* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download DISCLAIMER
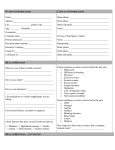
Survey
Document related concepts
Transcript
1 DISCLAIMER All statements contained in this manual, and the proceedings and objectives outlined herein, are informative only and represent that which the Association of Polysomnographic Technologists (APT) considers to be of the highest quality and methodology for the performance of polysomnographic (PSG) technology as well as providing for competent patient care, service, or performance of procedures relating to any particular set of circumstances. These materials are intended for use as a reference guide. They may be used as whole or in part. In all cases, the protocols for all procedures used in the sleep facility must reflect the actual operation in the sleep facility and they must conform to Clinical Practice Parameter guidelines established and accepted by the American Academy of Sleep Medicine (AASM), if they exist. If any protocol or procedure described in these samples is found to conflict with any Clinical Practice Parameter guidelines accepted by the AASM, the AASM accepted practice parameters will take precedence and must be followed. These documents do not supersede federal, state or local regulations pertaining to operating a medical practice. It is the intention of the APT Board of Directors that this manual be used as consultative material in striving for optimum patient care and treatment by the polysomnographic technologist in an sleep disorders facility under the direction of a state licensed physician who is preferably Diplomat of the American Board of Sleep Medicine. It is recognized that any specific procedure of service is always subject to modification, depending upon the circumstances of a particular case. Although the APT sets forth these standardized protocols, it realizes that certain aspects should be left to the discretion of the physicians licensed in the states in which these protocols will be used. This document contains information that is privileged and is intended solely for the use of the individual or entity by which it was purchased. You are hereby notified that any disclosure, copying or distribution of the contents of this document is prohibited. BACK TO TABLE OF CONTENTS 2 Edward Dana, President 502-387-6133 Dr. Kheder Kutmah, Medical Director 859-992-4660 Dr. Azmi Draw, Staff Physician 502-216-0191 Contessa Tyler, Clinical Coordinator 502-298-8279 Rana Dana, Business Manager 502-994-6897 Tina Bratcher, Office Manager 502-345-1226 Jennifer Tooley, Marketer 502-905-7874 Alma Dzebic, Secretary 502-365-6389 Mark Nunez, Technician 270-317-7714 Sarah Ford, Technician 502-291-2995 Mecca Schmitz, Technician 502-671-3967 James Thornton, Technician 270-317-7508 BACK TO TABLE OF CONTENTS 3 Table of Contents Appointment and requirement of Sleep Staff physician…………………………. 8 Assembly, Maintenance and Storage of Patient Charts…………………………...9 Communication with Primary Care Physician… ………………………………...12 Protocol for Follow up Calls …… ………………………………………..13 Protocol for Patient Acceptance Criterion … ………………………………14 Referrals for Evaluation/ Practice Parameters____________________________ 18 Authorization (Insurance) and Processing of Charges for Sleep Studies________20 Staffing Patterns and Ratios__________________________________________22 Fire Plan…………………………………………………………………………..23 Bomb Threat Plan………………………………………………………………...32 Severe Weather___________________________________________________35 Tornado Procedures________________________________________________36 Earthquake_______________________________________________________38 Emergency Contact________________________________________________39 Emergencies and Responses_________________________________________42 Psychiatric/ Belligerent Emergencies___________________________________46 Infection Control__________________________________________________47 Cleaning and Maintenance of Equipment and Facilities____________________49 Maintenance and Cleaning of Reusable Sensors and Interface Device…………51 Hazardous Materials……………………………………………………………..53 BACK TO TABLE OF CONTENTS 4 Latex Sensitivity…………………………………………………………………55 Polysomnographic Montages……………………………………………………57 Patient Arrival, Preparation and Electrode / Sensor Application……………….61 Physiological Calibrations Procedures………………………………………….67 Calibration of Equipment for Polysomnogram………………………………….71 Documentation During Polysomnogram………………………………………..76 Pediatric Polysomnography 13 Yeasrs Old and Under………………………...78 Et C02_________________________________________________________81 C02 Capnograph________________________________________________83 Pediatric Polusomnography 14 years old to 18 years old_________________85 Technician Record Review________________________________________88 Scoring Guidelines …………………………………………………91 Electricals Safety________________________________________________95 Electrical______________________________________________________97 Technical Failures Due to Equipment Malfunction_____________________99 Scoring Sleep Related Events ……………………………………………….100 Scoring EEG during Sleep________________________________________103 Titration of Positive Airway Pressure during Sleep…………………………..109 Titration of Positive Airway Pressure during sleep for Patient 13 Year old and under__117 Follow up Call after CPAP________________________________________125 BACK TO TABLE OF CONTENTS 5 Split Night Study……………………………………………………………...126 Oral/Nasal or Full Face Mask…………………………………………………128 Monitoring Oxygen Saturation Levels and Administration of____________130 Multiple Sleep Latency Test (MSLT)…………………………………………134 Portable Testing ……………………………………136 Portable Testing Trainee__________________________________________138 Fatigue, Sleepiness and Driving____________________________________140 Quality Improvement____________________________________________141 Maintenance of Wakefulness Test (MWT)____________________________142 Inter-Scorer Reliability Quality Assurance…………………………………147 Quality Assurance Policy________________________________________149 Employee Schedule and Time off Requests…………………………………..156 Addendum-Documents for the Profession, Sample Forms and Policies....158 Job Descriptions for Polysomnographic Technology…………………………159 Polysomnographic Training…………………………………………..160 Polysomnographic Technician………………………………………..162 Polysomnographic Technologist……………………………………...163 Polysomnographic Technology Core Competencies_______________167 Medical Emergency________________________________________176 Table of Contents – continued BACK TO TABLE OF CONTENTS 6 Confidentiality of Patient Information Policy and Medical Record__177 Capnography………………………………………………………….178 Polysomnographic Montages and Equipment Calibration and Function….179 Scoring Sleep Stages and Clinical Events…………………………………181 Supplemental Low Flow Oxygen Titration………………………………..183 Staff Ratios: Third shift staffing…………………………………………………185 Epworth Sleepiness Scale………………………………………………………….186 MSLT Pre Sleep Questionnaire……………………………………………………187 MSLT Post Sleep Questionnaire…………………………………………………..188 MWT Technical Documentation Form……………………………………………189 Physician Order Sheet……………………………………………………………..190 Standing Order Policy……………………………………………………………..191 Fire/Evacuation Check List and Responsibilities…………………………………192 Bed Partner Questionnaire………………………………………………………...193 Cancellation Protocol……………………………………………………………...194 CPAP/Bi Level PAP Titration Log Form…………………………………………195 Direct Referral Form………………………………………………………………196 Technician Observation Form_________________________________________198 BACK TO TABLE OF CONTENTS 7 Table of Contents – continued Pre-Sleep Question_______________________________________________200_ Medication Acknowledgement Form____________________________________203 MSLT Instruction Sheet______________________________________________205 24 Hr Phone Access________________________________________________206 24 Hr on Call for Doctor_____________________________________________207 Infection Control Policy…………………………………………………………...208 Assembly, Maintenance and Storage of Charts………………………………….210 BACK TO TABLE OF CONTENTS 8 Sleep Center of Kentuckiana Policy and Procedure TITLE: Appointment and Requirements of Sleep Staff Physicians ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s): 3-1-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 Every sleep disorders centers has the responsibility to meet all federal, state and local regulations pertaining to operating a medical practice, regardless of setting: hospital based, freestanding or other. POLICY: 1.0 Clinical Personnel Requirements 1.1 Each sleep disorders center must have as medical director a physician that holds a valid medical license in the state of the center. 1.2 The physician must be in good standing with the state medical board. 1.3 Each accredited sleep disorder center must have a diplomat of the American Board of Sleep Medicine (ABSM) on staff, or an individual who has been accepted by the ABSM to sit for the certification exam or equivalent. 1.4 Technologists must work under the direction of a state licensed physician. BACK TO TABLE OF CONTENTS 9 Sleep Center of Kentuckiana Policy and Procedure TITLE: Assembly, Maintenance and Storage of Patients Charts ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s): 3-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 TITLE: Assembly, Maintenance and Storage of Charts 1.3.1.1 Chief Complaint. 1.3.1.2 Sleep history. 1.3.1.3 Details of present illness. 1.3.1.4 Relevant past, social and family histories. 2.0 Medications. 3.0 Physical Exam. 3.1 4.0 Medication list is noted in the chart. If any new prescriptions is given it will be copied and place in chart. The physical examination should reflect a comprehensive inventory of body systems. Diagnostic Orders. 4.1 Appropriate authorizations from third party payers. 4.2 Signed consents for procedures. 4.3 Signed prescriptions from ordering physician; including procedure and diagnostic codes. Copies left in file. BACK TO TABLE OF CONTENTS 10 Page 2 TITLE: Assembly, Maintenance and Storage of Charts 5.0 Reports. 5.1 Sleep study reports are generated by the technologist. 5.2 The interpreting physician correlates the report with the raw data and does an interpretation. The interpretation will include the diagnosis and treatment recommendations. 6.0 Recording Samples. 7.0 Interpretation and Treatment Recommendations. 7.1 Follow up office note and/or treatment options. PAGE 3 TITLE: Assembly, Maintenance and Storage of Charts 8.0 Progress Notes. 8.1 All communication with patient or regarding the patient shall be noted, dated, and initialed on the progress note in black ink. 8.2 9.0 Communication should be documented at the time of the contact. MD to review care plan, update, and sign. Chart Maintenance. 9.1 Designated sleep disorders center staff will maintain current charts at designated location. 9.2 Designated sleep disorders center staff will assume responsibility for purging and/or archiving charts. BACK TO TABLE OF CONTENTS 11 Page 3 TITLE: Assembly, Maintenance and Storage of Charts 10.0 Chart Storage. 10.1 Current charts will be stored at the sleep disorders center in securable file cabinets or secured area within the center. 10.2 Charts that have been archived will be stored in a facility that meets the standards for medical record storage. 10.3 Chart is storage on a secure online storage (Dropbox). BACK TO TABLE OF CONTENTS 12 Policy and Procedure TITLE: Communication with Primary Care Physician ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s): 3-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 Policy: Sleep Center of Kentuckiana is facility designed to accommodate patients for evaluation and treatment of sleep disorders and pulmonary problems. In order to keep high quality of continuing medical care Sleep Center of Kentuckiana issued the following procedure to assure proper communication with the referring or primary care physician. . Procedure: 1- If patient is being referred from other physician for specific problem: a- Patient will be seen regarding that problem. b- If the problem is not clear our physician will clarify it with the referring physician or facility. c- After evaluating the patient our physician will send office notes or sleep study reports to the referring or primary care physician . d- Written letter/ copy of any test result will be sent to the referring physician. 2- If patient presented to the Sleep Center of Kentuckiana without referral, the primary care physician will be contacted to request the needed information a- If patient need to be admitted to the hospital arrangements will be made via ambulance. b- If patient has medical problem and needs specific follow up our physician will schedule testing through the office. c- If additional testing is required this information will be noted on the physician office note that is dictated and sent to the referring or primary care physician. . BACK TO TABLE OF CONTENTS 13 Policy and Procedure TITLE: Protocol for Follow up Calls ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s):3-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 Purpose: To ensure patient care for treatment use and response to therapy. Policy: Sleep Center of Kentuckiana believes that continuing medical care is as important as the initial treatment. As long as follow up calls will improve patient care and give our staff back up information regarding our service so we can improve service. Sleep Center of Kentuckiana is planning to perform follow up calls within 48 to 72 hours from the initial visit. Procedure: 1- Sleep Center of Kentuckiana personnel is going to perform there calls. 2- Introduce the facility and caller and position. 3- Ask for the patient (Guardian if minor or demented). 4- Avoid giving any information to anyone expect the patient or the guardian. 5- Conversation should include: a- Reason for call. b- Scheduling of appointment with the Doctor to Discuss result. c- Inform patient that the test result will be sent to referring Doctor, or PCP. d- Discuss any question, or concerns. e- Rate patient experience at the lab. 6- If there is an answering machine or patient not available leave brief message for patient to call back only. The office is open Monday – Friday from 9am-5pm and our answering machine is on after hours and calls will be returned the next business day. 7- All information to be documented in the chart. BACK TO TABLE OF CONTENTS 14 Policy and Procedure TITLE: Protocol for Patient Acceptance Criterion ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s):03-01-2007, 3-08-2011 REVISION DATE(s): 3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 To set standard criterion for a patient to be referred to the sleep disorders center to be evaluated with an overnight polysomnogram. The sleep disorders center is a specialized diagnostic facility where full polysomnographic evaluation is utilized to determine the diagnosis of a sleep disorder. POLICY: 1.0 General Considerations 1.1 Patients shall be seen on referral from a licensed physician according to the guidelines for patient referral of the state within which the sleep disorder center is located with physician order. 1.2 Written order. 1.2.1 Faxed from referring physician office. 1.2.2 Written on a prescription and brought in by patient or copy of a physician note; to include consult, history and physical. 1.3 Verbal order. 1.3.1 1.4 Complete verbal order form according to facility policy. Demographic and insurance information is obtained from referring physician’s office. ( Note : These duties may be performed by clerical staff) BACK TO TABLE OF CONTENTS 15 PAGE 2 TITLE: Patient Acceptance Criterion 1.4.1 Insurance is verified and determination for pre authorization is determined and, if required, obtained prior to scheduling patient. 1.4.2 Sleep chart is put together and information placed in the chart. 2.0 Referral Process 2.1 Clinical indication for sleep disorder consultation and testing. 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.1.8 2.1.9 3.0 Excessive daytime sleepiness and related exhaustion. Narcolepsy. Sleep apnea. Excessive snoring. Nocturnal myoclonus. Insomnia. Nocturnal esophageal reflux. Nighttime epileptic seizures. Parasomnias, including sleep walking, enuresis. Medical Director 3.1 The medical director of the sleep disorders center shall be a licensed physician in the state the center is located in. 3.2 The center may set a protocol for the patient to have an office visit with the medical director for all self referred patients and based on the discretion of referring MD. 3.3 The center may set a protocol for a patient to be referred to the sleep disorders center without an office visit with the medical director if referring physician is one of the following: Sleep MD, Pulmonologist, ENT, and Neurologist. BACK TO TABLE OF CONTENTS 16 PAGE 3 TITLE: Patient Acceptance Criterion 4.0 Patient Assessment 4.1 The patient should be medically stable when the polysomnogram is performed in the outpatient facility. 4.1.1 Patient must be able to understand and follow directions to obtain a valid sleep study, as well as be able to care for his/her personal needs. 4.1.2 4.1.3 4.2 During the order intake, it will be determined if this is the initial evaluation, repeat PSG evaluation for titration of Nasal CPAP/Bilevel, or repeat PSG evaluation post-surgical treatment or weight loss. Determine if patient will require a family member to be present. 4.1.3.1 Language interpretation, including sign language. 4.1.3.2 Physical disability. 4.1.3.3 Transportation needs. 4.1.3.4 Age limit above 7 years old. Standardized technician to patient ratio. 1:2 BACK TO TABLE OF CONTENTS 17 PAGE 4 TITLE: Patient Acceptance Criterion 5.0 Patient Information Packet 5.1 Patient will be mailed prior to consult or complete day of appointment. 5.2 Include in packet. 5.2.1 Sleep History Questionnaire 5.2.2 Beck Inventory. 5.2.3 Epworth Sleepiness Scale. 5.2.4 Consent to undergo sleep study 5.2.5 Directions to sleep disorders center with confirmation letter of study date and time. 5.2.6 HIPPA consent form. BACK TO TABLE OF CONTENTS 18 Policy and Procedure TITLE: Referrals for Evaluation/ Practice Parameters ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURPOSE: 1.0 To establish a written criteria to handle referrals for sleep disorders evaluations. General Considerations 1.1 In accordance with AASM guidelines, it is strongly recommended that a sleep disorders center (SDC) medical director or staff physician see all patients prior to polysomnography. 1.2 Sleep disorders center patients come from several sources; physician referrals for clinical evaluation, self-referrals for clinical evaluation, and direct referrals for polysomnography only. POLICY: 1.0 Referrals for Clinical Evaluations 1.1 Patients referred for clinical evaluation, both physician and self-referred, must be evaluated by a sleep center physician prior to polysomnography. 1.2 Sleep disorders center staff physician will obtain a history, which conforms to the AASM Practice Parameters for the Indications for Polysomnography and Related Procedures. In addition to this history, the physician will obtain a medical history, which will include past/present illnesses, medication history, and allergies. 1.3 Each patient should have a physical examination by the SDC medical director or staff physician. 