal ARF MOST COMMON FORM OF KIDNEY INJURY Adaptive to hypotension & volume depletion structurally fxn intact nephrons Oliguria & azotemia o Intra-Renal ARF Injury to kidney Acute tubular necrosis MOST COMMON FORM OF INTRARENAL ARF o Post-renal ARF Due to bladder outlet syndrome ATN occurs after ischemic or toxic event o Ischemic Hypoperfusion lasts for long time Pre-renal azotemia o Nephrotoxic Exogenous nephrotoxins ATN Aminoglycosides o Presents w/non-oliguric renal failure o 7-10 days post therapy Amphotericin B o Affects proximal tubule, medullary ascending loop of Henle, collecting ducts Radiographic contrast media o Non-oliguric renal failure o 24-48 hrs post Cyclosporine & tacrolimus o Decrease in dosage reverse renal insufficiency o Present w/HTN Acyclovir, Indinavir, Sulfa Drugs o Crystal formation Endogenous nephrotoxins ATN Myoglobinuria from rhabdomyolysis Hemoglobinuria from transfusion rxn Ischemic Acute Tubular Necrosis o Initiation o Maintenance Few days to several weeks Reduction in GFR, salt and water overload (edema), rising BUN & Cr o Recovery Regeneration of tubular epithelial cells Polyuria o Micro: tubular necrosis is patchy & affects single cells o Urinary Sediment Epithelial cell casts = MOST COMMON FORM Hyaline casts = tamm-horsfall mucoprotein solidified Granular casts Muddy brown casts = HALLMARK Toxic Acute Tubular Necrosis o Caused by dose-dependent toxic renal injury o Extensive tubular cell necrosis uniformly involving all nephrons o Casts present in collecting ducts w/extensive necrosis along proximal tubule segment at 3 days o 7 days = necrotic debris has disappeared from proximal tubules o 10 days = cells are regenerating, which mature at 15 days Path Lecture 7: Pyelonephritis Acute Pyelonephritis o Define: tubulointerstitial component of the kidneys affected o E.coli o Female o Ascending infection: MOST COMMON cause of clinical pyelonephritis o Morph: kidneys enlarged, red-congested w/yellow areas of focal abscess formation. Renal papillae are flat or diffusely blunted o Micro: areas of inflammation are well circumscribed & separated y zones of parenchyma that are fine. Abscesses form in cortex w/destruction of all the renal parenchymal elements in their center Acute Non-Complicated Pyelonephritis o By 3 weeks, interstitial fibrosis develops & scar contraction is evident in kidney poles o Lab: Pyuria, white cell casts, nitrite tests o E.coli most common, Klesbiella 2nd Acute Complicated Pyelonephritis o XGP Rare, serious complication characterized by an infectious renal phegmon Immunocompromised w/assoc. urolithiasis, UTI, DM Histo: lipid-laden macs E.coli or Proteus infection o Emphysematous pyelonephritis (EPN) Severe necrotizing infection causes gas formation Common in DM o Pyonephros = pus o Papillary necrosis Coagulative necrosis of renal medullary pyramids & papillae DM and persons w/UT obstructions Pyramids have white or yellow necrosis Chronic Pyelonephritis o Define: chronic interstitial inflammation induced by recurrent or persistent pyelonephritis o Often in pts w/major anatomic anomalies that keep infection alive o Major cause of ESRD throughout the world o Female and more often in infants and young children o Classification: Chronic non-obstructive pyelonephritis MOST COMMON SUBTYPE Pts w/VUR Chronic obstructive pyelonephritis Old male w/bladder stones, BPH, or carcinoma of prostate Women complication of cervical & endometrial carcinoma o Morph: coarse segmental scarring of kidneys, diffuse pelvicaliceal dilation & parenchymal thinning o Dx: intravenous urography Path Lecture 8: Amyloidosis Stains w/congo red that is orange brick in light and apple green