* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Renal System
Survey
Document related concepts
Transcript
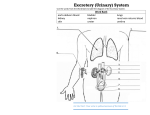
Renal System Overview of renal System: While bladder is contracted to urinate—ureters clamp off so there is no backflow of urine into the ureters. Urethra—Women short, 2-3” Men longer 8” Urinary meatus—outside Ureters, bladder and urethra, meatus—all innervated, can feel pain, Right kidney is a little lower than the left because the liver places it down. Kidneys are surrounded by a capsule. They will not feel pain unless the capsule is stretched. Kidney pain is flank pain. Kidneys need 20% of cardiac output in order to function—that is about 1200 ml of blood in a minute. Biggest cause of kidney failure—HTN, Diabetes, ETOH and drug abuse Functional unit of kidney—nephrons—there are over 1 million nephrons in each kidney Nephrons—glomelular filtration, Bowman’s capsule surrounds glomelular capillaries. Less than 1% of the blood filtered is excreted. Renal Pelvis—only holds 5 mL of urine. ADH (Vasopressin)—causes reabsorption of water/fluids—concentrated. Functions of Kidneys: 1. Fluid and electrolyte balance 2. acid and base balance 3. Excretion of wastes 4. BP regulation—renin—angiotension—aldosterone cycle 5. Formation of RBC—erythropoetin is a renal hormone that stimulates the formation of RBC from the bone marrow. 6. Vit. D—prohormone is converted to an active form by the kidneys. Helps with calcium reabsorption and use by the bones. Assessing the kidneys: 1. Creatinine—0.7-1.3 norms the end product of muscle metabolism. Solely excreted by the kidney. Used as a gauge of kidney function. If kidney failure—decreases in fct—increase of creatinine in blood. Can’t pull it across the glomerular filter to excrete. 2. BUN—blood urea nitrogen— Norm. 10-20. end product of protein metabolism. Solely excreted by the kidney. Elevated levels—fail or decreases kidney function. Cannot pull it out to excrete. 3. IUP—intravenous pyelogram determines size, shape, and excretory function. A dye is injected through vein Caution—allergic to iodine or shellfish. Bowel must be prepped—empty the bowel so you can see the kidneys 4. Retrograde urography Cath the urinary tract Inject a dye into the ureters. Renal pelvis—ureters—bladder After test have pt push fluids. Pg 1158—table of drugs that are nephrotoxic. -mycin antibiotics esp. when given IV. Administer over an hour. Pg 1163 tests UTI Most common pathogen—E coli Pyelonephritis—infection in the kidneys Cystitis—infection in the bladder Urethritis—infection in the urethra, more common in men usually from gonorrhea Pathophysiology—UTI Most common route for UTI is organism comes from urethra or bladder, come from below. Vagina or perineum—wipe front to back. Other routes—through the blood stream, or the lymphatic system sits in kidneys or Uriniary tract. Very uncommon, usually down and moves up. Risk factors for UTI— Aging—more underlying diseases. Everything slows down. Impaired immune response Females—short urethra, void after sex, wipe front to back Males—prostatic hypertrophy—enlargement of prostate—normal with aging, prevents urine flow Urinary tract obstruction—stone. Scarring Sex—void after sex, honeymoon cystitis, now 8th grade cystitis?? :) Signs and Symptoms Dysuria Frequency Urgency Hesitancy Suprapubic discomfort US—cloudy, foul odor Flank pain—kidney—there will be pyuria (pus in urine) Pyelonephritis—increased temp. Diagnostics H and P UA—clean catch, or straight cath Urine culture and sensitivity Treatment for cystitis Antibiotics—short therapy Bactrim—sulfa drug antiinfective. TAKE ENTIRE COURSE OF MEDICATION TO PREVENT RESISTANCE Urinary analgesics—pyridium will turn urine orange. Dyrenium Force fluids—caffeine is irritant, suppresses ADH, take cranberry juice Wipe front to back Void after sex Avoid harsh soaps like bubble bath Void frequently 10/11/04 Neophrostomy tube— Pyelostomy tube—diverts the urine from the ureter. ~ Renal pelvis only hold 5 mLs of urine. ~ Cannot irrigate with 30 mLs only 2-3 First sign or symptom of bladder or kidney cancer is gross hematuria. Kidneys—maintain fluid and electrolyte balance, regulated BP, begins formation of RBC (Erythropoetin) allows Ca to be absorbed from the gut, they maintain acid/base balance. Oliuria—less than 400 mL of urine output. Auria—less than 100 mL of urine output. I. Acute renal failure: Rapid decline in kidney function.—leads to azotemia Azotemia (nitrogenous waste in the blood) BUN and creatinine. Not symptomatic. Progresses to Uremia—(urine in the blood) person is symptomatic. Urine output of less than 400 mL in one day. Causes: 1. Pre-renal hypovolemia ACE inhibitors Severe burns excessive diuresis MI—decreased CO 2. Intrarenal Nephrotoxins—gentomycin Transfusion rx.—Hemolysis of RBC Amphotericin B 3. Post-renal Prostatic Ca or hypertrophy leads to obstructions Stones Hydronephrosis—kidney keeps making urine even if it is blocked. All of these things lead to ischemic changes in the kidneys. Clinical Course: 1. oliguric phase—1-7 days after injury. 