1.4 The appropriate polysomnographic evaluation is ordered by the SDC medical director or staff physician. BACK TO TABLE OF CONTENTS 19 PAGE 2 Referrals for Evaluation 2.0 Direct referrals for Polysomnography only 2.2 2.1 Direct referral 2.1.1 Referring physician must provide 2.1.2 Patient history, which conforms to the AASM Practice Parameters for the Indications for Polysomnography and Related Procedures. 2.1.3 Medical history, which will include past/present illnesses, medication history, allergies, and the results of a physical examination. The SDC medical director or staff physician will ensure that each patient referred meets the minimum indications for polysomnography in accordance with the AASM Practice Parameters. BACK TO TABLE OF CONTENTS 20 Policy and Procedure TITLE: Authorization (insurance) and Processing of Charges For Sleep Studies ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s): 3-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 PURPOSE: To optimize cash flow and prompt payment by patient and third party payer. POLICY: Every patient is to have a clear understanding of his or her financial responsibility for procedures rendered. PROCEDURE: 1.0 2.0 Information specific to the patient’s insurance will be obtained prior to being seen at the Sleep Disorders Center. Information may include: 1.1 Patient Name 1.2 Name of Insured 1.3 Patient’s Social Security Number 1.4 Patient’s Date of Birth 1.5 Insurance Company Name 1.6 Insurance Company Address 1.7 Insurance Company Phone Number 1.8 Policy Number and Group Number Verify medical insurance coverage BACK TO TABLE OF CONTENTS 21 Page 2 TITLE: Authorization (insurance) and Processing of Charges For Sleep Studies 2.1 Necessary pre-authorization should be obtained per insurance coverage requirements prior to study. 2.2 Financial obligations should be explained to patient upon request. 2.3 Refer to patient billing representative for specific billing questions. BACK TO TABLE OF CONTENTS 22 Policy and Procedure TITLE: Staffing Patterns and Ratios ORIGINAL DATE: 9-01-2006 EFFECTIVE DATE: 9-01-2006 REVIEW DATE(s): 3-01-2007 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 To establish technologist to patient ratios appropriate for patient care and to ensure patient safety. POLICY: 1.0 A ratio of two (2) patients to one (1) technician/technologist, as recommended under the American Academy of Sleep Medicine accreditation standards. 1.1 In the event that the sleep center will be performing pediatric studies with pediatric patients of <4 years of age, the ratio of technologist to pediatric patient will be 1:1. 1.2 If a patient presents to the sleep center and requires continuous medical attention (due to underlying medical problems), the ratio of technologist to patient should be 1:1. See Addendum, page 145 BACK TO TABLE OF CONTENTS 23 ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Fire Plan EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: A well-documented and rehearsed fire plan is essential to the sleep disorders center. Fire drills should be conducted on all shifts at regular intervals. These drills are called at unspecific hours of the day and night. Participation in these drills is essential for all staff personnel in order to eliminate confusion during a real fire emergency. These drills are necessary to keep you aware of what must be done in case of fire. All drills are necessary to provide for patient and employee safety and all staff is to treat all alarms as real fires. Of course, the best defense against fires is the prevention of them in the first place. Several parts of this fire plan are aimed at the prevention of fire. The importance of fire prevention cannot be over emphasized in a hospital based and free-standing sleep disorders centers. ESSENTIAL COMPONENTS OF THE FIRE PLAN: Employees, Tech and Patient: The staff member is the first line of defense in the prevention and protection from fires. It is your responsibility to report all fire hazards in your daily travels throughout the facility. With everyone’s help, we can prevent fires. Structure: The sleep disorders center should be built with fire resistive materials constructed to conform to local, state and national fire and electrical codes for health care facilities. The basic facility structure is designed to resist fire. Most of the materials that are utilized to make the center comfortable and attractive are combustible. In an effort to minimize the spread of smoke and fire, the center should ideally be constructed with smoke containment divisions to provide compartmentalization, which minimizes the spread of smoke and or fire. Compartments must be able to close during a fire emergency to provide the sealed compartments needed to retard the growth of an active fire. These barriers to smoke and fire provide us with a safe exit from the effected area. To maintain optimum fire compartmentalization and to keep the emergency exits free, please ensure that. All fire doors remain free of objects such as chairs, door wedges or carts that may prevent closing During a fire emergency. BACK TO TABLE OF CONTENTS 24 PAGE 2 TITLE: Fire Plan All exits and exit-ways remain clear at all times-exit doors must never be blocked, for any reason. Note: Report all violations to your department supervisor or unit manager. Fire Alarm System / Fire Suppression System: The fire alarm system should be designed to provide early warning of a fire situation. The system should be able to be activated manually by use of the fire alarm pull stations, located throughout the facility. It should also be activated automatically when a smoke detector is tripped. When the alarm system is activated by an employee, the employee needs to call 911 Tell the 911 dispatcher WHO is calling, WHERE the location of the fire is, and WHAT is burning and its intensity. Doing this allows the operator or the 911 dispatcher to notify the fire department immediately. Should the alarm be activated by a smoke detector, sprinkler system or if you would fail to call the operator, the automatic fire system should notify the fire department after a 3-minute interval. Smoke Detector System-Smoke detectors be installed in corridors, hazardous areas and in the air conditioning ductwork. The smoke detectors give early warning of a fire, Cigarette smoke, dust or burning toast among other things can set off these units. They actually detect particles not formally found in clean air. When a smoke detector trips, it sets off the fire alarm system. BACK TO TABLE OF CONTENTS 25 PAGE 3 TITLE: Fire Plan Fire Extinguishers: All fires have three rings in common, heat, fuel and oxygen supply. To put out a fire, we can use a fire extinguisher to remove at least one of these components: Remove the heat from the fuel. Remove the fuel. Remove the oxygen supply. Fire is classified by its type of fuel: Class A-Combustible solids, i.e. wood, cloth, paper, plastics. Class B-Combustible or Flammable liquids i.e. gasoline, oil. Class C-Live electrical, i.e. electrical equipment that is shorted or arcing. (Fires in small appliances that are connected to wall receptacles are considered Class C fires. If these appliances can be unplugged, then they are considered a Class A fire when disconnected). The four types of fire extinguishers used are: 1. Pressurized Water- Used for Class A fires, this extinguisher can be found in many areas of facility. It can be recognized by the silver colored tank body. This unit contains 2 gallons of water that when applied to a fire, cools the fuel to extinguish the fire. 2. Extinguisher- Used for Class B, C fires, this extinguisher can be recognized by large nozzle and short hose. This extinguisher removes the oxygen from fire to extinguish it. Do not touch the nozzle of this extinguisher when discharging as the CO2 is expelled at a temperature of minus 72 degrees Fahrenheit and can cause frostbite. 3. Halon- Used for Class A, B, C or Class B, C fires (this depends on the size of the extinguisher). Halon extinguishers of nine pounds and greater can be used on any type of fire. Extinguishers of less than nine pounds may only be used on Class B and C fires. Fire Extinguisher Operation- Fire extinguishers operate differently. Operating instructions for your extinguisher are on the nameplate. Read and understand the instructions before an emergency occurs. For most extinguishers, follow these instructions (remember the word PASS): Pull the pin. Most extinguishers first require the user to twist the pin to break the plastic string or cable tie prior to pulling the pin. Care should be taken not to squeeze the handle while attempting to pull the pin out. Aim the extinguisher nozzle, horn or hose at the base of the fire. Hold the extinguisher firmly by the handle provided. BACK TO TABLE OF CONTENTS 26 PAGE 4 TITLE: Fire Plan Squeeze or press both handle together. Start discharging the extinguisher within 6 to 10 feet of the near edge of the fire. Be prepared for the discharge. The contents of the extinguisher are under pressure and the noise of the discharge can be frightening if you don’t expect it. Most extinguishers discharge their contents in 10 to 15 seconds. You are too close if the stream of the discharge scatters the burning materials. Sweep from side to side at the base of the fire until the fire goes out. Shut off the extinguisher. Watch for re-flash and reactivate the extinguisher if necessary. Responsibility for Notification: In the event of a fire, the operator or 911 dispatcher will make notification in the following order: Local Fire Department Local Law Enforcement Agency Fire Prevention: Fire prevention is an essential part of the overall fire plan. Security Services should be responsible for the maintenance and inspections of the fire extinguishers and standpipe hoses. Security should also conduct the required fire drills. The Department of Safety and Engineering will be responsible for the testing and maintenance of the fire alarm systems. The Environmental Services and Purchasing Department shall insure that upholstered furniture, carpet, bedding, window draperies, wall coverings, decorations and other curtains and coverings are purchased, installed and maintained as flame resistant. NFPA 101 and 260B1983 will be used as standards. GENERAL INSTRUCTIONS FOR RESPONSES TO FIRES: RACE: IF THE FIRE IS IN YOUR AREA, STAY CALM-DON’T SHOUT FIRE, USE THE FOLLOWING FOUR STEP PLAN TO NOTIFY AND RESPOND TO A FIRE IN YOUR IMMEDIATE AREA: R.A.C.E. Rescue: Immediate action may be needed to save a life. Move patients in immediate danger and close doors. Yet, do not delay the alarm. Alert: Alert help by pulling the fire alarm and notifying the operator by dialing “0” or 911. *In facilities where the fire alarm stations are unavailable, alert the building occupants dial “0” or 911 and evacuate the building in an orderly fashion BACK TO TABLE OF CONTENTS 27 PAGE 5 TITLE: Fire Plan Confine: Close doors and windows, to prevent smoke spread and to cut off air supply to the fire. Extinguish: If possible with an appropriately rated portable fire extinguisher. If fire is in a Patient Area: Follow procedures spelled out above, remember R.A.C.E. If oxygen shut-down is necessary, the unit’s lead Technologist. Technical Director, or Medical Director will be responsible for approving any shut down of the oxygen system to minimize potential health complications associated with the oxygen shutdown. Know the location of the oxygen valve and what area it serves. If oxygen is necessary to sustain life, use portable tanks. Turn off unnecessary electrical equipment. If you are away from your duty station at the time of an alarm, return to it immediately. Act according to your department fire plan. Check patient rooms to see if they are occupied. Begin with room closest to the fire. If patients are not in their rooms, locate them immediately. If patients must be moved, move them away from the fire. Reassure patients-try not to reveal your own apprehensions. Use phones only when absolutely necessary. Do not use elevators-use stairs. Direct all visitors to the nearest fire exit. Secure records and valuables. Remove to a safe place. If fire is in a Non-patient Area: Follow procedure spelled out above, remember R.A.C.E. Make sure that all people in the area are aware that a fire exists. Pass the word calmly so that a panic situation is not created. When you are sure no one in the fire area, close doors to contain fire and smoke. If irreplaceable records or valuables are near the area of the fire, remove to a secure place. Save what you can but do not take the chance of injury. It is better to save some instead of losing all. If you are away from your department at the time of the alarm, return to it immediately and act according to your department plan. If asked to leave the area by the leader of the fire response team or the leader of the fire department, do so promptly so that the fire-fighting effort is not hampered. BACK TO TABLE OF CONTENTS 28 PAGE 6 TITLE: Fire Plan EVACUATION: The term evacuation is applied to the movement of patients in an emergency. It does not mean emptying the building rather it usually denotes the temporary removal of patients beyond the smoke barrier on the same floor. Move patients to a safe area of refuge until the Fire Department rescue team arrives. This is referred to as a horizontal evacuation. Patients should be kept in their rooms, unless the area is threatened by smoke or flame, at which point, horizontal evacuation begins. Needless evacuation will expose patients to unnecessary handling and anxiety. The strategy is to “Defend in Place”. Since a number of areas of refuge are created on each patient floor by smoke and fire partitions, the need for anything more than horizontal evacuation is remote. In the unlikely event that a vertical evacuation to another floor is required, (as determined by the hospital fire response team or the local fire department) the primary route is to be the stairwells. A. General Patient Evacuation Procedures: There are four (4) stages of evacuation: Evacuate horizontally first, from compartment to compartment (separated by fire doors). Note: the person in charge of the Fire Response Team or Fire Department responding to the scene will authorize the next two steps. Evacuate vertically next. Evacuation to another wing is next. Total evacuation is the final stage, where the entire building is evacuated. Do not evacuate the Facility until instructed to do so by the Fire Personnel or Administrative person in charge. You will be advised as to the relocation area. Rooms are searched for patients starting nearest to the fire or incident. After a room is searched, the door is closed and a pillow is placed in front of the door. NOTE: No one will use the elevators during the emergency except as directed by the Fire Personnel or Administrator in charge. If the fire is in your area, relocate only those patients in the immediate area of the fire. Patients nearest the fire area must be moved first. The leader of the fire Response team or officers of the fire department will advise you. This may be necessary if the involvement spreads from the original area. Reassure all patients that they will be removed to a safe place and that there is no need for fear. Remain calm, work efficiently. Patients able to walk will be wrapped in blankets or bedspreads and taken to corridors to join hands with other patients, single file led by a Staff down the fire exit stairs. Non-ambulatory patients should be evacuated horizontally to a safe area of refuge on the same floor and kept there until the fire department arrives to assist (see your departmental emergency preparedness evacuation plan. For these non-ambulatory patients, wheelchairs and wheeled stretchers may be used for horizontal (lateral) flow. For transporting patients down stairs, the twoperson carry or a blanket fashioned into a stretcher is recommended. BACK TO TABLE OF CONTENTS 29 PAGE 7 TITLE: Fire Plan Emergency Use of Elevators: Employees are instructed not to use elevators during a fire emergency. In some buildings the elevator will be unavailable due to a feature called Fire Recall. If a pull station or smoke detector is activated near the elevator, the elevator will return to a designated floor and stay there until it is released by Security. If the elevators must be used to evacuate non-ambulatory patients vertically, then it should be done with the use of manual override keys. Fire rescue and security personnel are provided with these keys. Such an evacuation must be coordinated through the supervision of the local fire department. Under fire conditions, an elevator can become a death trap for the car occupants. There are three situations in which this can occur: Individuals attempting to escape from a fire floor may find that the smoke detectors on the outside of the elevator doors react to the smoke, preventing the doors from closing or opening, trapping the victims on the fire floor. A descending elevator may be recalled to the fire floor when the hall button controls become short-circuited by the heat of the fire or by water from sprinklers or fire hoses. The door may open on the fire floor and the occupants overcome by the inrush of smoke or toxic gases. Heat or water may short-circuit the control system, and as a result, the elevator may become trapped between floors. Firefighters may have to be diverted from fire-fighting efforts in order to rescue the elevator occupants. The last person or persons to leave the fire or incident area should be: Lead Technologist, Technical Director, the Medical Director or respective designees. Administrator or Designee if applicable. Security Officers if applicable. The corridor doors adjacent to the fire zone should be closed. No one is to re-enter until the area until the All Clear Signal is given by the Fire Department. In the event that a total evacuation of the building is required: All available Security Personnel and Facilities Personnel will physically search the entire building to ensure that all persons have vacated the building. The Fire Marshall. Fire Department or a designee will coordinate the search effort. B. Patient removal Methods: Two Person or Seat Carry: o Two persons carry patient. o Carriers grasp the others wrist under the patient’s knees. o The other arm of each carrier is placed behind the patient’s back and onto the top of the shoulder of the other carrier. Infant and Child Removal: o Place a blanket on the floor. o Place two infants in the same bassinet. o Place the bassinets in the middle of the blanket. BACK TO TABLE OF CONTENTS 30 PAGE 8 TITLE: Fire Plan o Fold the blanket over one end, fold the corners in, and then roll the sides in to form a pocket. o Grasp the folded corners and pull the infants to safety. o Alternatively, place as many children as possible in one crib and pull the crib to the prescribed area. One Person Carries: o Pack Strap Carry – The patient is positioned with their front to the back of the person who will carry them. If sufficient length of bandage or convenient material such as sheets is available, the patient’s hands are tied to allow the rescuer free use of his/her hands. This carry is to move an injured person a short distance when their injuries or conditions are not serious. o Saddle Back Carry – A simple and effective method of moving an injured person a short distance when the injuries or conditions are not serious. Note: In