birefringence (B-sheets of amyloid) in polarized light AL Amyloidosis – txt w/chemo o MOST COMMON FORM OF AMYLOIDOSIS IN US & EU o All patients have plasma cell dyscrasia Multiple myeloma (MM) Malignant plasma cells in bone marrow producing M protein Monoclonal gammopathies of undetermined significance (MGUS) Monoclonal Ig (M grotein) in serum or urine in persons w/out myeloma Lamda chains o Clinical: amyloid deposition in virtually every system BUT CNS, fatigue & weight loss Renal amyloidosis Cardiac amyloidosis – rt sided heart failure Peripheral amyloid neuropathy – spinal nerves GI amyloidosis – constipation or constipation/diarrhea Others – easy bruising – “raccoon eyes” o Always progressive AA Amyloidosis – txt by controlling underlying inflammatory dz o MOST COMMON form of systemic amyloidosis worldwide o Fibrils composed of serum amyloid A (SAA) which is secreted during acute inflammation Liver major site synthesis o Clinical: Liver & spleen where amyloid A FIRST deposits BUT kidney is common clinical presentation RACCOON EYES, ORTHOSTATIC HTN = NOT FEATURES ATTR Amyloidosis o Senile systemic amyloidosis (SSA) – affects elderly o Deposition of amyloid mainly in heart of TTR molecules o Dx: TTR B2M Amyloidosis o Hemodialysis assoc. o Clinical: osteoarticular sites Hereditary Systemic Amyloidosis o Familal Mediterranean Fever = periodic disease – txt w/colchicine Brief episodes of peritonitis, pleuritis, and arthritis assoc. w/fever MEVF gene codes for pyrin or marenostrin (AR) o Familial Amyloidotic Polyneuropathy – txt w/liver transplant Liver produces mutated TTR & affects peripheral nerves Diagnosis of Amyloidosis o Renal & hepatic biopsy – high positive yield in most forms of systemic amyloidosis o Recta mucosa – biopsy site of choice Path Lecture 9: Renal Vascular Disorders Benign Nephrosclerosis o Define: focal ischemia of parenchyma from sclerosis of renal arterioles & small aa. o Older blacks o Can be w/out HTN, but HTN & DM = increased incidence & severity o Medial & intimal thickening & hyaline deposition in arterioles o Normal or moderately decreased kidney size o Cortical surface: resembles grain leather o Micro: hyaline arteriosclerosis – patchy ischemic atrophy Malignant HTN Nephrosclerosis o Younger AA men o Hyperplastic arteriosclerosis & increased levels of angiotensin & renin = TYPICAL o Morph: “flea-bitten” appearance b/c of pinpoint petechial hemorrhages o Micro: fibrinoid necrosis of arterioles & onion-skin lesion of arterioles o Clinical: HTN, papilledma, retinal hemorrhage, encephalopathy, CV abnormalities, renal failure Renal Artery Stenosis (RAS) o Potentially curable form of HTN w/surgical txt o Atherosclerotic RAS = MOST COMMON CAUSE OF RENO-VASCULAR HTN Important cause of chronic renal insufficiency & ESRD Proximal 1/3 of main renal artery Older men o Fibromuscular Dysplasia (FMD) Deformation in renal artery wall stenosis Younger women NO INFLAMMATION Thickening of arterial wall occurs Distal 2/3 of artery = string of beads o Kidneys small w/signs of diffuse ischemic atrophy Atheroembolic Renal Disease o Emboli are cholesterol crystals appearing as rhomboid clefts Sickle cell disease nephropathy o Hematuria & hypothenuria (decreased ability to concentrate) Diffuse Cortical Necrosis o Most often after an obstetric emergency o Massive ischemic necrosis limited to cortex o Clinical: sudden anuria, terminating rapidly in uremic death Renal Infarcts o Result of embolized thrombi often from MI o Most renal infarcts are of the “white” anemic variety Path Lecture 10: Tumors of the Kidney Benign tumors of the kidney o Renal papillary adenoma Epithelial lesions of the renal cortex