2. GFR—15 mL/min 3. leads to anuria 4. specific gravity test—ability to diulute or concentrate an Urine. Normals 1.003-1.030 Low is dilute, high is concentrated. Signs and symptoms— 1. UA—output of less than 100 mL ?WBC in the urine? 2. Fluid volume excess—kidneys can’t get rid of urine—leads to overload. ~ increased BP, bounding pulse, Neck vein distention, edema, CHF 3. kidneys can’t synthesize ammonia—needed for Hydrogen ion excretion—results in metabolic acidosis. 4. Sodium imbalance—decreased sodium level—confusion 5. potassium excess—hyperkalemia. (3.5-5.0 normals) BIG CAUTION is when you get to 6—prone to life-threatening arrythmias—the kidneys can’t excrete K+. Will also have peaked T-waves, may have ST depression. Metabolic acidosis—causes K+ release from the cells. Tissue death from trauma causes release of K. Treatment for hyperkalemia—greater than 6. 1. IV insulin—regular is only type that can be given IV. Moves K+ back into the cells Dextrose IV solution (D5)—to prevent hypoglycemia from the insulin. 2. Sodium Bicarbinate IV Moves K+ into cells 3. Kaexylate enema Exchange resin K+ for Na Should have stool after enema to get rid of K+. 4. increased BUN (norm 10-20) and creatinine levels (norms .07-.03) 5. Decreased Ca levels, because of decreased GI absorption—Vit. D def. II. Diruretic phase—kidneys beginning to work again. Lasts 1-3 weeks Gradual increase in urinary output—1-3 L a day. Up to 5 L/day—can result in hypovolemia. Decreased BP Decreased K+ Recovery is evident when BUN and creatinine return to normal. III. Diagnostics Pg 1214 table 45-3 H and P—causative factor. UA—specific gravity and osmolatity— BUN and creatinine levels Electrolytes—K, Na,Mg IVP— MRI CT scan IV. Collaborative Care Fluid restriction—add 600 mLs to yesterdays output—total fluid allowed for the day. Sodium restriction—so it doesn’t conserve more fluid Diuretics—lasix, bumix, (osmotic diuretics) Manitol. ACE inhibitors—prinivil Ca channel blockers—causes venous dilation—renoprotectant—cardizem Beta blockers—lopressor Dialysis—artificial kidney, peritoneal or hemo-dialysis. Monitor I and O, and weight. Leading cause of death in acute renal failure—infection Use meticulous skin care and aseptic technique. I. Chronic Renal failure Progressive irreversible destruction of nephrons in both kidneys. Scar tissue forms. Most common causes are HTN, and diabetes. (African American and American Indians more prone to) A. Signs and Symptoms: 1. Elevated BUN Nausea and vomiting Lethargy Coma Sezieres. 2. Elevated triglycerides 3. Increased K+ 4. Metabolic Acidosis—dyspneic—Kussmaul’s respirations (deep resp) 5. Anemia—decreased erythropoetin yellowish, pale skin. uremic frost—skin is trying to excrete waste. Pruiritis—crawling, itching from down deep. 6. Platelets function is altered—bleeding tendencies. 7. Infection—WBC function is altered—diminished immune response. 8. Cardiovascular, increased BP, CHF, arrhythmias. 9. Stomatitis—mouth ulcerations, breath smells like urine. Infertility Anorexia N/V and diarrhea. 10. Infertility Diagnotic studies—same as acute UA—for creatinine clearance. 24 hr urine collection. Starts and ends with an empty bladder. B. Medicines—a lot same as acute 1. increased BP—diuretics, ACE inhibitors, Ca channel blockers, Beta blockers. Think about toxicity, not being excreted sufficiently. 2. Hyperkalemia—tx same as acute 3. Anemia—transfusions—overload and incompatibility don’t usually give. Usually give Procrit—stimulates formation of RBC (Erythropoetin). 4. Diet must be done by a nutritionist, protein, Na etc. restriction. Very complicated. 5. Will always have fluid restriction even they have dialysis. 6. III. Dialysis—Movement of fluid and particles across a semi-permeable membrane. Movement from blood or peritoneal membrane and into the dialysate (dialysis fluid). Types of dialysis a) peritoneal b) Hemodialysis. Principles of dialysis: a) Osmosis—movement of water from greater to lower b) Diffusion—movement of solutes from greater to lower. c) Ultrafiltration—adding an artificial pressure gradient—artificial pull, done by machine. Peritoneal dialysis—pg 1229 and 1230 pictures. Dialysate pulls excess fluids, electrolytes and waste etc. out across the peritoneal membrane by osmosis. Can maintain some independence—can do at home etc. 3 steps: qid a) instill dialysate into the abdomen—2-3 liters. b) Dwell time—30 min. c) Drain--gravity Hemodialysis— Vascular access device Types: a) arteriovenous shunt—fistula (abnormal opening between two things) pg 1233. Leaves through the artery and comes back through a vein. Rate of flow is 200-500 mL/min. diasylate pulls waste from blood. Takes 4-6 hours to complete Must be done 3 times a week. Premedicate with heparin to prevent clotting. b) Subclavian catheter—3 lumen Complications from dialysis— Hypotension—0.9% NaCl Disequalibrium syndrome Blood loss Sepsis—infection throughout system Kidney transplants Types: a) Cadaver—90% success rate b) Live donor—95% success rate. Biggest complication is rejection: hyperacute—in OR, or long-term—1 yr later. The old kidneys are not removed unless there is severe uncontrolled HTN or severe infections. Must be on anti-rejection drugs for life. Immuran Steroids—prednisone chronic antiinflammatory drugs Preventative ulcer meds--amphajel