both of these carries, some strength is required, not all employees Will be able to use these carries and therefore they should use their own judgment. Three Person Carry – This carry is often used to carry a severely injured person. o Three people line up on one side of the patient/victim, preferably with the tallest at the shoulders, then at the hips, and the third at the knees. o All three people kneel on the knee nearest the patient’s feet. The person at the patient’s shoulders works his or her hands under the patient’s neck and shoulders; The person at the hips places his/her hands under the patient’s pelvis and hips. The person at the knee is responsible for lifting the knees and ankles. o At the command “LIFT”, usually given by the person at the shoulders, all three persons will lift the patient onto their knees. o At the second command, they are to slowly turn the patient toward them until the patient rests in the bends of their elbows. o At the third command, all three are to rise together to a standing position. NOTE: Although this is a good way to carry a severely injured person, three of your personnel will be used to move such persons. As in all cases of moving victims or patients, the person in charge of the area must take into account the severity of the victim’s injuries, the proximity of that victim to the danger, the total number of victims / patients that need to be moved immediately and the estimated time of arrival of additional help. BACK TO TABLE OF CONTENTS 31 PAGE 9 TITLE: Fire Plan Blanket Drag: o Spread a blanket on the floor alongside the bed, placing one-third of it under the bed and approximately 8 inches extended beyond the patient’s head. o Grasp the patient’s ankles, and move the patient’s legs until they fall at the knee over the edge of the bed. o From the back, encircle the patient with your arms; place your arms under the patient’s armpits and lock hands over the patient’s chest. o Slide the patient slowly to the edge of the bed and lower them onto the blanket. o Taking care to protect the patient’s head, slowly lower the head and upper torso to the blanket and wrap the blanket around the patient. o At the patient’s head, grip the blanket with both hands, one above each shoulder, holding the patient’s head firmly in the 8 inches of the blanket. DO NOT ALLOW PATIENT”S HEAD TO SNAP BACK! o Lift the patient to a half-sitting position and pull the patient to safety. Incline Drag: o Double a blanket lengthwise, place it on the floor parallel and next to the bed, leaving 8 inches extended beyond the patient’s head. o Using suitable means, remove patient from bed to the folded blanket on the floor. o Grasping the blanket above the patient’s head with both hands, drag the patient headfirst to the stairway. o Position yourself on two or three steps lower than the patient, patient’s body inclined upward. o Place your arms under the patient’s arms and clasp your hands over the patient’s chest. o Back slowly down the stairs, constantly maintaining contact with patient, keeping one leg against the patient’s back. BACK TO TABLE OF CONTENTS 32 Policy and Procedure TITLE: Bomb Threat Plan ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: center. Telephone: (502) 387-6133 To establish and maintain procedures for responding to a Bomb Threat to a sleep disorders POLICY: 1.0 General Considerations If a Bomb threat is called into a sleep disorders center this procedure will give the individual(s) who receive the threat a process in which to follow that will assist law enforcement agencies with as much information as possible to assess the seriousness of the threat, determine where the threat originated, how real the threat is, and how to determine if further action is necessary to protect the patients and personnel of the sleep disorders center. PROCEDURE: 1.0 Person receiving original call shall: 1.1 1.2 1.3 1.4 1.5 1.6 Prolong conversation as long as possible. Ask where and when the bomb will explode. Note if the caller indicates knowledge of the center by description of locations. Be alert for distinguishing background noises; i.e. music, voices, machinery, etc. Study voice characteristics. Call 911. BACK TO TABLE OF CONTENTS 33 PAGE 2 TITLE: Bomb Threat Plan 2.0 Duties of the Sleep Center of Kentuckiana Facility Designee. 2.1 Call 911 2.2 Notify the appropriate local law enforcement agencies. 2.3 Notify Administrator on call. 2.4 Notify Technicians. 2.5 Notify Sleep Disorders Center Supervisor On-Call The emergency Preparedness Committee has established the following procedure should a bomb threat occur: If phone call is received: 1. Prolong conversation as long as possible. 2. Ask where and when the bomb will explode. 3. Note if caller indicates knowledge of the hospital by description of locations. 4. Be alert for distinguishing background noises; music, voices, machinery. 5. Study voice characteristics. 6. Tell caller many lives will be lost if the bomb explodes. Ask why they placed the bomb. 7. NOTIFY POLICE 911. 8. Complete Bomb Threat Check Sheet below. 9. Do not discuss the call with others. BOMB THREAT CHECK SHEET Complete as much of the flowing as possible immediately after the telephone call. EXACT MESSAGE AS RECEIVED _____________________________________________________________________________________ _ _____________________________________________________________________________________ _ INFORMATION ON CALLER”S IDENTITY Date of Call_______________ Time of Call__________ Phone # Received On______________________ Name_________________________________________________ Age____________________________ BACK TO TABLE OF CONTENTS 34 Address__________________________________________________________________ Sex_________ Phone_________________________________ Organization____________________________________ BOMB FACTS When will it go off_______________________________________________________________________ Location______________________________________________________________________________ _ Other________________________________________________________________________________ _ CALL WAS (circle one) Internal Outside Local Long Distance Unknown BACKGROUND NOISE (circle any heard) PAGE 3 TITLE: Bomb Threat Plan Office Machines Factory Bedlam Voices Airplanes Animals Street Traffic Music Mixed Trains Other_________________________________________________________________________________ VOICE CHARACTERISTICS (circle all that apply) Tone Speech Language Loud Fast Excellent Distinct Fair Emotional Low Distorted Cursing Raspy Stutter Abusive Nasal Religious Irrational Emotions Calm High Laughing Rational Pleasant COMMENTS:________________________________________________________________________ NAME:__________________________________________________ DATE:_____________________. BACK TO TABLE OF CONTENTS 35 Policy and Procedure TITLE: SEVERE WEATHER ORIGINAL DATE: 3-08-2011 EFFECTIVE DATE: 03-08-2011 REVIEW DATE(s): 03-08-2011 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 I. Purpose: To provide for the safety of patients, visitors, and staff during a severe weather emergency such as ice storms, snowstorms, rain, flooding, etc. II. Policy: Read this entire response guide and review incident management team chart. Use this response guide as a checklist to ensure all tasks are addressed and completed. Implement Emergency Operations Plan and Severe Weather Emergency Response Plan Initiate facility hardening Protect patients, visitors, staff and facility Maintain patient care and medical management Restore normal operations as soon as feasible Immediate (Operational Period 0-2 Hours) III. Procedure: (Incident Commander): Activate the facility Emergency Operations Plan Activate Command Staff and Section Chiefs, as appropriate Establish incident objectives and operational period (Liaison Officer): Notify local emergency management of hospital situation status, critical issues and resource requests Notify local EMS and ambulance providers about the situation and possible need to evacuate or relocate patients Communicate with other healthcare facilities to determine: Situation status Surge capacity Patient transfer/bed availability Ability to loan needed equipment, supplies, medications, personnel, etc. Monitor weather conditions, structural integrity, and facility security. BACK TO TABLE OF CONTENTS 36 Policy and Procedure TITLE: TORNADO PROCEDURES ORIGINAL DATE: 03-08-2011 EFFECTIVE DATE: 03-08-2011 REVIEW DATE(s): 03-08-2011 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 IV. Purpose: This procedure has been developed to assist all employees, patients and visitors in conducting themselves in a safe manner when threatening weather conditions exist that may result in a tornado watch, warning, or an actual occurrence. V. Policy: It is the policy of the Sleep Center of Kentuckiana to provide all employees, patients and visitors with a specific plan of action designed to provide optimum safety in the event of tornado activity. VI. Definitions: A. Tornado Watch- issued when severe thunderstorms and/or tornadoes are most likely to occur. Watches usually cover large geographic area for periods up to six hours. If a tornado watch is issued for your area, continue to monitor information sources. Tornado watches are issued by the National Weather Service and relayed by local media. The term “watch” means that weather conditions in the area are such that a tornado could develop. B. Warning-A Funnel shaped cloud or a tornado has been sighted in the area. When a tornado warning is issued, take shelter immediately. VII. Procedure: 1- Non- Clinical Area A. Close all windows, blinds and drapes in the area. B. Move away from windows, either to an interior wall or, preferable a hallway. C. Make only emergency telephone calls until the “ ALL CLEAR” is given D. Remain calm and remain in your area unless called to assist in another area. 2- Clinical Area A. Close all windows, blinds and drapes in the area. B. Have ambulatory patients assemble in an inside hallway. BACK TO TABLE OF CONTENTS 37 PAGE 2 TITLE: TORNADO PROCEDURES C. D. E. F. Move all occupied beds as far from windows as possible. Use blankets to cover patient as well as possible. Make only emergency telephone calls until “ALL CLEAR” is given. Patient in beds are moved into hallways or evacuated to other parts of the Facility only when directed to do so by the incident Commander, in response to immediate danger or, actual damage. G. Stay calm. The “Weather Alert” does not necessarily mean that the Facility is in the direct path of the tornado, only that a tornado has been sighted in the area. 3. The Facility Administrator-on- call will evaluate the need to activate the emergency Preparedness Plane. 4. Anyone who is injured will be treated in the Emergency Department, or alternative area as decided by the Incident Commander. 5. If evacuation becomes necessary, the Incident Commander and Emergency Preparedness Coordinator will coordinate activity with local Hospitals, local Emergency Operations Center, and ambulance services. 6. After the danger has passed, Weather Radio to announce. 7. If a tornado touches down, severe damage will result including downed power lines fractured gas lines, and broken water pipes. Be cautious in any area hit by a tornado for these hazards. 8. Heavy hail and rainfall often accompany tornadoes. Hail damage and flash flooding are definite risks following a tornado. BACK TO TABLE OF CONTENTS 38 Policy and Procedure TITLE: EARTHQUAKE ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 Policy When you feel an earthquake, duck under a desk or sturdy away from windows, bookcases, file cabinets, heavy mirrors, hang plants, and other heavy objects that could fall. Watch out for falling plaster and ceiling tiles. Stay undercover until the shaking stops and hold onto your cover. If it moves, move with it. Here are some additional tips for specific locations: If you are in a HIGH- RISE BUILDING, and not near a desk or table, move against an interior wall and protect your head with your arms. Do not use the elevators. Do not be surprised if the alarm or sprinkler systems come on. Stay indoors Glass windows can dislodge during the quake and sail for hundreds of feet. If you’re OUTDOORS, move to a clear area away from trees, signs, buildings, electrical wires and poles. If you’re on a sidewalk near a building, duck into a doorway to protect your self from falling bricks, glass plaster, and other debris. If you’re driving, pull over to the side of the road and stop. Avoid overpasses, power lines, and other hazards. Stay inside the vehicle until the shaking is over. If you’re in a crowded room, or other public place, do not rush for exits. BACK TO TABLE OF CONTENTS 39 Policy and Procedure TITLE: Emergency Contact ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s):03-01-2007, 3-08-2011 REVISION DATE(s): 03-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 To establish and maintain procedures for responding to both external and internal disasters which place extraordinary demands upon the sleep facility personnel and facilities. POLICY: The sleep disorders center maintains plans for external and internal emergencies. PROCEDURES: 1.0 EXTERNAL DISASTER PLAN 1.1 While the entire Sleep Center of Kentuckiana may be affected by the response to a disaster, the following procedure will be followed: Call 911 Environmental Services Sun Property (502)894-9083 Contact the poisoning center if needed (502)589-8222. Contact the closest emergency department Aubudan Hospital (502)636-7111. Contact urgent care physician or center in the first floor of our building. Inform Sleep Center administration o President Edward Dana (502)387-6133. o Medical Director Kheder Kutmah (859)992-4660. o Clinical Coordinator Contessa Tyler (502)298-8279. o Management Team Rana Dana (502)994-6897 Tina Bratcher (502)345-1226. o . Medical Staff o Technicians and assistant technicians: Mark Nunez (270)317-7714. Mecca Schmitz (502)671-3967 Sarah Ford (502)291-2995. James Thornton (270)317-7503. BACK TO TABLE OF CONTENTS 40 Page 2 TITLE: Disaster Plan 2.0 Plan Director. Staff and House Officers on call. Administration. Admitting Office. Patient Transport. Facilities. Medical Records. Head Technician. A complete copy of the external disaster plan is provided in the Safety Manual. Initial orientation and continuing education of employees involved with the disaster plan is the responsibility of the respective department heads. INTERNAL DISASTER PLAN: 2.1 Implementation: A command team consisting of the Medical Director or his designee, Administrator on call, Security Manager and Chairman of the Safety Committee will make the decision to implement the Internal Disaster Plan. 2.2 A Medical Center / building command post will be established in the Emergency Department office suite if functional. An alternate site will be designated if the first site is not available. 2.3 While the entire Sleep Center of Kentuckiana may be affected by the response to a disaster, the following procedure will be followed: Call 911 Environmental Services. Contact the poisoning center if needed. Contact the closest emergency department. Contact urgent care physician or center in the first floor of our building. Inform Sleep Center administration o President Edward Dana (502)387-6133. o Medical Director Kheder Kutmah (859)992-4660. o Clinical Coordinator Contessa Tyler (502)298-8279. o Management Team Rana Dana (502)994-6897 Tina Bratcher (502)345-1226. Medical Staff o Technicians and assistant technicians Mark Nunez (270)317-7714. Mecca Schmitz (502)671-3967. Sarah Ford (502)291-2995. James Thornton (270)317-7503. BACK TO TABLE OF CONTENTS 41 Page 3 TITLE: Disaster Plan 2.4.4.1 Termination: When disaster response personnel are no longer needed, the Plan Director will advise staff to announce “Disaster now over-all facility personnel may return to routine duties.” Policy and Procedure TITLE: Emergencies and Responses ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 POLICY: To provide established guidelines to follow when emergency situations occur during the performance of diagnostic polysomnographic evaluations. PROCEDURE: 1.0 Guidelines for emergencies during a sleep study to ensure safety and care of patients. 1.1 If there is any question of patient safety, call the sleep disorders center (SDC) Medical Director: Dr. Kheder Kutmah (859)992-4660. BACK TO TABLE OF CONTENTS 42 1.2 The polygraph recording will continue during the emergency uninterrupted. Disconnect head box immediately prior to defibrillation. Emergency Situation Response Chest pain, neck, jaw or arm pain Call SCK Medical Director: Dr. Kheder Kutmah (859)992-4660. Mild to moderate difficulty breathing Call SCK Staff Physician: Dr. Azmi Draw (502)216-0191. Severe difficulty breathing Call emergency by dialing 911 or Call medical director: Dr. Kheder Kutmah (859)992-4660. Seizures without cardiac arrest Turn patient on side in case of vomiting. Call Sleep Center Medical Director: Dr. Kheder Kutmah (859)992-4660. Headache-moderate to severe Call Medical Director: Dr. Kheder Kutmah (859)992-4660. Symptoms of stroke, i.e., paralysis Weakness of limbs, difficulty speaking, difficulty comprehending Emergency Situation Nausea/vomiting Call 911 Response Call Medical Director: Dr. Kheder Kutmah (859)992-4660. Page 2 TITLE: Emergencies and Responses Fall/Injury Change in behavior, i.e., agitation Hostility, Anxiety Suicide ideation SPO2 below 80% on 4 L per minute of oxygen Call night supervisor, administration And Notify referring physician Clinical Coordinator: Contessa Tyler (502)298-8279. Call Medical Director: Dr. Kheder Kutmah (859)992-4660. Call Clinical Coordinator: Contessa Tyler (502)298-8279. Call Medical Director: Dr. Kheder Kutmah (859)992-4660. Notify night supervisor or Security Wake up patient Notify SDC Medical Director: BACK TO TABLE OF CONTENTS 43 Asystole of 5 seconds or more Ventricular tachycardia for 10 Dr. Kheder Kutmah (859)992-4660. Check patient (Tech 1 will check patient and start CPR if Applicable, Tech 2 will Call emergency dialing 911 and inform Medical director: Dr. Kheder Kutmah (859)992-4660. Check patient (Tech 1 will check patient and start CPR if Applicable, Tech 2 will Call emergency dialing 911 and inform Medical director: Dr. Kheder Kutmah (859)992-4660. Seconds or more Runs of PVCs (6 or more) occurring 3 or more times Page 3 TITLE: Emergencies and Responses Symptomatic tachycardia 120 bpm or more over a minute or more, or not associated with periods of apnea Symptomatic bradycardia less than 40 BPM over a minute or longer, or not associated with periods of apnea Wake up patient Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Wake up patient Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Wake up patient Check Patient check EKG patients and electrodes. Call 911 Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. No EKG activity Check patient –Inform medical director Call emergency by dialing 911 if applicable begin CPR Parasomnia mobility (sleep walking, Active night terrors) Pediatric Emergency Situations Maintain patient safety Call and inform medical director. Response BACK TO TABLE OF CONTENTS 44 SP02 falls below 70% with periods of apnea Wake up patient, Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. SP02 falls below 70% for 120 sec. or more Wake up patient, Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Check patient Call emergency by dialing 911 if applicable begin CPR Call medical director: Dr. Kheder Kutmah (859)992-4660. Wake up patient Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Asystole of 5 seconds or more Ventricular tachycardia for 10 sec. or more Runs of PVCs (6 or more) occurring 3 or more times Tachycardia over a minute or more, or not associated with periods of apnea Bradycardia less than 60 bpm over a minute or more, or not associated with periods of apnea Page 4 TITLE: Emergencies and Responses Non Emergency Wake up patient Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Wake up patient Call SDC Medical Director: Dr. Kheder Kutmah (859)992-4660. Wake up patient Call SDC Medical Director: Response PSG not completed due to equipment malfunction or other problems Contact Sleep Center Clinical Coordinator: Contessa Tyler (502)298-8279. Call Tech Support at Respironics: (800)345-6443. Medical Records Documentation: Document incident in comments or observations section of acquisition equipment as well as on paperwork. Complete report of incident is required. BACK TO TABLE OF CONTENTS 45 Policy and Procedure TITLE: Psychiatric/ Belligerent Emergencies ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: SUBJECT: Psychiatric Emergencies PURPOSE: To recruit assistance in preventing a non-armed, belligerent, agitated, confused, and/or combative person from causing injury to self or staff of the Sleep Disorders Center. BACK TO TABLE OF CONTENTS 46 POLICY STATEMENT: To establish guidelines for the Facility for any sudden, violence or threatening behavior for which immediate help is needed top reserve the safety of the Facility staff and the patients. KEY POINT: In the event the individual is known to be armed, call 911. 