* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download rajiv gandhi university of health sciences, karnataka
Survey
Document related concepts
Transcript
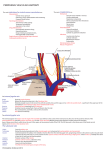
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE ANNEXURE-II 6. BRIEF RESUME OF THE INTENDED WORK 6.1 NEED FOR STUDY: The word "jugular" refers to the throat or neck. It derives from the Latin "jugulum" meaning throat or collarbone and the Latin "jugum" meaning yoke. Veins of neck are superficial or deep to deep fascia, and are not entirely separate. The external jugular vein forms part of the superficial venous system of the head and neck. With its tributaries it drains the superficial structures of the face, scalp and posterolateral neck. The internal jugular vein is part of the deep venous system of the head and neck. Internal jugular vein is a large vein collecting blood from skull, brain, superficial parts of face and much of neck. It begins at the cranial base, descends in the carotid sheath and terminates posterior to the sternal end of clavicle by uniting with the subclavian vein to form brachiocephalic vein. Its inferior bulb, dilatation near its end, is in the depression between the sternal and clavicular heads of the sternocleidomastoid, the lesser supraclavicular fossa, where a needle can be inserted with precision in the living subject.1 Various anomalies of the internal jugular vein have been reported. The studies have made possible the correlation of these anomalies with disorders in the ontogenetic development of the veins of the neck.2 In its course, it descends vertically applied to lateral side of internal and common carotid artery, enclosed with them and vagus nerve in the carotid sheath. It may course lateral, in front of (overriding) and rarely medial to common carotid artery.3 The vein may be rudimentary, its blood return taken over by the external jugular vein. The external jugular vein crosses obliquely superficial to sternocleidomastoid, and ends in subclavian vein.1 It has been proved that a large external jugular vein is associated with a small internal jugular vein. The two veins may communicate directly in the upper neck or indirectly, via emissary veins which link the superficial and deep systems. It is therefore feasible that blood that normally passes through one system may be diverted through the other causing the diameters of these vessels to vary inversely with each other.4 Rarely, the internal jugular vein receives tributaries like bronchial, vertebral, suprascapular and transverse cervical veins. Rare anomalies like bilateral duplication of the internal jugular veins have also been reported.5 Internal jugular vein is often chosen by clinicians and anesthetists for central venous access because the landmarks are easily identifiable. It also offers higher success rate with fewer complications, when done with a thorough knowledge of its anatomy, variations and anomalies. Knowing all the morphological variants of the course of head and neck veins is of utmost importance both for the surgeon operating at this level, for radiologists performing a catheterization, and for the clinician in general.2 The internal jugular vein may be endangered during removal of tuberculous or neoplastic lymph nodes.1 Their involvement in these different procedures can lead to various acute complications such as accidental carotid arterial puncture, irritation to the brachial plexus, pericardial tamponade, haemothorax, pneumothorax and formation of a local haematoma compromising the upper airway.3 Not many dissection studies have been done on internal jugular vein and its variations in Karnataka/ India. Hence this study becomes essential. ANNEXURE-III 6.2 REVIEW OF LITERATURE: 1. Internal jugular vein is a large vein collecting blood from skull, brain, superficial parts of face and much of neck. It begins at the cranial base, in the posterior compartment of jugular foramen, where it is continuous with the sigmoid sinus. It ultimately terminates by uniting with the subclavian vein, posterior to the sternal end of clavicle, to form the brachiocephalic vein, which in turn empty into superior vena cava. As it descends in the carotid sheath, it is related to internal and common carotid arteries on the medial side and the vagus nerve between vein and arteries, but posterior to them. Superficially, it is overlapped by sternocleidomastoid muscle and the deep cervical lymph nodes lie along its superficial aspect. Tributaries received by the vein, during its course through the neck include: facial vein, lingual vein, pharyngeal vein, superior and middle thyroid veins and occasionally occipital vein. The thoracic duct opens near the union of left subclavian vein and internal jugular vein and right lymphatic duct opens at the same site on right. 2. A study conducted on 60 human cadavers, observed the internal and external jugular veins from the point of view of their origin, course and affluents. Following morphological variabilities were observed in case of the jugular veinsExternal jugular vein that receives as affluents the facial and lingual veins and drains into internal jugular veins, draining the latter’s territory – 3.33% Internal jugular vein that receives the lingual, upper thyroid and facial veins, independent13.33%, via the linguofacial trunk- 50%, and via thyrolinguofacial trunk-33%. The authors have correlated these anomalies with disorders in the ontogenetic development of the veins of the neck. The superficial veins of the head and neck arise from the superficial capillary plexus which eventually, will form the primary vein of the head. By the enlargement of the individual capillaries, the confluence and regression of some of the veins in the area where the blood flow was deviated, wide canals are formed. The factors controlling this are still largely unknown. With the development of the cranium, the first vessel that can be identified is the ventral pharyngeal vein, which drains most of the mandibular bone and the hyoid arch in the