w/a tubular/papillary architecture Small, solid, well circumscribed, yellow-tan tumors in cortex o Angiomyolipoma Varying components of blood vessels, smooth m., and adipose tissue Pts w/tuberus sclerosis could get this in teens o Oncocytoma Cells w/granular & acidophilic cytoplasm – eosinophilia due to abundant mito Men >50 yo Mahogany brown w/central steallate scar Differentiate from RCC which is yellow-orange Malignant Tumors o RCC Large cells w/clear to granular cytoplasm & prominent vasculature MOST COMMON CANCER OF KIDNEY Smoking, obesity, HTN, enviro & occupational, acquired renal cystic disease w/ESRD Inherited forms: RCCa related to von Hippel-Lindau disease o Predisposition to retinal & cerebellar hemangiomas, clear cell renal carcinomas, and pheochromocytomas RCCa Tumor Types Clear Cell carcinoma o MOST COMMON TYPE o Loss of VHL on chromosome 3 Papillary carcinoma o From distal collecting tubule o Assoc. w/pts on chronic hemodialysis o Tan brown cut surface, Psammoma bodies might be there Chromophobe renal cell carcinoma o Pale eosinophilic cells w/perinuclear halos arranged in a solid sheet o Plant-cell like Carcinoma of the collecting ducts of Bellini o Arises in medulla o Nests of malignant tumor cells mixed w/fibrotic stroma w/in medulla Renal medullary carcinoma o Associated w/sickle cell Wilms Tumor (Nephroblastoma) o Ped malignant from metanephric blastema o MOST COMMON TYPE OF RENAL MALIGNANCY IN KIDS o Nephrogenic rests are precursor lesions o Hereditary forms: WAGR syndrome Denys-Drash syndrome – WT1 mutation Beckwith-Wiedmann syndrome – WT2 mutation o Solitary mass tan to tan-gray Path Lecture 11: Tumors of the Urothelium Benign Proliferative Urothelial Lesions o Urothelial hyperplasia Marked thickened urothelium w/o cytologic atypia NO MALIGNANCY o Von Brunn Nests Bulbous invaginations of surface urothelium encroaching into lamina propria o Pyelitis, Ureteritis, Cystitis Cystica Von Brunn nests develop central lumen Pyelitis – in kidney Ureteritis – in ureter Cystitis cystica – in bladder & associated w/bladder carcinoma o Squamous metaplasia Reactive process w/replacement of urothelial lining by squamous epithelium o Neurogenic Adenoma Males Clustered small papillae assoc. w/small multiple tubule structures + Pax-2 transcription factor Chronic infection Epithelial Tumors of Urinary Bladder o In Africa, increased b/c of Schistosoma hematobium o Whites mostly in urban o Papillary lesions – red & elevated o Flat lesions – carcinomas extending along bladder surface. Multiple, red, velvety, flat patches only mucosal surface = carcinoma in situ o Urothelial papilloma – men >50 yo o Urothelial carcinoma in situ – flat, non-invasive tumor all layers of urothelium Multiple red, velvety, flat patches confined to mucosal surface = CIS o Papillary urothelial neoplasms of low malignancy potential (PUNLMP) Can’t invade or metastasize o Low grade urothelial carcinoma Papillary low grade urothelial carcinoma Sea anemones o High grade urothelial carcinoma Malignant neoplasm often invasive Epithelium of varying thickness Non-Urothelial Carcinomas of the Bladder o Squamous cell carcinoma Common in countries w/urinary schistosomiasis Squamous differentiation resembling epidermis o Adenocarcinoma Glandular differentiation Mucin-secreting & trigone area Mesenchymal (Soft tissue) tumors of the bladder o Benign tumors MC – leiomyoma o Sarcomas Rhabdomyosarcoma – resembles skeletal m. features MOST COMMON MALIGNANT BLADDER TUMOR IN KIDS Bladder trigone Leiomyosarcoma Malignant smooth muscle tumor MOST COMMON SARCOMA OF BLADDER IN ADULTS Dome of bladder & lateral wall Seen after txt w/cyclophosphamide