911 is not to be called for individuals leaving against medical advice, or for individuals who are not physically threatening to staff or injury to them self. PROCEDURE: 1. Assess the situation 2. If help is needed call Medical Director Dr. Kheder Kutmah at (859)992-4660 and give a brief description of the situation. 3. If suicide call the 24 hours crisis and into line (502)589-4313. 4. In the event an injury occurs to the patient, or staff a reportable event form is completed employees report to the Emergency department. 5. Responders are released when 911 officer and sleep center staff agree that the situation is under control. ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Infection Control EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To insure the safety of sleep disorder center staff and patients by controlling the spread of infection. POLICY: Universal Precautions and Blood borne Pathogen Standards will be followed when caring for patients. BACK TO TABLE OF CONTENTS 47 PROCEDURE: 1.0 Universal Precautions. 1.1 Wash hands before and after contact with each patient during hookup, the polysomnographic evaluation, and removal of electrodes. 1.2 2.0 Gloves, when used, should be disposed of after contact with each patient. Infectious conditions. 2.1 Document infectious conditions. 2.1.1 Review patient questionnaire and medical records. 2.1.2 Information obtained while talking with the patient during the hook up procedure. 2.2 3.0 Laundry. 2.2.1 Bag laundry according to facility protocol. Sharps container. 3.1 3.2 Blunt tip needles used to applying electrode gel to EEG electrodes. Needles used by patients for self-injections, i.e. insulin. Page 2 TITLE: Infection Control 4.0 Personal Protective Equipment (PPE). 4.1 5.0 Single use supplies. 5.1 6.0 Instruct staff to location of PPE in the facility. Dispose of single use supplies, i.e. nasal cannulas, stick on electrodes, etc. after removed from patient in a trash can in the patient room. Multiple use sensors and supplies. 6.1 Clean with an agent such as Control III or Sporiciden according to manufacturer recommendations. BACK TO TABLE OF CONTENTS 48 6.2 7.0 Designate separate location for clean and dirty sensors and supplies. Safety and Infection Control in-service. 7.1 New employee orientation yearly thereafter. 7.2 Maintain log of date and attendees. Policy and Procedure TITLE: Cleaning and Maintenance of Equipment and Facilities ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 A routine schedule for the cleaning and maintenance of equipment and facilities helps to assure the accurate and continued operation and reduces infectious risks to patients and technologists. POLICY: BACK TO TABLE OF CONTENTS 49 1.0 General Considerations: 1.1 The sleep disorders center should be cleaned routinely. Preventative maintenance checks on all equipment will be performed in compliance with regulations pertaining to operating a sleep disorders center following manufacturer’s specifications and Occupational Safety and Health Administration (OSHA) requirements. Procedure: 1.0 Daily cleaning of sleep disorders center. 1.1 Floor. 1.2 1.3 Clean and disinfect restroom(s). 1.2.1 Re-stock paper supplies. 1.2.2 Re-fill soap dispensers. Empty trash. 1.3.1 Damp cleans the containers. 1.3.2 Line containers. PAGE 2 TITLE: Cleaning and Maintenance of Equipment and Facilities 2.0 3.0 1.4 Make beds in patient rooms. 1.5 Clean sinks. 1.6 Dust counter and / or desktops. Weekly cleaning of sleep disorders center. 2.1 Damp dust desks, phones, counters, filing cabinets, and office equipment. 2.2 Polish any wood furniture with wood polish. As needed cleaning of sleep disorders center. BACK TO TABLE OF CONTENTS 50 3.1 4.0 Wash windows. Maintenance of equipment. 4.1 Annual routine visual inspection made. 4.1.2 Preventative maintenance checks are required for all equipment. 4.1.3 Frequency of evaluations is mandated by local regulatory agencies. 4.2 Documentation of preventative maintenance checks will be filed for reference. Policy and Procedure TITLE: Cleaning and Maintenance of Reusable Sensors and Interface Devices ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: A routine schedule for the cleaning and maintenance of sensors and patient interface devices helps to assure the accurate and continued operation of equipment and reduces infection risks to patients and technologists. BACK TO TABLE OF CONTENTS Telephone: (502) 387-6133 51 POLICY: 1.0 General Considerations 1.1 The sleep disorders center director is responsible for developing proper maintenance and cleaning of equipment policies and procedures consistent with manufacturer’s specifications, state and local health policies, and Occupational Safety and Health Administration guidelines. PROCEDURE: 1.0 Reusable Patient Sensors and Interface Devices 1.1 Equipment cleaning area should have separate areas for dirty and clean sensors and interface devices. 1.2 use. All reusable patient sensors and interface devices are cleaned after each 1.3 All reusable patient sensors and interface devices should be cleaned with an Occupational Safety and Health Administration / Environmental Protection Agency approved disinfectant in a method that is compliant with the manufacturer’s specifications and your sleep disorders center’s policies. PAGE 2 TITLE: Cleaning and Maintenance of Reusable Sensors and Interface Devices 2.0 3.0 Examples of reusable patient sensors and interface devices: 2.1 Electrodes 2.2 Respiratory monitoring devices 2.3 PAP interface, accessories and tubing 2.4 Snoring sensors 2.5 Oximeter probes SINGLE USE PATIENT SENSORS AND INTERFACE DEVICES BACK TO TABLE OF CONTENTS 52 3.1 Single patient use devices are intended for one time use and are to be discarded appropriately. These devices are usually labeled as single use by the manufacturer on the packaging. 3.1.1 Examples of single patient use sensors and interface devices: 3.1.1.1 Nasal oxygen cannulas. 3.1.1.2 Electrodes, oximeter probes, flow sensors, etc. sold as single patient use only. ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Hazardous Materials EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To establish a specific procedure for the use, storage and clean up of any hazardous materials used in the sleep disorders center to assure the safety of patients and staff. BACK TO TABLE OF CONTENTS 53 POLICY: All sleep disorders center staff will follow approved standards when using hazardous materials. PROCEDURE: 1.0 Material Safety Data Sheets (MSDS) 1.1 2.0 MSDS information for all hazardous materials are located in this section of the policy and procedure manual. Hazardous materials. 2.1 List all hazardous materials. (This is not meant to be an all-inclusive list.) 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.2 PAGE 2 TITLE: 3.0 Insure all hazard materials are appropriately labeled. Hazardous Materials Storage 3.1 4.0 Acetone. Dispatch. Disinfecting solutions. Colorox wipes. Alcohol. Bleach. Flammable materials. 3.1.1 Stored in a flammables metal cabinet or equivalent storage container. 3.1.2 Stored according to Occupational Safety Health Administration and state requirements. Spills of hazardous materials used in the sleep disorders center. BACK TO TABLE OF CONTENTS 54 4.1 Refer to MSDS information for each hazardous material. ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Latex Sensitivity EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To outline procedures for avoidance of latex contact in specifically identified patients and employees. BACK TO TABLE OF CONTENTS 55 POLICY: Exposure to products and/or equipment containing latex will be minimized in patients and staff with known or suspected sensitivity to such products. PROCEDURE: 1.0 Identification of persons at risk. Inpatients with known latex sensitivity as identified in patient’s chart. 1.2 Outpatients will be questioned about latex sensitivity prior to the hookup. 1.3 Technologists with known or suspected latex sensitivity should notify their supervisor. 2.0 Precautions. 2.1 Remove latex items from the monitoring room of sensitive patients. 2.2 Substitute item or sensor routinely used with non-latex item or sensor. Read description of item or sensor from the manufacturer. Examples include: 2.2.1 Gloves. 2.2.2 Electrode wires. 2.2.3 Snap on electrodes. 1.1 PAGE 2 TITLE: Latex Sensitivity 3.0 2.2.4 PAP interface. 2.2.5 Tape. Identification after hookup. 3.1 Patient has reaction to a latex item or sensor used during hookup or polysomnogram. 3.1.1 Skin reddening or rash. BACK TO TABLE OF CONTENTS 56 3.1.1.1 Change to non-latex item or sensor. 3.1.1.1.1 Determine if reaction is such that patient can continue with study. 3.1.1.1.1.1 If patient is able to continue with study and document the situation on the patient summary form. Monitor patient closely. 3.1.1.1.1.2 If patient is unable to continue with study, disconnect the patient and contact supervisor. Carefully document the situation on the patient summary form. 3.1.2 Bronchospasm or laryngeal edema anaphylaxix 3.1.2.1 Activate EMS per facility protocol 3.1.2.2 Notify supervisor after EMS personnel have arrived. Policy and Procedure TITLE: Polysomnographic Montages ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 Standardized polysomnographic montages provide for consistency of recordings and accuracy of analysis for interpretation of sleep study data. BACK TO TABLE OF CONTENTS 57 POLICY: Procedures performed use standard montages, which meet published guidelines and requirements. PROCEDURE: 1.0 Diagnostic polysomnographic montage should include 1.1 EOG LEOG-M2 REOG-M1 1.2 EEG C3-M2 C4-M1 O1-M2 O2-M1 F3 -M2 F4- M1 1.3 EMG Chin 1 – Chin 2 Left Anterior Tibialis Right Anterior Tibialis Snore 1.4 ECG Lead I or II placement PAGE 2 TITLE: Polysomnographic Montages 1.5 1.6 1.7 1.8 2.0 Airflow Nasal/Oral flow Airflow Pressure Transducer Nasal / Oral flow Air flow C02 Nasal/ Oral flow Respiratory effort Chest Abdominal Position Body position Oxygen saturation Oximetry PAP Titration Montage BACK TO TABLE OF CONTENTS 58 3.0 4.0 2.1 Includes 1.1 – 1.8 2.2 PAP flow PAP device 2.3 PAP pressure PAP device or manual input per acquisition equipment requirements. MSLT and MWT Montage 3.1 EOG LEOG – M2 REOG – M1 3.2 EEG 3.3 EMG C3 – M2 C4 – M1 O1 – M2 O2 – M1 F3- M2 F4- M1 Chin – Chin 3.4 ECG Lead I or II placement Filter Settings 4.1 EOG 4.1.1 LFF = 0.3 Hz PAGE 3 TITLE: Polysomnographic Montages 4.2 4.3 4.1.2 HFF = 30-35 Hz 4.1.3 EEG 4.2.1 Sensitivity = 50 u V/cm 4.2.2 HFF = 30 – 35 Hz 4.3.3 Sensitivity = 50 u V/cm LFF = 0.3 Hz EMG BACK TO TABLE OF CONTENTS 59 4.4 4.5 4.3.1 LFF = 10 Hz 4.3.2 HFF = 70 – 100 Hz 4.3.3 Sensitivity = 50 V/cm ECG 4.4.1 LFF = 1.0 Hz 4.4.2 HFF = 15 Hz 4.4.3 Sensitivity = 1 MV/cm Airflow and respiratory effort 4.5.1 LFF = 0.1 Hz 4.5.2 HFF = 1.0 Hz 4.6 4.5.3 Sensitivity = 50 uV/cm 60 cycle filter is recommended “out” but can be “in” as necessary to eliminate 60 cycle artifact that cannot otherwise be identified and eliminated. 4.7 Alternative settings for LFF PAGE 4 TITLE: Polysomnographic Montages 5.0 4.7.1 Setting LFF to 1.0 will attenuate the slow rolling eye movements in the EOG and the delta waves in the EEG. Direct Current (DC) amplifier 5.1 Used to record slower moving potentials using a fixed linear scale. 5.1.1 Oximeter 0 – 100% 5.1.2 5.1.3 5.1.4 PAP Device pH monitor Pressure transducer 0 – 20 cm H2O BACK TO TABLE OF CONTENTS 60 Policy and Procedure TITLE: Patient Arrival, Preparation and Electrode / Sensor Application ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: BACK TO TABLE OF CONTENTS 61 PURPOSE: To provide standard methods to prepare the patient for polysomnographic recording and to identify standard procedures for application of electrodes and sensors to ensure consistency of pre-evaluation routine among sleep disorders center technicians and technologists. POLICY: Technicians and technologists will follow the standard methods for welcoming the patient to the sleep disorders center and applying the electrodes and sensors according to the montage of the evaluation ordered by the referring physician. 1.0 10/20 Hookup Protocol Statement of Purpose It is the policy of The Sleep Center of Kentuckiana to provide a standard electrode set-up for the technicians. This will ensure the acquisition of quality recorded data for the Sleep Physicians to diagnose and treat patients. DESCRIPTION: * Measure from nasion to inion * Measure from right pre-auricular to left pre-auricular point. * Ground electrode (Fp) is in the middle of the forehead - 10% from nasion. Page 2 TITLE: Patient Arrival, Preparation and Electrode / Sensor Application * Cz is the 50% point between nasion and inion and the 50% point between the left and right pre-auricular points. * T3 is 10% up from the left pre-auricular point. * T4 is 10% up from the right pre-auricular point. * C3 is 20% up from T3 or 20% down from Cz * C4 is 20% up from T4 or 20% down from Cz BACK TO TABLE OF CONTENTS 62 * Measure the circumference of the head from Fp to Fp running through T3, T4 and O1, O2. * Oz is 10% up from the inion and 50% of the circumference measurement. * O1 is 5% to the left of Oz * O2 is 5% to the right of Oz * Fp1 is 5% to the left of Fp * Fp2 is 5% to the right of Fp * F3 is 20% left from FPI *F4 is 20% right from FP2 * Double Check - C3 should be 50% between Fp1 and O1 * C4 should be 50% between Fp2 and O2 2.0 Patient Hook Up Procedure It is the policy of The Sleep Center of Kentuckiana to use the International 10-20 measurement and placement system for polysomnographic EEG electrode placement. “Visualized” or “estimated” electrode placement is not permitted. Remaining electrodes are applied maintaining a consistent and uniform technique. Page 3 TITLE: Patient Arrival, Preparation and Electrode / Sensor Application A. Patient hook up will be done in the patient’s room. Turn camera on and start recording prior to hookup and till electrodes are removed the next morning. B. Electrode Application * Be sure to use skin prep on all areas which will receive an electrode. Nu- prep is to be used on EEG areas. Be careful not to get it into patient’s eyes. BACK TO TABLE OF CONTENTS 63 * Plug each electrode lead wire into terminal box after placing electrode on patient. Doing one at a time will help prevent getting wires mixed up. * After attaching electrodes they should then be checked for proper impedance. Do this by pressing “the impedance icon” and following directions on the screen. C. Types of Electrodes * Grass electrodes - these are filled with electrode cream and then placed on a folded 2 x 2 gauze pad with additional electrode cream for EEG placement. * Pellett / Contour electrodes - attach these pre-adhesive pads to lead wire snap. Then attach electrode to patient in appropriate spot. This will ensure that patient will not be bruised by pushing on the already attached electrode with lead wire. D. Electrode Placement * Ground - This should be your first sensor hook-up. It goes on the mid forehead and is plugged into the patient ground slot on the terminal box. Use a grass electrode here. Page 4 TITLE: Patient Arrival, Preparation and Electrode / Sensor Application * Head (EEG) - Mark scalp electrode sites using International 10 – 20 system. Clean each electrode site with Nu- prep and then Skin Prep pad. Apply a small amount of Elefix cream to a 2 X 2 gauze pad. Next fill a Grass electrode with Elefix cream. Place this electrode in the cream on the gauze, with the cup side of electrode pointed up. With the wire directed towards the top of the head, place the cream filled cup on the prepared site pressing the cup to the surface of the scalp. BACK TO TABLE OF CONTENTS 64 E. Electrode Placement (cont) * Mastoid (reference A1, A2) - One electrode is placed on the mastoid bone directly behind each ear. These are used as reference channels for brain waves and eye movement channels. * Eyes (LOC/ROC) - The right EOG should be placed 1 cm out and 1 cm up from the right outer canthus of the eye. The left EOG should be placed 1 cm out and 1 cm down from the left outer canthus of the eye. * Chin EMG - Three electrodes are used to monitor chin muscle movement. One is placed on the center of the chin. The other two are placed one on each jawline, equal distance apart. If the patient has a beard it is acceptable to place all three electrodes under the chin (This allows patient to keep his beard). An alternative method with a full beard, would be using cream and gauze with Grass sensors, as on EEG leads. * EKG - Three electrodes are used to monitor the Heart. One electrode is placed just below the clavicle on each side of chest. The other electrode is placed at V6. * Leg EMG - Two electrodes, about 1 cm apart, are placed on each leg to monitor leg muscle movement at the anterior tibialis muscle. Shave area to rid hair if needed prior to placement. * Pull all lead wires (except leg EMG) into a ponytail at the crown of the patient’s head. Gently twist wires and Coban together. Go down about 15 inches and Coban again. Page 5 TITLE: Patient Arrival, Preparation and Electrode / Sensor Application F. Other Sensors * Respiratory Effort Belts - Place Thoracic Belt such that it runs directly under the patient’s arm pit (This belt has velcro on it). Place Abdominal Belt such that it runs over large part of stomach. BACK TO TABLE OF CONTENTS 65 * Airflow Sensor - Position on patient’s face between upper lip and nose. The two tabs should be slightly bent upward in front of nares. The other tab should be slightly bent down towards mouth. * Position Sensor - Place on Thoracic Belt with wire towards the top of the belt. * Micro - Apply adhesive pad to sensor and then place on side of patient’s neck. * SaO2 - Apply adhesive strip to Oximeter sensor and place on patient’s finger. Wrap with Coban. G. Final Preparation * When all electrodes and sensors have been attached to the patient and the connectors inserted into the Patient Box, attach the cable from the Patient Box to the top side of the Alice 5 unit. * Impedance Check - The electrode impedance should be less than 5K ohms. To check the impedance press Impedance icon prior to the acquisition. Head box will appear: follow directions on screen. Any electrode higher than 5K should be rescrubbed and reapplied. * Main cable can now be disconnected and patient may watch TV prior to lights out. Page 6 TITLE: Patient Arrival, Preparation and Electrode / Sensor Application 3.0 Bundle electrodes. 