common cardinal vein. Progressively, as the neck lengthens, its drainage level shifts towards the cranial part of the precardial vein which later develops into the internal jugular vein. 3. A study was done on 104 consecutive uraemic patients undergoing creation of internal jugular vein temporary angioaccess, focusing on the anatomical variation of internal jugular vein. The internal jugular veins were classified according to their diameters and anatomical locations. The internal jugular veins were divided into adequate sized (5mm diameter or more) and small sized (less than 5mm) groups. An internal jugular vein was defined to be of normal location if it lay superficially and laterally to the carotid artery with a distance less than 10mm between them. An internal jugular vein located ≥ 10mm lateral to the carotid artery was defined to be far away from the carotid artery. The reverse of carotid artery and internal jugular vein indicated that the internal jugular vein was located medially to the carotid artery. The term ‘overriding’ was used for an internal jugular vein located directly above the carotid artery. This study found anatomical variations in 18.3% of the right and 16.4% of the left internal jugular veins. Unilateral variations were found in 17.3% and bilateral variations were discovered in 8.7%. A total of 26% had internal jugular vein anatomical variations that might contribute to difficulty in external landmark guided internal jugular veins cannulation. 4. The relationship between internal jugular vein diameter as measured with an ultrasound imaging machine and external jugular vein diameter was studied in 50 anesthetized patients undergoing elective cardiac surgery. There was an inverse correlation between external jugular vein diameter and internal jugular vein diameter (r=-0.47, p<0.001). 40% patients with an external jugular vein diameter of 7mm or greater had an internal jugular vein diameter of less than 15mm. No patient with an external jugular vein diameter of less than 7mm had an internal jugular vein diameter of less than 20mm. No other patient dimension (height, weight, body mass index, neck circumference) predicted internal jugular vein size. These results suggest that a large external jugular vein (i.e. 7mm or greater in external diameter) may be associated with a small internal jugular vein. 5. A rare bilateral duplication of the internal jugular vein was discovered during cadaveric dissection. From each jugular foramen, a single internal jugular vein descended to the level of the hyoid bone then divided into medial and lateral veins. The medial internal jugular veins travelled in the carotid sheath; the lateral internal jugular veins coursed posterolateral to the sheath across the lateral cervical region (posterior triangle) of the neck. On the right side, both internal jugular veins entered the subclavian vein separately. On the left side, the medial internal jugular vein drained into a large bulbous jugulovertebrosubclavian sinus. The lateral vein diverged posterolaterally toward the border of trapezius muscle, then received transverse cervical vein, and then turned sharply anteromedially to drain into the jugulovertebrosubclavian sinus. The study also suggests that internal jugular vein duplication differs from fenestration anatomically and potentially, developmentally. The mechanism of development and the clinical significance of multiple internal jugular veins are also discussed. ANNEXURE-IV 6.3 OBJECTIVES OF STUDY: To find out: 1. 2. 3. 4. 5. Location of internal jugular vein in relation to common carotid artery Position of internal jugular vein in relation to heads of sternocleidomastoid Mode of termination of internal jugular vein Afferent vessels of internal jugular vein Caliber: right and left internal and external jugular veins and common carotid arteries at the level of cricoid cartilage ANNEXURE-V MATERIAL AND METHODS: 7.1 SOURCE OF DATA: The preserved human cadavers from Department of Anatomy, Kempegowda Institute of Medical Sciences and other Medical Colleges in and around Bangalore. 7.2 METHOD OF COLLECTION OF DATA: Purposive sampling technique will be used. The study will be conducted on 50 adult human cadavers irrespective of sex. Gross dissection will be done by following the guidelines of Cunningham’s manual. The deep dissection of neck will be done. Carotid sheath will be exposed and internal jugular vein will be identified on both sides. Relevant findings regarding its location in relation to carotid artery, heads of sternocleidomastoid and termination of afferent vessels will be noted. The caliber of the internal jugular vein, external jugular vein and common carotid arteries will be measured using sliding calipers at the level of cricoid cartilage. Statistical analysis will be done based on these measurements using descriptive statistics like percentage and mean. Paired-t test will be used to compare the calibers of veins and arteries of both sides. ANNEXURE-VII LIST OF REFERENCES: 1. Williams P.L., Bannister L.H., Berry M.M., Collins P., Dyson M., Dussek J.E.et.al. Gray’s anatomy, 39th Ed. Edinburgh: Elsevier Ltd., 2006. 552 2. Monica-Adriana Vaida., Niculescu V., Motoc A., Bolintineanu S., Izabella Sargan., Niculescu M. C. 2006 “Correlations between anomalies of jugular veins and areas of vascular drainage of head and neck.” Romanian Journal of Morphology and Embryology, 47(3): 287-90 3. Bing-Shi Lin., Chi-Woon Kong., Der-Cherng Tarng., Tung-Po Huang., Gau-Jun Tang. 1998 “Anatomical variation of the internal jugular vein and its impact on temporary haemodialysis vascular access: an ultrasonographic survey in uraemic patients.” Nephrology Dialysis Transplantation, 13: 134-38 4. Stickle B. R., McFarlane H. 1997 “Prediction of a small internal jugular vein by external jugular vein diameter.” Anaesthesia, 52: 220-22 5. Downie S.A., Schalop L., Mazurek J.N., Savitch G., Lelonek G.J., Olson T.R. 2007 “Bilateral duplicated internal jugular veins: case study and literature review.” Clinical Anatomy, 20(3): 260-6