3.1 4.0 The leads may need to be grouped loosely together as in a ponytail fashion at the top of the head for comfort of the patient. Head box. BACK TO TABLE OF CONTENTS 66 4.1 5.0 Place all electrode wires and sensor connections into the head box according to the montage. Prepare for acquisition. 5.1 Assist the patient into bed helping with the electrode wires and the head box. TITLE: Patient Arrival, Preparation and Electrode / Sensor Application 5.2 6.0 Instruct patient how to reach technician after acquisition has started. Perform a physiological calibration. Policy and Procedure TITLE: Physiological Calibration Procedures ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Medical Director SIGNATURE: TITLE: President BACK TO TABLE OF CONTENTS 67 PURPOSE: To conduct standard maneuvers that insures the quality of the recorded signal for reference while scoring the polysomnogram. POLICY: All equipment required for sleep study testing that requires calibration must be properly calibrated both prior to the study recording and after each study. All calibration signals must be recorded and stored. Both machine calibrations and physiologic calibrations must be performed. PROCEDURE: 1.0 2.0 Machine Calibrations 1.1 Per polysomnographic recording equipment and oximeter manufacturer guidelines. 1.2 Refer to equipment calibration policy. Physiological Calibrations 2.1 After the polysomnogarphic recording equipment has been calibrated and the Patient Arrival, Preparation and Electrode / Sensor Application policy has been completed 2.1.1 Instruct the patient to lie supine through the calibration procedure. 2.1.2 Assure the patient that all instructions will be repeated as needed. 2.1.3 Follow the response to each command, check the quality of the signal and make adjustments as necessary: 2.1.3.1 To the electrodes, thermistor, or belts. 2.1.3.2 To the sensitivity, gain, polarity or filter settings. PAGE 2 TITLE: Physiological Calibration Procedure 2.1.3.3 3.0 To replace electrodes. Patient Calibration Instructions Type instructions on the computer screen or write on paper recording as the patient is instructed to perform the calibration procedures. Give the instructions slowly and clearly. 3.1 E/C Eyes Closed for 15 to 30 seconds BACK TO TABLE OF CONTENTS 68 3.2 E/O 3.3 E/C 3.4 LR 3.5 LL 3.6 LR 3.7 LL 3.1.1 Ask the patient to close their eyes and look straight ahead. Eyes Open for 15 to 30 seconds 3.2.1 Ask the patient to open their eyes and look straight ahead. Eyes closed for 15 to 30 seconds 3.3.1 Ask the patient to close their eyes and look straight ahead. Look Right 3.4.1 Ask the patient to keep their eyes closed and without moving his/her head look to the right then back to the center. Look Left 3.5.1 Ask the patient to keep their eyes closed and without moving his/her head look to the left then back to the center. Look Right 3.6.1 Ask the patient to keep their eyes closed and without moving his/her head look to the right then back to the center. Look Left 3.7.1 Ask the patient to keep their eyes closed and without moving his/her head look to the left then back to the center. PAGE 3 TITLE: Physiological Calibration Procedures 3.8 LU Look Up 3.8.1 Ask the patient to keep their eyes closed and without moving his/her head look up then back to the center. 3.9 LD Look Down BACK TO TABLE OF CONTENTS 69 3.9.1 3.10 BLNX Ask the patient to keep their eyes closed and without moving his/her head look down and back to the center. Blink eyes 3.10.1 Ask the patient to blink his/her eyes 5 times. 3.11 JAW Bite Down on Jaw 3.11.1 Ask the patient to bite down on jaw or clench the teeth. 3.12 SNORE Snore Sound 3.12.1 Ask the patient to simulate a snore sound or clear throat. 3.13 FLEX Flex Foot 3.13.1 Ask the patient to point and flex each foot separately. The foot should be non-weight bearing Tag each leg separately on recording. Repeat 2 times on each leg. 3.14 IN/OUT Breath in and out PAGE 4 TITLE: Physiological Calibration Procedures 3.14.1 3.15 Ask the patient to breath normally and then on your instruction take breaths in and out. Mark the record IN and OUT accordingly. HOLD Take in breath and hold BACK TO TABLE OF CONTENTS 70 3.15.1 Ask the patient to breath normally and then on your instruction take in a breath and hold it for 10 seconds (to a count of 10), then resume normal breathing. 3.16 MUELLERS Mueller’s maneuver 3.16.1 Ask the patient to hold breath and try to take 5 breaths against a closed airway, then resume normal breathing. 4.0 Perform Patient Calibration 4.1 Begin LIGHTS OUT or LIGHTS ON procedure. 4.1.1 If physiological calibrations are instructed with an intercom, instruct patient to move to a comfortable sleeping position and go to sleep. The door to the patient’s room should have been closed while the patient calibrations were given. Remind the patient that the technician is readily available and if the patient should need anything to call the technician. 4.1.2 If physiological calibrations were instructed without and intercom, go to the patient’s door and instruct the patient to move to a comfortable sleeping position and go to sleep. Remind the patient that the technician is readily available and if the patient should need anything to call the technician. Close the door when you leave the room. Policy and Procedure TITLE: Calibration of Equipment for Polysomnogram ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 BACK TO TABLE OF CONTENTS 71 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURPOSE: To document functionality of diagnostic equipment, to document the proper filter settings and uniform signal responses essential for accurate and thorough diagnosis, and to maintain the integrity of the polysomnographic recording throughout the study. This procedure is sometimes referred to as “equipment calibrations” or “machine calibrations”. POLICY: All equipment used for patient monitoring is to be calibrated for functionality using standard settings. 1.0 General Considerations 1.1 Calibration for digital acquisition equipment is generally performed by internal software using a known calibration signal. Refer to the manufacturer’s manual for details. 1.2 Calibration procedures include the testing of all ancillary equipment. 1.3 All equipment calibrations are to be conducted prior to the arrival of the patient to allow for troubleshooting or equipment replacement. 1.4 Calibration procedures are to be documented on the polygraph. Identify signal derivations, filter settings, and calibration voltages. Page 2 TITLE: Calibration of Equipment for Polysomnogram 1.01 Introduction to Calibrations (e.g., Alice5 software) BACK TO TABLE OF CONTENTS 72 Statement of Purpose Regularly scheduled calibrations are an essential part of maintaining laboratory performance. Calibrations covered in this document include: peripheral device (CPAP/BiPAP®; oximeter) calibrations, machine calibrations, and physiological calibrations. Peripheral devices calibrations The oximeters and PAP devices in use at the Sleep Disorder Center all have a linear analog output. This means that: the lowest measurement the device makes (i.e., 0% or 0cm) corresponds to the device’s lowest output voltage (typically, 0V), the highest measurement the device makes (100% or, say, 20cm) corresponds to the device’s highest output voltage, and all in-between values can be plotted on a straight line defined by the lowest and highest output voltages. For example, if 0V corresponds to 0% SaO2 and 1V corresponds to 100%, then 0.8V will correspond to a blood oxygen level of 80%. The oximeter’s analog output will be 0.8V whenever the patient’s blood oxygen level is measured to be 80%. Because the relationship between measurement and output voltage is linear, whatever difference exists between the device and Alice will be the same through the whole range of values. E.g., if an oximeter is reading 98% and Alice is reading 96%, Alice will misreport a desaturation to 84% as a desaturation to 82%. In this instance, Calib400, the calibration program found in the AL3 subdirectory, can be used to “tell” Calvin to add .02V (corresponding, of course, to 2%) to the voltage it receives on the SaO2 channel. The calibration procedure, which is a 2-person process, is described in the Calibration of DC Signals Protocol. Each auxiliary device calibrated, record the date of calibration and your initials in the (Calibration) Log. Page 3 TITLE: Calibration of Equipment for Polysomnogram Machine calibrations BACK TO TABLE OF CONTENTS 73 On a standard polygraph, each signal passes through an amplifier which amplifies and filters the signal and allows the technician to specify what size pen deflection (measured in mm) a given input voltage (measured in V) will cause (sensitivity). Alice is not nearly as complicated: there are no pens, no shifting baselines, and state-of-the-art hardware and software make daily meticulous measurements and dialflipping a thing of the past. However, Calvin amplifiers should be checked periodically to ensure that they are continuing to work properly. By recording a calibration signal for EEG, EOG, EMG, and ECG channels at both the beginning and the end of a study, we demonstrate the integrity of each of these channels for the duration of the study. Basically, all like signals (e.g., all EEG channels) should look the same. If they do not, something is seriously wrong with the Alice unit, and Respironics should be contacted. Impedance (Z), measured in k, is defined as the opposition to the flow of alternating current (AC); impedance is - crudely put – a measure of how well electrodes have been applied. Impedance checks are performed at the beginning and the end of each study and as needed (i.e., when signal quality is noted to deteriorate). Acceptable impedance is less than 5k. Temporarily turning off the 60Hz filter is another good indicator of signal quality - noticeable 60Hz artifact with the filter off is indicative of an electrode (or connection) problem. Machine calibrations and impedance checks are described in the document Machine Calibrations, also called the ‘Starting/Stopping Sleep Study Protocol.’ Full details on calibration can be found in the Alice manual. Physiological Calibrations Physiological calibrations are performed at the beginning of each study to demonstrate the proper functioning of monitoring devices. The technician uses this procedure to ensure signal quality in every channel of data. The exact protocol to be followed is outlined in Pre-Study Physiological Calibrations. Please refer to that document while reading the discussion below: “Without moving your head, OPEN your eyes and look straight ahead.” – Allow this to run for 30 seconds or one full epoch/screen. Relatively low voltage, mixed frequency EEG should be apparent, with occasional eye blinks and a relatively high amplitude chin EMG. Be looking for EKG artifact in the EEG and EOG channels. Page 4 TITLE: Calibration of Equipment for Polysomnogram BACK TO TABLE OF CONTENTS 74 “Without moving your head, CLOSE your eyes and keep them closed.” – Again, allow this to run for 30 seconds or one full epoch/screen. Eye blinks should desist and alpha waves, characteristic of relaxed wakefulness, should be apparent, especially in the occipital channels. Eye movements: The EOG measures the movement not of eye muscles but of the cornea-retinal potential, or dipole, relative to a (stationary) reference electrode. In the human eye, the cornea has a slight positive charge and the retina a slight negative charge. Looking to the right should cause a negative deflection of the ROC channel (as the positive cornea moves away from A1) and a positive deflection of the LOC (as the positive cornea moves toward A2). Looking to the left has the opposite effect, etc . “Grit your TEETH. Relax. [Alternately: “Clench your jaw,” “Make a chewing motion.”]” – This should elicit a marked increase in chin EMG amplitude from an already high amplitude signal (Sens=10+). If it does not, reposition and try again. NB: On most patients, I have found that prepping with alcohol only is ideal for obtaining a decent chin EMG; EMG signals are typically better when impedances – normally such a nuisance in other derivations – are a bit high. “Clear your throat [CLR THRT].” – This is intended to test the snore mic. “Pull the toes of your right foot [RT FT] up. Relax.” – As with the chin EMG, flexing of the foot should cause a burst of high amplitude activity, as the monitored muscle group, the anterior tibialis, aids in the flexing action. Unlike the chin EMG, the resting leg EMG should be a relatively flat line. “BREATHE NORMALLY.” – As noted on the Pre-Study Physiological Calibrations Protocol, with the more self-conscious patient, it is often more expedient to give no instruction, and to allow the patient to assume his or her “normal” respiratory rate and rhythm. “Take a deep breath IN. And EXhale.” – Inspiration should result in an upward deflection of FLOW, THO, and ABD channels and an increase in intercostal EMG. “Take a deep breath and HOLD it. [Approximately 10-12 seconds] Breathe.” – While breath is being held ECG artifact should be apparent in one or both respiratory effort channels (THO, ABD). Page 5 TITLE: Calibration of Equipment for Polysomnogram BACK TO TABLE OF CONTENTS 75 1.02 Calibration of DC Signal Protocol (e.g., with Alice5 software) Statement of Purpose Oximeters and CPAP/BiPAP® devices are calibrated weekly; this document outlines steps to be taken in this calibration process. Turn on the oximeter and the CPAP/bi-level unit; one partner should sit quietly on the bed wearing the SaO2 finger probe and keeping the CPAP/bi-level mask occluded. Confirm accurate delivery of pressure simultaneously by measuring pressure at hose with water column or digital manometer. In Alice, select ‘Acquisition & analysis.’ At Configurations screen, select the appropriate ‘Split Night’ configuration. Note which slots CPAP and SaO2 are assigned to by checking ‘Contents.’ Begin an acquisition. Press Enter to move through the Patient Data screen - a Date of birth must be entered to continue! – then press F10. By using the intercom to speak with your partner and by checking the digital display on the appropriate remote control, compare the signals on the screen to the DC signals (what the oximeter and the CPAP/bi-level device are reading). If the signals are not the same, note the difference. Use CTRL/End to abort the acquisition, press F6 to clear the acquisition error, then exit Alice. Open Calib400 by clicking on the appropriate icon on the Windows95 desktop. Press “Y” to test the RJ-11 inputs, then tab to the appropriate slot number. Using the ‘+’ key if Alice was too low and the ‘-‘ key if Alice was too high, adjust the values. Generally, two “clicks” in an SAO2 slot correspond to 1% SaO2. In the example above, tapping the ‘+’ key 4x should correct the problem. A single “click” in a CPAP slot will typically equate to a 0.2cm change. Follow the instructions on-screen to save the new settings and exit; repeat steps 2-6, above, until the readings are identical. For each auxiliary device calibrated, record the date of calibration and your initials in the Cal(ibration) Log. (An example of an Oximeter Calibration Log can be found in Appendix A.) For further details, please see Alice manual . BACK TO TABLE OF CONTENTS 76 Policy and Procedure TITLE: Documentation During Polysomnogram ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 Documentation during the acquisition of a polysomnographic evaluation is integral in the scoring and interpretation of the collected data. The observations of the technologists detail relevant information in addition to the physiological channels being recorded. POLICY: 1.0 General Considerations 1.1 Visual and auditory monitoring. 1.1.1. Audio-visual monitoring system. 1.2 2.0 1.1.1.1 Allows patient to communicate with technologist. 1.1.1.2 Allows technologist to observe and document patient behaviors, arousals, movements, etc. 1.1.1.3 Aids technologist in correlating polysomnographic events with patient activity. 1.1.1.4 Keeps unnecessary interruptions to a minimum. Documentation facilities scoring technologist and interpreting physician in correlating polysomnographic findings with behavioral events. QUESTIONNAIRES AND FORMS 2.1 Pre-sleep questionnaire (See page 151). 2.2 Post-sleep questionnaire (See page 153). 2.3 Bed Partner questionnaire ( See page 163). BACK TO TABLE OF CONTENTS 77 PAGE 2 TITLE: Documentation During Polysomnogram 2.4 PSG technical form (See page 155). 2.5 Titration log form (See page 167). PROCEDURE: 1.0 2.0 ADMINISTERING of QUESTIONNAIRES 1.1 Patient completes pre-sleep questionnaire upon arrival in the sleep disorders center. 1.2 Patient completes post-sleep questionnaire after final awakening. FORMS 2.1 Patient summary form. 2.1.1 Fill in all required information 2.1.2 Detail unusual and pertinent observations and events. 2.1.2.1 2.2 Technical form. 2.2.1 2.3 This information may also be able to be entered electronically into the digital recording at the time of the observation or event. Enter data at 15 to 30 minute intervals. Titration log form. 2.3.1 Enter each pressure change indicating the reason for change. 2.4 Forms should be completed during the study with overall summary written after polysomnographic acquisition is completed. Policy and Procedure TITLE: Pediatric Polysomnography 13 years old and under ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 78 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: REVISION DATE(s): 01/11/2010 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: Provide adequate information to perform quality polysomnograms on pediatric patients per physician order with confidence and competence. This policy includes testing for children and adolescents. Polysomnography is essential to diagnose certain sleep-related conditions. Below is a list of common indications: 1.0 General Considerations 1.1 Disorders included for evaluation. 1.1.1 Snoring. 1.1.2 Excessive Daytime Somnolence. 1.1.3 Insomnia, unexplained, resistant to therapy. 1.1.4 Neuromuscular Disease. 1.1.5 Parasomnias. 1.1.6 Arousal Disorders, which include, but are not limited to: Confessional arousals, sleepwalking, sleep terrors. Other parasomnias include hypnogogic hallucinations and sleep paralysis, nocturnal seizures, bruxism, and rhythmic-movement disorder. 1.1.7 Sleep associated seizures. POLICY: 1.0 Evaluation of ages studied in sleep disorders center. 1.1 7 Years of age and above. PAGE 2 TITLE: Pediatric Polysomnography 13 Years old and under BACK TO TABLE OF CONTENTS 79 2.0 Equipment and staffing needs. 2.1 2.2 Appropriate age-specified equipment and pediatric trained Technician will be scheduled to perform a polysomnographic evaluation for pediatric patient. CO2 Capnography will monitor the pediatric CO2 levels during the polysomngraph test 3.0 Parents must stay with their child during the sleep study. 4.0 4.1 Visit to the sleep disorders center prior to scheduled procedure is encouraged. Familiarize parent and child with the surroundings and answer any questions. PROCEDURES: 1.0 Evaluation procedure. Discuss with the medical director at the time of child arrival for specific instructions on individual cases. 1.1 Follow policy and procedures for: 1.1.1 Polysomnographic montages. 1.1.1.1 1.1.2 Patient arrival, preparation and electrode/sensor application. 1.1.2.1 1.1.3 Check with medical director to determine if a specific montage needs to be utilized. Calibration of equipment for polysomnogram. Physiological calibrations procedures. Refer to policy on page 59. 1.1.3.1 1.1.3.2 1.1.4 Use age specific terminology. Parents can help the child with understanding instructions. Documentation during polysomnogram. PAGE 3 TITLE: Pediatric Polysomnography 13 Years old and under BACK TO TABLE OF CONTENTS 80 2.0 Scoring . 2.1 2.2 Follow policy for scoring. 2.1.1 Sleep stages. 2.1.2 Sleep related events. Check with medical director for any special instructions. American Thoracic Society, Standards and Indications for Cardiopulmonary Sleep Studies in Children, AMJ Respir Crit Care Med, 1996; 153: 866-878. American Academy of Pediatrics, Clinical Practice Guidelines: Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome: Pediatrics, Volume 109, Number 5, April 2002, pp. 707-712. American Academy of Sleep Medicine. Reference Manual for Policies, Procedures, Documentation and Reporting. Rochester, MN: American Academy of Sleep Medicine, 2002. ORIGINAL DATE: 09-01-2006 Policy and Procedure TITLE: Et C02 EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 81 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: REVISION DATE(s): 01/11/2010 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: DEFINITION: EtCO2 assesses ventilation, by measuring carbon dioxide in the exhaled gas. TcCO2 assesses ventilation by measuring carbon dioxide through the skin. SETTING: This guideline is confined to the use of capnography in the sleep laboratory setting as a method of assessing airflow during polysomnographic evaluation. The polysomnographic evaluation must be performed in a facility-based sleep study laboratory, and not in the home or in a mobile facility. INDICATIONS: Capnography is useful in the assessment of apnea, hypoventilation, hypopnea and rebreathing of CO2. Primary indications are: 1.) Pediatric Polysomnography, 2.) Patients with ahistory of lung disease, 3.) COPD patients with history of CO2 retention who require oxygen titration and/or non-invasive ventilation support, 4.) Patient’s with neuromuscular disorders affecting the respiratory muscles and 5.) Patients with tracheostomy. CONTRAINDICATIONS: None. PRECAUTIONS: There is a potential for localized erythema or skin burns from the TcCO2 electrode at high heater temperatures. OUTCOME ASSESSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response. The following competency evaluation tool allows for an objective assessment of the performance of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. INSTRUCTIONS: The validator evaluates the employee in the performance of the competency, indicating either a pass (P) or needs improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for Page 2 TITLE: Et C02 BACK TO TABLE OF CONTENTS 82 procedure, preparing environment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY DEMONSTRATES KNOWLEDGE OF/SKILLS IN P OR NI COMMENTS Equipment Specific Operation / Calibration • Assure proper function of EtCO2/TcCO2 device. • Knowledge of operation of EtCO2/TcCO2 device. • Calibrate EtCO2/TcCO2 device to PSG system and gas calibration as required. Nasal Cannula • Knowledge of how to fit appropriate nasal cannula for monitoring EtCO2/TcCO2 allowing for patient comfort and compliance. • Adjust and proper fit. TcCO2 Electrode • Knowledge of appropriate sites for application of Application TcCO2 electrode. • Proper application and fixation of electrode. Patient Interaction • Explain EtCO2/TcCO2 procedure to patient during Pre-testing procedure. • Communication skills. Use of Equipment • Identify when to use EtCO2/TcCO2 monitoring during NPSG. • Understands the basic theory of EtCO2/TcCO2 Monitoring • State normal values for EtCO2/TcCO2 and factors that can affect observed values. • Clinical reasoning • Identify event characteristics (i.e., respiratory, cardiac, sleep stage, etc). Documentation • Document and record changes in noted during NPSG on polygraph and technical note forms. • Identify, document and inform supervisor of equipment problems and EtCO2/TcCO2 monitoring supply needs. Patient Safety • Identify when to contact Medical Director. • Identify when to change the TcCO2 site if using higher electrode temperatures. • Basic trouble shooting of device and possible solutions. Infection Control • Proper disposal of interface device. • Proper cleaning and disinfection of nondisposable items Policy and Procedure TITLE: C02 Capnograph ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 83 REVIEW DATE(s):03-01-2007 3-08-2011 APPROVAL(s): SIGNATURE: REVISION DATE(s): 01/11/2010 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: A quantifiable method for measurement of end tidal CO2 (EtCO2), or Transcutaneous CO2 (TCCO2) during overnight Polysomnogram. DEFINITON: EtCO2 assesses ventilation, by measuring carbon di9oxide in the exhaled gas. TcCO2 assesses ventilation by measuring carbon dioxide through the skin. SETTING: This guideline is confined to the use of capongraphy in the sleep laboratory setting as a method of assessing airflow during Polysomnographic evaluation. The Polysomnographic evaluation must be performed in a facility-based sleep study laboratory, and not in the home or in a mobile facility. INDICATION: Capnography is useful in the assessment of Apnea, Hypoventilation, Hypopnea and rebreathing of CO2. Primary indications are: 1.) Pediatric Polysomnography, 2) Patient with a history of lung disease, 3) Require oxygen titration and/or non-invasive ventilation support, 4) Patient’s with neuromuscular disorders affecting the respiratory muscles 5) Patient with Tracheostomy. CONTRAINDICATIONS: None. PRECAUTIONS: There is a potential for localized erythema or skin burns from TcCO2 electrode at high heater temperatures. OUTCOME ASSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response. The following competency evaluation tool allows for an objective assessment of the performance of the Polysomnographic technologist, Polysomnographic technician and Polysomnographic trainee. INSTRUCTIONS: The validate evaluates the employee in the performance of the competency, indicating either a pass (P) or needs improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified on the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for Page 2 TITLE: C02 Capnograph BACK TO TABLE OF CONTENTS 84 procedure, preparing encironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY DEMONSTRATES KNOWLEDGE OF/SKILLS IN P OR NI P OR NI COMMENTS Equipment Specific of Operation/ Calibration Assure proper function of EtCO2/TcCO2 device. Knowledge of operation of EtCO2/TcCO2 device. Calibrate EtCO2/TcCO2 device to PSG system and gas calibration as required. CALIBRATION AS REQUIRED: Nasal Cannula Knowledge of how to fit appropriate nasal. Cannula for monitoring EtCO2/TcCO2 allowing for patient comfort and compliance. Adjust and proper fit. Application TcCO2 electrode. Proper application and fixation of electrode. Patient interaction interation explain EtCO2/TcCO2 procedure to patient during pre-testing procedure. Policy and Procedure TITLE: Pediatric Polysomnography 14 years old to 18 years old ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 85 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: REVISION DATE(s): 01/11/2010 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: Provide adequate information to perform quality polysomnograms on pediatric patients per physician order with confidence and competence. This policy includes testing for children and adolescents. Polysomnography is essential to diagnose certain sleep-related conditions. Below is a list of common indications: 1.0 General Considerations 1.1 Disorders included for evaluation. 1.1.1 Snoring. 1.1.2 Excessive Daytime Somnolence. 1.1.3 Insomnia, unexplained, resistant to therapy. 1.1.4 Neuromuscular Disease. 1.1.5 Parasomnias. 1.1.6 Arousal Disorders, which include, but are not limited to: Confessional arousals, sleepwalking, sleep terrors. Other parasomnias include hypnogogic hallucinations and sleep paralysis, nocturnal seizures, bruxism, and rhythmic-movement disorder. 1.1.7 Sleep associated seizures. POLICY: 1.0 Evaluation of ages studied in sleep disorders center. 1.1 7 Years of age and above. PAGE 2 TITLE: Pediatric Polysomnography BACK TO TABLE OF CONTENTS 86 2.0 Equipment and staffing needs. 2.1 Appropriate age-specified equipment and pediatric trained Technician will be scheduled to perform a polysomnographic evaluation for pediatric patient. 3.0 Parents may stay with their child during the sleep study. 4.0 Visit to the sleep disorders center prior to scheduled procedure is encouraged. 4.1 Familiarize parent and child with the surroundings and answer any questions. PROCEDURES: 1.0 Evaluation procedure. Discuss with the medical director at the time of child arrival for specific instructions on individual cases. 1.1 Follow policy and procedures for: 1.1.1 Polysomnographic montages. 1.1.1.1 1.1.2 Patient arrival, preparation and electrode/sensor application. 1.1.2.1 1.1.3 Check with medical director to determine if a specific montage needs to be utilized. Calibration of equipment for polysomnogram. Physiological calibrations procedures. Refer to policy on page 59. 1.1.3.1 1.1.3.2 1.1.4 Use age specific terminology. Parents can help the child with understanding instructions. Documentation during polysomnogram. PAGE 3 TITLE: Pediatric Polysomnography BACK TO TABLE OF CONTENTS 87 2.0 Scoring . 2.1 2.2 Follow policy for scoring, refer to pages 77-86. 2.1.1 Sleep stages. 2.1.2 Sleep related events. Check with medical director for any special instructions. Policy and Procedure TITLE: TECHNICIAN RECORD REVIEW ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 88 REVIEW DATE(s 03-01-2007, 3-08-2011 APPROVAL(s): SIGNATURE: REVISION DATE(s): 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: Purpose: The purpose of this policy is to establish universal guidelines for the technical analysis of raw patient data and the generation of technical reports and physician interpretations. Policy: Sleep studies will be reviewed and analyzed in a uniform, standard manner regardless of who is doing the review. This should eliminate any confusion and instill consistency among scorers. Likewise, reports and interpretations shall be prepared in a systematic fashion. Responsibility: The technician scoring the polysomnogram is responsible for adhering to the uniform standards of practice defined by this policy. Procedural Index: Scoring Protocols Generating Summary Reports Physician Interpretation Procedures Procedure: Scoring Protocols Sleep studies will be reviewed and scored by technicians or designated representatives. The technical review of the record is inclusive of the following: Sleep stage ECG dysrhythmias ECG rhythm Arousals Respiratory disturbances Leg movements Abnormal behavioral manifestations Page 2 TITLE: TECHNICIAN RECORD REVIEW BACK TO TABLE OF CONTENTS 89 Sleep architecture is generally the first parameter scored by the technician. Sleep is scored as stage Wake, N1, N2, N3 REM, or, according to the conventions AASM scoring rules manual. Sleep is staged from the first “lights off” to “lights on”. Spontaneous arousals are those arousals from sleep, which are not secondary to any identifiable pathological cause. Arousals are typically scored after sleep has been staged. A separate pass is usually needed for the arousals. An arousal must meet the criteria defined by the AASM task force and are as follows: An EEG arousal is an abrupt shift in EEG frequency, which may include theta, alpha, and/or frequencies greater than 16Hz but not spindles, subject to the following rules and conditions. 1. Subjects must be asleep, defined as (10) continuous seconds or more of the indications of any stage of sleep, before an arousal can be scored. 2. A minimum of (10) consecutive seconds of intervening sleep is necessary to score a second arousal. 3. The EEG frequency shift must be (3) seconds or greater in duration to be scored as an arousal. 4. Arousals in NREM sleep may occur without concurrent increases in submental (chin) EMG amplitude. 5. Arousals are scored in REM sleep only when EEG frequency shifts are accompanied by concurrent increases in submental (chin) EMG. 6. Arousals cannot be scored based on changes in submental (chin) EMG amplitude alone. 7. Artifacts, K-complexes or Delta waves are not scored as arousals unless accompanied by an EEG frequency shift in a least one derivation. If such activity precedes an EEG frequency shift, it in not included in reaching the (3) second duration criteria. When occurring within the EEG frequency shift, artifacts or Delta wave activity are included in meeting duration criteria. 8. The occurrence of pen-blocking artifact should be considered an arousal only if an EEG arousal pattern is contiguous. The amplifier-blocking event can be included in reaching duration criteria. 9. Nonconcurrent, but contiguous EEG and EMG changes which were individually less than (3) seconds, but together greater than (3) seconds in duration, are not scored as arousals. 10. Intrusion of alpha activity of less than (3) seconds duration into NREM sleep at a rate greater than one burst per (10) seconds is not scored as an EEG arousal. Three seconds of alpha sleep is not scored as an arousal unless a 10-second episode of alpha-free sleep precedes it. 11. Transitions from one stage of sleep to another are not sufficient of themselves to be scored as EEG arousals unless they meet the criteria indicated above. Respiratory events are scored following the sleep staging and arousals. Respiratory events are assigned to the following categories: obstructive apneas, obstructive hypopneas, central apneas, and mixed apneas. Obstructive apnea is defined as the absence of airflow despite the persistence of respiratory effort for a Page 3 TITLE: TECHNICIAN RECORD REVIEW BACK TO TABLE OF CONTENTS 90 Duration of at least (10) seconds. Obstructive hypopnea is defined as at least a 30% reduction in airflow with concurrent respiratory effort for a duration of at least (10) seconds. To be scored as a hypopnea, the event must be terminated with an arousal or associated with an oxygen desaturation of at least 3%. Medicare guidelines do not recognize the termination arousal, so the hypopnea must be followed by a desaturation of at least 4% to qualify as a hypopnea when testing a Medicare patient. Central apnea is defined as a cessation of airflow as well as thoracic and abdominal effort for a duration of at least (10) seconds. Sleep onset central apneas are considered insignificant and are not to be scored unless they are repetitive and arousing. Mixed apnea is defined as an apnea of at least (10) second duration, which begins with a central component usually, followed by an obstructive component. The duration of apneic and hypopneic events is delineated using the reader station’s mouse. Leg movements are scored with respiratory events or by themselves. Only periodic limb movements are scored. To qualify as a periodic limb movement there must be a series of movements including at least (4) movements, each separated by 5-90 seconds. These movements must be at least .5 seconds in duration, with amplitude of at least 25% of the leg movement bio-calibrations performed at start of test. Limb movements within or following arousals, or respiratory events are not scored. Finally, periodic limb movements are only scored in epochs scored as NREM sleep usually. The vast majority of limb movements in REM sleep is phasic jerks and is not considered to same as PLMs. ECG is reviewed for several items: 1. Type of rhythm (e.g., normal sinus, atrial fibrillation). 2. Presence of arrhythmia (PVCs, PACs, etc.) Abnormal behavioral manifestations should be described by the technician in detail in the technician’s notes. Correlate the technician’s description with any atypical or unusual Polysomnographic patterns. The scoring technician must verify all automatic digital scoring. Generating Summary Reports When the technician has completed his/her review and scoring of the polysomnogram he/she must generate a summary report for the Medical Director’s use and to place in the patient’s file. A custom report outline for each test has been created in the system and it contains all the basic information generally needed. The steps involved in generating the summary report are listed in the user manual provided by the software maker which is available to technicians. ORIGINAL DATE: 09-01-2006 Policy and Procedure TITLE: Scoring Guidelines EFFECTIVE DATE: 09-01-2006 BACK TO TABLE OF CONTENTS 91 REVIEW DATE(s 03-01-2007, 3-08-2011 APPROVAL(s): SIGNATURE: REVISION DATE(s): 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: OBJECTIVES: � To describe the knowledge and skills required to accurately score sleep stages and clinical events recorded during the polysomnographic evaluation. � To define quality assessment methods for scoring sleep studies. � To describe the knowledge and skills necessary to generate a comprehensive and accurate report. DEFINITION: Scoring is the process of reviewing, analyzing, classifying and tabulating sleep staging and clinical events from the polysomnogram according to published professional standards and guidelines. Recordings are staged in 30 second epochs. Clinical events include, but are not limited to, sleep related movements; arousals; cardiac arrhythmias; sleep disordered breathing; and oxygen destructions. SCOPE: This guideline applies to sleep state recognition, clinical event scoring and report generation for comprehensive polysomnography; and respiratory event scoring for portable monitoring if used by the center. Scoring will be performed according to guidelines outlined in The American Academy of Sleep Medicine (AASM) Manual for the Scoring of Sleep and Associated Events. Pediatric and adult scoring rules will be applied to the appropriate age groups as indicated in the manual. INDICATIONS: The report compiled from the accurate scoring of the raw data is the single most important element of the nocturnal polysomnographic examination and the preparation should be thorough and systematic. Scoring according to professionally accepted guidelines is necessary because much of its diagnostic utility depends on the ability to correlate specific changes or abnormalities. The generation of an accurate report is a significantly more powerful and complex tool than could be provided by individual and independent measurements of each variable. The methods and requirements for scoring each of the variables and their integration through the technical report are determined by the medical director. The interpreting physician uses the technical report to complete the clinical impression and diagnostic recommendation. CONTRAINDICATIONS: No contraindications in the sleep disorders center are present. PAGE: 2 TITLE: Scoring Guidelines BACK TO TABLE OF CONTENTS 92 OUTCOME ASSESSMENT: Scoring quality is determined by inter-scorer reliability assessment. The following competency evaluation tool allows for an objective assessment of the scoring performance level of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. Updated September 2009 PROCEDURE: Inter-scorer reliability assessment will be performed on three 200 epoch samples per quarter, or 12 per year. The following parameters will be compared for agreement with the medical director or corporate appointed board certified sleep specialist: epoch-by-epoch sleep staging, respiratory events, leg movements and arousals. Each scorer is evaluated for agreement with the reference scorer on each parameter, indicating either a pass (P) if agreement is at minimum 90%, or needs improvement (NI) if agreement is < 90%.. For each NI, an action plan for correction is specified in the quality assessment report. Corrective actions for scorers that need improvement may include repeat testing, training, or exclusion from further scoring. Scorers will also need to demonstrate competencies outlined below for identifying all types of normal and abnormal clinical events and artifact, as well as optimizing the viewing of the recording and compiling a complete and accurate report. Updated September 2009 CORE COMPETENCY DEMONSTRATES KNOWLEDGE OF/SKILLS IN P OR NI COMMENTS General Scoring Skills • Identifying characteristic waveforms of sleep and wakefulness. • Applying rules according to patient age. • Identifying artifact. • Differentiating between normal and abnormal clinical events. • Utilizing scoring software to mark and label sleep stages and event types. • Validating the integrity of the record by checking calibrations and impedences. • Utilizing system software to optimize the recording display using: • derivation changes • sensitivity or gain adjustments • filter settings • time scale changes Page 3 TITLE: Scoring Guidelines BACK TO TABLE OF CONTENTS 93 • channel inversion • 50/60 Hz filter control • Identifying seizure activity. • Identifying parasomnia activity. • Identifying oxygen desaturation events. • Identifying CO2 levels. • Identifying PH levels Visual Rules • Applying AASM guidelines for scoring sleep stages in children and adults: • W, N1, N2, N3, REM • Applying the rules for Major Body Movements • Recognizing the need for a manual review of all computerized scoring. Arousal Rules • Identifying and scoring arousals according to accepted guidelines. Cardiac Rules • Applying AASM guidelines for identifying and reporting on types and rates of arrhythmias in adults and children. • sinus tachycardia • sinus bradycardia • asystole > 3 seconds • wide complex tachycardia • narrow complex tachycardia • atrial fibrillation • other arrhythmias Movement Rules • Identifying sleep related movements according to AASM guidelines: • Periodic Limb Movements in Sleep (PLMS) • Alternating Leg Muscle Activation (ALMA) • Hypnogogic foot tremor (HFT) • Excessive Fragmentary Myoclonus (EFM) • Bruxism • REM Sleep Behavior Disorder (RBD) • Rhythmic Movement Disorder Updated September 2009 Respiratory Rules • Identifying sleep disordered breathing in adults and children according to AASM guidelines: Page 4 TITLE: Scoring Guidelines BACK TO TABLE OF CONTENTS 94 Apneas is scored by using the Thermister. Hypopneas is scored by the Pflow. • Cheyne-Stokes respiration • Obstructive apnea • Central apnea • Mixed apnea • Obstructive hypopnea • Respiratory Effort Related Arousal (RERA) • Hypoventilation . Report Generation • Using analysis software for report generation. • Manually calculating data in report. • Insuring correct and complete patient information on report. • Providing printed samples of sleep stage and/or clinical events per facility protocol. • Reviewing final report for errors. Inter-scorer Reliability • Maintaining epoch by epoch correlation of at minimum 90% with the reference scorer on: • Sleep stages • Arousals • Respiratory events • PLMs BACK TO TABLE OF CONTENTS 95 Policy and Procedure TITLE: ELECTRICAL SAFETY ORIGINAL DATE: 09-01-2006 REVIEW DATE(s 03-01-2007, 3-08-2011 APPROVAL(s): SIGNATURE: EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: POLICY: The following safety precautions shall be followed at all times when electrical devices are utilized. PROCEDURE: Electrical devices shall be protected from wet floors. The frame of all electrically operated machinery shall be grounded. Brass light sockets within reach shall be replaced with nonconducting material. Extension lights shall be equipped with rubber handles, sockets and lamp guards. The cords shall be of approved rubber covered type. Nonconducting links shall be inserted in brass pull chains. If a "shock is felt" from any electrical equipment, immediately remove from service, tag equipment and report it to the Engineering Department for repair. Care is to be maintained when connecting and disconnecting electrical equipment. Switch to "off" position before connecting or disconnecting. Turn on the polysomnograph and calibrate before the patient is connected to the instrument. Disconnect the patient from the polysomnograph and then turn the instrument off. BACK TO TABLE OF CONTENTS 96 Page 2 TITLE: ELECTRICAL SAFETY Do not disconnect the plug from the wall by grasping the power cord. Grasp the plug itself and disconnect. Do not roll equipment or furniture over patient and power cables. Report and remove from service any device that has been dropped, abused, had liquid spilled on it or has evidence of overheating. A routine visual inspection are made by the Tech, and a yearly inspection made by the biomedical Engineer. BACK TO TABLE OF CONTENTS 97 Policy and Procedure TITLE: ELECTRICAL ORIGINAL DATE: 09-01-2006 REVIEW DATE(s 03-01-2007, 3-08-2011 APPROVAL(s): SIGNATURE: EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: POLICY: All appropriate personnel will be responsible for assessing the condition of electrical equipment in their use. PROCEDURE: Electrical equipment and devices with electronic components shall be evaluated as follows: Electrical connectors, such as jacks, receptacles or plugs, must be of an approved type, free of cracks or breaks and properly attached to the line cord or cable. Mechanical indexing mechanisms must be free of wear or damage to prevent improper alignment or mating of plugs and receptacles. Cables, cords and internal wiring must be of an approved type and of proper wire size to safely handle the required current. All cables, cords and internal wiring must be of sufficient length. All cables, cords and internal wiring must be free of unsafe or unsightly splices, and of frayed, cracked, abraded or brittle insulation. Cables, clips, studs and terminals must be free of dirt, rust, corrosion and other deposits. Switches, circuit breakers, relay points and selectors must not be dirty, corroded, excessively worn or pitted. BACK TO TABLE OF CONTENTS 98 Page 2 TITLE: ELECTRICAL Grounding systems must be of an approved type and properly installed. All electrical components, such as relays, transformers, capacitors, electron tubes and resistors, must operate without overheating. Heating elements must produce and maintain the temperature rise required for proper operation. Electrical meters must respond to the appropriate control and operate properly. Electrical components, such as connectors or switches on explosion-proof equipment, must conform to the requirements of the National Fire Protection Association Handbook. . Batteries must be properly charged and free of cracks, breaks or leaks. Electrolyte or wet cell batteries must be at the proper level. Electrical leakage currents must be within acceptable limits. Electric Motors: The electric motor must operate under load without excessive variation/hunting (varying speed) or noise. The electric motor must operate without excessive temperature rise when operated at the rated duty cycle and mechanical load. BACK TO TABLE OF CONTENTS 99 Policy and Procedure TITLE: TECHNICAL FAILURES DUE TO EQUIPMENT MALFUNCTION ORIGINAL DATE: 09-01-2006 REVIEW DATE(s 03-01-2007, 3-08-2011 APPROVAL(s): SIGNATURE: EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 3-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: POLICY FOR TECHNICAL FAILURES DUE TO EQUIPMENT MALFUNCTION PROCEDURE 1. ANY STUDY THAT IS LESS THAN 2 HRS OF RECORDING IS CONCIDERED AN INCOMPLETE STUDY. 2. CALL PATIENT TO INFORM OF EQUIPMENT FAILURE AND SCHEDULE A REPEAT STUDY 3. CALL THE ELECTRIC INSPECTOR TOM BLEDSOE AT 502-381-5444 TO GET EQUIPMENT EVALUATED AND TESTED IF ITS EQUIPMENT FAILURE RELATED. 4. IF EQUIPMENT IS NEEDED TO BE REPAIRED CALL RESPIRONICS AT 1-800-345-6443 PRODUCT SUPPORT 20258348 TO OBTAIN AN REFFERENCE AUTHORIZATION NUMBER. 5. LOG THE ITEM, SERIAL NUMBER, RA NUMBER AND DATE OF ITEM THAT IS BEING SENT BACK ON THE LOG SHEET UNDER RETURNS. 6. IF THE EQUIPMENT IS UNABLE TO BE REPAIRED IT IS TO BE REPLACED. BACK TO TABLE OF CONTENTS 100 Policy and Procedure TITLE: SCORING SLEEP RELATED EVENTS ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 To assist the attending technologist in scoring sleep-related events, including respiratory events, arousals, leg movements, heart rate and arrythmias. POLICY: 1.0 General Considerations 1.1 Standard definitions will be used for all sleep-related events. 1.2 2.0 Sleep-related definitions will conform to the Clinical Practice Parameters set by the American Academy of Sleep Medicine (AASM) where they exist. Scoring EEG Arousals 2.1 Patient must be a sleep 10 seconds or more to score an arousal 2.2 Minimum of 10 continuous seconds of intervening sleep is needed to score a second arousal. 2.3 EEG frequency shift must be 3 seconds or more to be scored as an arousal. 2.4 Arousals in NREM sleep may occur without an increase in the submental EMG amplitude. 2.5 Arousals in REM sleep are scored only if there is an increase in submental EMG amplitude. BACK TO TABLE OF CONTENTS 101 PAGE 2 TITLE: Scoring Sleep Related Events 2.6 Arousals cannot be based on submental EMG amplitude only. 2.7 They are accompanied by an EEG frequency shift lasting 3 seconds or greater. 2.8 Three seconds of alpha intruded sleep is scored as an arousal only if 10 seconds of alpha free sleep precedes it. 2.9 Arousals that occur without any explanation are scored as spontaneous. 2.10 3.0 4.0 Snore arousals are defined as an event of progressive snoring or snorting terminated by a cortical arousal. No desaturation or obvious hypopnea is seen with this event, however, an EEG arousal as defined is present. Scoring Periodic Limb Movements 3.1 Leg movement (LM) is a 0.5 to 5 second burst of anterior tibialis activity with an amplitude of 25% or greater of the calibration movements. 3.2 Periodic Limb Movement (PLM) episode is 4 or more LMs separated by more than 5 seconds but less than 90 seconds from the onset of each LM. 3.3 To score LMs individually or during PLM episode as associated with an arousal, the arousal onset must follow the LM onset by not more than 3 seconds. 3.4 Left and right LMs can be analyzed separately. Scoring Sleep Related Respiratory Events 4.1 Apnea is defined as a complete cessation of airflow for at least 10 seconds. 4.1.1 4.1.2 4.1.3 Central apnea is defined as a cessation of airflow for at least 10 seconds with an absence of thoracic and abdominal effort. Obstructive apnea is defined as a cessation of airflow for at least 10 seconds with continued thoracic and abdominal effort. Mixed apnea is defined as a cessation of airflow for at least 10 seconds with an absence of thoracic and abdominal effort followed by continued thoracic and abdominal effort. BACK TO TABLE OF CONTENTS 102 PAGE 3 TITLE: SCORING SLEEP RELATED EVENTS 4.2 5.0 Hypopnea is defined as an abnormal respiratory event of at least 10 seconds with at least 30% decrease in thoracic and abdominal effort or airflow as compared to baseline accompanied by at least a 4% oxygen desaturation. Calculating Indices. 5.1 5.2 Apnea/hypopnea Index (AHI). 5.1.1 AHI equals the total number of apneas and hypopneas divided by total sleep time (TST) in hours. 5.1.2 Apnea index equals the total number of apneas divided by TST in hours. 5.1.3 Hypopnea index equals the total number of hypopneas divided by TST in hours. Periodic Limb Movement (PLM) Index. 5.2.1 PLM index equals the total number of periodic limb movements divided by TST in hours. 5.2.2 PLM arousal index equals the total number of periodic limb movements associated with an arousal divided by the TST in hours. BACK TO TABLE OF CONTENTS 103 Policy and Procedure TITLE: Scoring EEG during Sleep ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 PURPOSE: To establish and formalize the scoring system of sleep stage. POLICY: All sleep records will be scored using established criteria. For infants to the age of 6 months, sleep staging will be scored according to the criteria established in A Manual of Standardized Terminology, Technology and Criteria for Scoring States of Sleep and Wakefulness in Newborn Infants (1). All sleep recordings on patients over 6 months of age will be scored for sleep stage using the criteria established A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human PROCEDURE: 1.0 Monitoring Sleep for Staging 1.1 Electroencephalogram (EEG) electrode placement for monitoring and scoring sleep stages. 1.1.1 The EEG is the core measurement of polysomnography. Reliable recording of EEG begins with accurate measurement of the skull according to the International 10-20 System of Electrode Placement (3). 1.1.2 Sleep stages are best visualized at C3 and C4 using referential derivations of C3/M2 and/or C4/M1. In addition, a bipolar derivation of C3/A2 and/or C4M1 is recommended. 1.1.2.1 1.1.2.2 1.1.3 A1 is placed on the left mastoid. A2 is placed on the right mastoid. For assessing sleep onset or arousals during sleep, the derivation of O1/A2 or O2/A1 should be used in addition to C3/A2 and C4/A1. BACK TO TABLE OF CONTENTS 104 PAGE 2 TITLE: Scoring EEG during Sleep 1.1.4 1.2 Additional 10/20 system electrode placements and derivations are required for recording for recording EEG activity during sleep for documenting and localizing epileptiform activity. Electro-occulogram (EOG) electrode placement for monitoring and recognizing eye movements during sleep. 1.2.1 Electrodes should be placed at the outer canthus of the eye, o ne approximately 0.5 cm above and slightly lateral to the canthus and the other approximately 0.5 cm below and slightly lateral to the canthus. These are referenced to the opposite mastoid in a referential derivation. 1.2.1.1 Right outer canthus (ROC) referenced to M1. 1.2.1.2 1.2.2 1.3 left outer canthus (LOC) referenced to M2. Classification of eye movements may assist differentiation between sleep stages and wakefulness. 1.2.2.1 Blinking eye movements. 1.2.2.2 Slow rolling eye movements. 1.2.2.3 Rapid eye movements. Electromyogram (EMG) electrode placement for monitoring muscle activity during sleep. 1.3.1 2.0 Chin EMG Placement 1.3.1.1 Required for differentiating wakefulness and Rapid Eye Movement (REM) sleep in adults, pediatrics and older infants. May be less useful in newborn infants. Sleep Stages for 6 Months or Older 2.1 Stage W (wakefulness) 2.1.1 Wakefulness is defined by alpha activity (7-14 cps activity), more BACK TO TABLE OF CONTENTS 105 PAGE 3 TITLE: Scoring EEG during Sleep Prominent in the occipital leads, for more than 50% of the epoch. Eye opening results in attenuation of alpha activity. 2.1.2 2.2 2.3 Usually, but not necessarily accompanied by a relative high tonic chin EMG. Eye blinks may be seen without classic conjugate rapid eye movements (REMs). Stage 1 2.2.1 Defined by a relatively low voltage, mixed frequency EEG with a prominence of activity in the theta (2-7 cps) range. Vertex sharp waves may appear with amplitude as high as 200 uV. Absence of K-complexes, sleep spindles and REMs. It is also characterized by slow rolling eye movements and tonic EMG levels are usually below those of relaxed wakefulness. Alpha activity is less than 50% of the epoch. 2.2.2 Transition from wakefulness to other sleep stages or following body movements or arousals during sleep. Stage 2 2.3.1 Defined by the presence of sleep spindles (12-14 cps activity lasting at least 0.5 seconds) and K complexes and the absence of sufficient high amplitude, slow activity noted in Stage 3 and 4. K complexes are defined as EEG wave forms having a well delineated negative sharp wave which is immediately followed by a positive component with a total duration of the K complex should exceed 0.5 spindles and K complexes are transient phenomena. If less than 3 minutes of recording occurs between spindles and/or K complexes, the intervening epochs are scored as Stage 2. If the interval is greater than 3 minutes, the interval is scored as Stage 1, even if it contains no movement arousal. 2.4 Stage 3 2.4.1 Defined by an EEG recording in which at least 20% but not more than 50% of the epoch consists of waves of 2 cps or slower with an amplitude greater than 75 uV from peak to peak (the difference between the most negative and positive points of the wave). BACK TO TABLE OF CONTENTS 106 PAGE 4 TITLE: Scoring EEG during Sleep 2.5 3.0 Stage REM 2.6.1 Defined by the appearance of relatively low voltage, mixed frequency EEG activity accompanied by episodic REMs. The EEG pattern resembles the one described in Stage 1, except that vertex sharp waves are not prominent in Stage REM. “Saw-tooth” waves may be noted with bursts of REM. Aplha activity may be somewhat more prominent during Stage REM than during Stage 1 and the frequency is generally 1-2 cps slower than during wakefulness. There is an absence of K complexes and sleep spindles. 2.6.2 To define the precise beginning and end of REM periods, the EEG, EOG and EMG activity must be used. 2.6.2.1 Sleep spindles and K complexes stop and the EEG changes to relatively low voltage, mixed frequency for one or more epochs before REMs start. Score Stage REM from the last sleep spindle or K complex if the EMG is at the same level before and after the end of the spindle or K-complex and there has been no movement arousal. For more details, refer to pages 9-10 in the manual (2). 2.6.2.2 REM ends with the absence of REMs, augmentation of the EMG, or occurrence of sleep spindles and/or K-complexes. For more details refer to pages 10-11 in the manual (2). Scoring Sleep in Newborn Infants 3.1 Guidelines for categorizing the sleep stages of full term newborns. Due to rapid development changes, adjustments may be required when studying premature infants. BACK TO TABLE OF CONTENTS 107 PAGE 5 TITLE: Scoring EEG during Sleep Center of Kentuckiana 3.2 In addition to the parameters for staging in older infants and adults, behavioral observations provide valuable information for interpretation of sleep stages in infants. 3.3 Defined sleep patterns. 3.3.1 LV1 – “Low voltage irregular” activity similar in all head regions with little variation. Voltage 14-35 uV but generally 20-30 uV. Predominant theta activity (5-8 cps) but also slow waves (1-5 cps). 3.4 3.5 3.3.2 TA- “Trace Alternate” activity similar in all head regions with little variation. Voltage 14-35 uV but generally 20-30 uV. 3.3.3 Predominant theta activity (5-8 cps). Duration of bursts is 3-8 seconds and they are separated by 4-8 seconds of attenuated mixed frequency activity. 3.3.4 HVS – “High voltage slow” activity is a continuous rhythmic activity of medium to high voltage (50-150 uV) with frequency of 0.5-4 cps. 3.3.5 M – “Mixed” pattern of intermingled high voltage slow and low voltage components with little periodicity. Amplitude usually lower than HVS pattern. Wakefulness or “Non-Sleep States” 3.4.1 Best described by behavioral observation as polygraphic criteria are difficulty to assess. 3.4.1.1 Crying – vocalization with motor activity, eyes open or closed with facial grimacing. 3.4.1.2 Active wake – gross body movements, eyes open and moving, may be vocalization. 3.4.1.3 Quiet awake- inactivity, eyes open and “bright” with fixation on objects, face relaxed. Active REM Sleep BACK TO TABLE OF CONTENTS 108 PAGE 6 TITLE: Scoring EEG during Sleep 3.6 3.7 3.5.1 EEG activity defined as variable with LV1, M, or rarely HVS pattern. 3.5.2 EOG activity defined as eyes closed with blinks, REMs, as well as slow rolling eye movements. 3.5.3 EMG activity defined as suppressed when not moving. 3.5.4 Behavior defined as periods of activity (including smiling, grimacing, frowning, sucking, limn and finger movements. Body movements, generally slow but at times sudden and jerky, alternate with periods of quiescence. Penile erections and vocalizations present. Respirations are irregular. Quiet Sleep 3.6.1 EEG activity as HVS, TA or M. 3.6.2 EOG activity is defined by closed eyes with no REMs. 3.6.3 EMG activity if high. 3.6.4 Behavior defined as quiescence, regular respirations, no body movements except mouth movements and occasional startles. Indeterminate Sleep 3.7.1 3.8 Epochs which do not meet the criteria of Active-REM or Quiet Sleep. Most ofet seen when sleep stages are changing and with arousals. Artifact Time 3.8.1 Similar to movement time. If less than one minute of time occurs when it is difficult to determine the state of the infant’s sleep due to movement and vocalization it is scored the same as the preceding period. If more than one minute, it is scored as artifact time. BACK TO TABLE OF CONTENTS 109 Policy and Procedure TITLE: Titration of Positive Airway Pressure During Sleep ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURPOSE: To insure consistency among polysomnographic technologists in the sleep disorders center while performing positive airway pressure (PAP) titration studies. Positive airway pressure is a non-invasive treatment of sleep related breathing events and requires titrating the pressure to eliminate respiratory events, repetitive EEG arousals, oxygen desaturation, and snoring. POLICY: Positive airway pressure titration is to be initiated on order of the sleep disorders center medical director. A written protocol for performing split night studies can be utilized when appropriate. This policy covers both continuous positive airway pressure (CPAP) titration and bi-level positive airway pressure (Bi-Level PAP). PROCEDURE: 1.0 Patient Orientation and Preparation 1.1 1.2 1.3 1.4 Review patient intake sheet and physician’s order for titration. Obtain and document baseline oxygen saturation while the patient is awake and in the following positions- sitting up and supine. Have the patient view a video on PAP titration. 1.3.1 Have TV and DVD equipment set up in patient room prior to patient arrival. 1.3.2 Allow adequate time for viewing and questions. Explain PAP procedure to the patient. 1.4.1 Describe the titration process to allow the patient to know that the pressure will be titrated during the study. BACK TO TABLE OF CONTENTS 110 PAGE 2 TITLE: Titration of Positive Airway Pressure during Sleep 1.4.2 1.5 Instruct the patient on how to contact technologist during PAP titration. Fit the patient with the appropriate PAP interfaces, i.e. mask, nasal pillows, and appropriate headgear etc. 1.5.1 1.5.2 1.5.3 1.6 2.0 Determine if the patient wears dentures. 1.5.1.1 Most masks have to be stabilized on the upper lip by the teeth or dentures. 1.5.1.2 If the patient cannot sleep with dentures in place, an interface such as nasal pillow may be the appropriate option to allow for adequate seal. Ask the patient if there are any initial concerns about using PAP therapy during the study. After the appropriate PAP interface has been selected, allow the patient to hold the mask to his/her face at a low pressure prior to securing with headgear. 1.5.3.1 Allow patient to have control over removing the interface if the pressure becomes overwhelming. 1.5.3.2 Instruct patient on how to remove the mask after it is secured with the headgear and again, explain how to signal for the technologist. Document interface type and size on APT technical summary form as well as any nasal patency issues. Titration of CPAP 2.1 Monitor CPAP flow signal from titration equipment to the acquisition equipment through a DC channel if required. 2.1.1 2.2 Alternatively, place thermistor under mask or in designated nasal pillow shell for flow signal. Initiate CPAP at a level adaptation, usually 4-5 cm H2O. BACK TO TABLE OF CONTENTS 111 PAGE 3 TITLE: Titration of Positive Airway Pressure During Sleep 2.2.1 CPAP may be initiated at a higher level per patient request or physician order. Document reason 2.3 Determine that the patient is in a comfortable position and check for interface leaks. Make necessary adjustments. 2.4 Titrate CPAP pressure to eliminate respiratory events, oxygen desaturation, snoring and EEG arousals. 2.4.1 Increase pressure in 2 cm H2O increments. 2.4.2 If patient is sensitive to pressure increases, increments of 0.5 or 1 cm H20 may be used. 2.4.3 Note titration of CPAP pressure may vary with patient tolerance. 2.4.4 Adequate time should be allowed for patient to acclimate to the pressure at each increment at least 15 minutes of sleep. 2.4.5 Patients with REM related respiratory events should be titrated to the pressure that is necessary to treat during that stage of sleep. 2.4.6 2.5 2.6 Document reason for each pressure increase on the APT PAP titration form. Decrease pressure in response to patient awakenings. 2.5.1 Patient awakens to use the restroom. 2.5.2 Patient awakens spontaneously and has difficulty returning to sleep at the current pressure setting. 2.5.3 Document reason for each pressure decrease on the APT PAP titration form. 2.5.4 Remember the overall goal of determining the appropriate CPAP pressure to treat the patient’s sleep related breathing disorder is to achieve maximum time asleep. Decreasing the pressure can allow the patient to return to sleep promptly. Sleeping position during CPAP titration study. BACK TO TABLE OF CONTENTS 112 PAGE 4 TITLE: Titration of Positive Airway Pressure during Sleep 2.6.1 Let patient begin the night in the sleeping position that is normally used. This should help achieve a shorter sleep onset latency. 2.6.2 Tech can ask patient to move to supine position. 2.6.2.1 When taking a restroom break. 2.6.2.2 After a spontaneous awakening. 2.6.2.3 After a significant period of sleep time and patient has not spontaneously moved to the supine position. 2.6.2.4 3.0 Changing patients sleeping position to supine is contraindicted if the patient has had a back or spine injury. Problem solving during the CPAP titration process. 3.1 Air leak – most lab titration machines will compensate for a degree of air leak. 3.1.1 Complaints of air leaks around the mask and in the eyes. 3.1.1.1 If mask is too big, use a smaller size of the same mask. 3.1.1.2 Re-size using a different style mask. 3.1.1.3 Change to nasal pillows type system. 3.1.1.4 Change to oral interface if indicated. 3.1.1.5 Check tightness of headgear straps to position of forehead pad or adjustment device and make changes as indicated. BACK TO TABLE OF CONTENTS 113 PAGE 5 TITLE: Titration of Positive Airway Pressure During Sleep 3.1.2 3.2 3.1.2.1 Add chin strap 3.1.2.2 3.1.2.3 3.1.2.4 3.1.2.5 Add heated humidity. Add thermistor under the mask to get signal. Consider full face mask. Increasing pressure can resolve mouth breathing. Nasal dryness or soreness. 3.2.1 3.2.2 3.3 Excessive oral leak can lead to a decrease in the CPAP flow signal and may be observed by audio and video surveillance or entering the patient room. Add humidity. 3.2.1.1 Passover humidity. 3.2.1.2 Heated humidity. Have patient use water soluble moisturizer in nares. 3.2.2.1 Saline gel. 3.2.2.2 K-Y Jelly ® 3.2.2.3 RoEzlt ® moisturizer or Nasal Moist ® gel. Claustrophobia. Patients may feel claustrophobic for the first time in their life when they attempt CPAP. 3.3.1 During the hook up procedure, ask the patient if they have experienced claustrophobia. Suggest an interface other than the mask. 3.3.2 Could be caused by anxiety of the testing procedure. BACK TO TABLE OF CONTENTS 114 PAGE 6 TITLE: Titration of Positive Airway Pressure During Sleep 3.4 3.5 3.3.3 Could be panic response to the mask being placed on the face and the pressure initiated. 3.3.4 If patient awakens after sleeping with CPAP, determine if the claustrophobic feeling is related to nasal congestion and if so, use appropriate intervention. 3.3.5 If patient awakens after sleeping with using a nasal mask, change to nasal pillows or other type of interface. 3.3.6 Elevating the patients head with a bed wedge type of device or equivalent may be helpful in addressing the patient’s panic response to the PAP device. Nasal bridge soreness. 3.4.1 Make sure mask size is appropriate. 3.4.2 Adjust fit of nasal mask by adjusting forehead piece. 3.4.3 Loosen headgear straps. Nasal congestion caused by inflammation in the nares associated CPAP titration process. 3.5.1 Add humidity – Passover or heated. 3.5.2 If approved by medical director, use oxymetazolone (Afrin®) for short term relief. Contraindiction for patients with tachyarrhythmia. 3.5.3 Use saline spray. 3.5.4 Apply an external nasal dilator tape ( Breathe-Right® Nasal Strips) 3.5.5 Discontinue CPAP titration and resume with baseline recording with thermistor for a period of time to allow nasal congestion to resolve, then re-initiate Nasal CPAP titration. BACK TO TABLE OF CONTENTS 115 PAGE 7 TITLE: Titration of Positive Airway Pressure during Sleep 3.6 Cheyne Stokes respiration pattern. 3.6.1 Titrate pressure slowly based on arousal and desaturation. Increasing the pressure too rapidly as well as higher pressures may lead to increased duration of the central apnea component. 3.6.2 Change to Bi-Level PAP. 4.0 Bi-Level Positive Airway Titration (Bi-level PAP) Switch patient from CPAP to BIPAP when CPAP pressure needed is greater than or equal to 15 or persistent Hypoxemia despite adequate CPAP titration. 4.1 Terms defined. 4.1.1 Inspiratory positive airway pressure – IPAP. 4.1.1.1 4.1.2 Pressure required to open the airway on inspiration. Expiratory positive airway pressure – EPAP. 4.1.2.1 Pressure required to maintain the airway open during expiration. 4.2 Explain the Bi-level PAP titration process so the patient will understand that there is a lower pressure on expiration. 4.3 Instruct the patient on how to contact technologists during PAP titration. 4.4 Follow steps 1.5 and 1.6 above. 4.5 Titration of Bi-level PAP. 4.5.1 Increase IPAP pressure 2.0 cm higher than ending EPAP/CPAP pressure (ending optimal CPAP pressure if available). Switch to Spontaneous Mode. B-Level is now initiated. BACK TO TABLE OF CONTENTS 116 PAGE 8 TITLE: Titration of Positive Airway Pressure during Sleep 4.5.2 If hypopneas, desaturations, respiratory arousals, or snoring is observed, increase IPAP pressure by 2.0 cm. If apnea (obstructive, mixed, central), increase EPAP pressure by 2.0 cm. Keep the difference between inspiratory and pressure at least 4 4.6 Starting presure for bilevel titration. 4.6.1 Switch from CPAP start with EPAP presure of (8) cmh20 and IPAP presure of (12) cmh20. 4.6.2 Starting titration with BIPAP 4.6.2.1 If first time titration start with EPAP presure of 6 cmh20 and IPAP 10 cmh20 4.6.2.2 If retitration BIPAP or CPAP follow the instruction for switching from CPAP to BIPAP. BACK TO TABLE OF CONTENTS 117 Policy and Procedure TITLE: Titration of Positive Airway Pressure During Sleep for Patients 13 years old and under. ORIGINAL DATE: 01-04-2012 EFFECTIVE DATE: 01-04-2011 REVIEW DATE(s): 01-04-2012 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 PURPOSE: To insure consistency among polysomnographic technologists in the sleep disorders center while performing positive airway pressure (PAP) titration studies. Positive airway pressure is a non-invasive treatment of sleep related breathing events and requires titrating the pressure to eliminate respiratory events, repetitive EEG arousals, oxygen desaturation, and snoring. POLICY: Positive airway pressure titration is to be initiated on order of the sleep disorders center medical director. A written protocol for performing split night studies can be utilized when appropriate. This policy covers both continuous positive airway pressure (CPAP) titration and bi-level positive airway pressure (Bi-Level PAP). PROCEDURE: 1.0 Patient Orientation and Preparation 1.1 1.2 1.3 1.4 Review patient intake sheet and physician’s order for titration. Obtain and document baseline oxygen saturation while the patient is awake and in the following positions- sitting up and supine. Have the patient view a video on PAP titration. 1.3.1 Have TV and DVD equipment set up in patient room prior to patient arrival. 1.3.2 Allow adequate time for viewing and questions. Explain PAP procedure to the patient and Parent or Guardian. 1.4.1 Describe the titration process to allow the patient to know that the pressure will be titrated during the study. BACK TO TABLE OF CONTENTS 118 PAGE 2 TITLE: Titration of Positive Airway Pressure during Sleep 1.4.2 Instruct the patient on how to contact technologist during PAP titration. 1.5 .1 Facial deformalities can be caused by the pressure on the face from a PAP interface, proper fitting is important. Fit the patient with the appropriate PAP interfaces, i.e. mask, nasal pillows, and appropriate headgear etc according to the special instructions given by the Sleep Medicine Physician. 1.6 2.0 1.5.2 Ask the patient if there are any initial concerns about using PAP therapy during the study. 1.5.3 After the appropriate PAP interface has been selected, allow the patient to hold the mask to his/her face at a low pressure prior to securing with headgear. 1.5.3.1 Allow patient to have control over removing the interface if the pressure becomes overwhelming. 1.5.3.2 Instruct patient on how to remove the mask after it is secured with the headgear and again, explain how to signal for the technologist. Document interface type and size on APT technical summary form as well as any nasal patency issues. Titration of CPAP 2.1 Monitor CPAP flow signal from titration equipment to the acquisition equipment through a DC channel if required. 2.1.1 2.2 Alternatively, place thermistor under mask or in designated nasal pillow shell for flow signal. Initiate CPAP at a level of 4 cm H2O. BACK TO TABLE OF CONTENTS 119 PAGE 3 TITLE: Titration of Positive Airway Pressure During Sleep 2.2 2.3 2.4 CPAP may be initiated at a higher level per patient request or physician order. Document reason Determine that the patient is in a comfortable position and check for interface leaks. Make necessary adjustments. Titrate CPAP pressure to eliminate respiratory events, oxygen desaturation, snoring and EEG arousals. 2.4.1 Increase pressure in 1 cm H2O increments. 2.4.2 If patient is sensitive to pressure increases, increments of 0.5 cm H20 may be used. 2.4.3 Increase CPAP level if at least 3 or more hypopneas, reras or obstructives are present. 2.4.4 Adequate time should be allowed for patient to acclimate to the pressure at each increment at least 15 minutes of sleep. 2.4.5 Patients with REM related respiratory events should be titrated to the pressure that is necessary to treat during that stage of sleep. 2.4.6 2.5 2.6 Document reason for each pressure increase on the APT PAP titration form. Decrease pressure in response to patient awakenings. 2.5.1 Patient awakens to use the restroom. 2.5.2 Patient awakens spontaneously and has difficulty returning to sleep at the current pressure setting. 2.5.3 Document reason for each pressure decrease on the APT PAP titration form. 2.5.4 Remember the overall goal of determining the appropriate CPAP pressure to treat the patient’s sleep related breathing disorder is to achieve maximum time asleep. Decreasing the pressure can allow the patient to return to sleep promptly. Sleeping position during CPAP titration study. BACK TO TABLE OF CONTENTS 120 PAGE 4 TITLE: Titration of Positive Airway Pressure during Sleep 2.6.1 Let patient begin the night in the sleeping position that is normally used. This should help achieve a shorter sleep onset latency. 2.6.2 Tech can ask patient to move to supine position. 2.6.2.1 When taking a restroom break. 2.6.2.2 After a spontaneous awakening. 2.6.2.3 After a significant period of sleep time and patient has not spontaneously moved to the supine position. 2.6.2.4 3.0 Changing patients sleeping position to supine is contraindicted if the patient has had a back or spine injury. Problem solving during the CPAP titration process. 3.1 Air leak – most lab titration machines will compensate for a degree of air leak. 3.1.1 Complaints of air leaks around the mask and in the eyes. 3.1.1.1 If mask is too big, use a smaller size of the same mask. 3.1.1.2 Re-size using a different style mask. 3.1.1.3 Change to nasal pillows type system. 3.1.1.4 Change to oral interface if indicated. 3.1.1.5 Check tightness of headgear straps to position of forehead pad or adjustment device and make changes as indicated. BACK TO TABLE OF CONTENTS 121 PAGE 5 TITLE: Titration of Positive Airway Pressure During Sleep 3.1.2 3.2 3.1.2.1 Add chin strap 3.1.2.2 3.1.2.3 3.1.2.4 3.1.2.5 Add heated humidity. Add thermistor under the mask to get signal. Consider full face mask. Increasing pressure can resolve mouth breathing. Nasal dryness or soreness. 3.2.1 3.2.2 3.3 Excessive oral leak can lead to a decrease in the CPAP flow signal and may be observed by audio and video surveillance or entering the patient room. Add humidity. 3.2.1.1 Passover humidity. 3.2.1.2 Heated humidity. Have patient use water soluble moisturizer in nares. 3.2.2.1 Saline gel. 3.2.2.2 K-Y Jelly ® 3.2.2.3 RoEzlt ® moisturizer or Nasal Moist ® gel. Claustrophobia. Patients may feel claustrophobic for the first time in their life when they attempt CPAP. 3.3.1 During the hook up procedure, ask the patient if they have experienced claustrophobia. Suggest an interface other than the mask. 3.3.2 Could be caused by anxiety of the testing procedure. BACK TO TABLE OF CONTENTS 122 PAGE 6 TITLE: Titration of Positive Airway Pressure During Sleep 3.4 3.3.3 Could be panic response to the mask being placed on the face and the pressure initiated. 3.3.4 If patient awakens after sleeping with CPAP, determine if the claustrophobic feeling is related to nasal congestion and if so, use appropriate intervention. 3.3.5 If patient awakens after sleeping with using a nasal mask, change to nasal pillows or other type of interface. 3.3.6 Elevating the patients head with a bed wedge type of device or equivalent may be helpful in addressing the patient’s panic response to the PAP device. Nasal bridge soreness. 3.4.1 To help prevent facial deformities from the pressure of the Cpap mask being on the pediatric face follow the special instructions from the Sleep Physician on which mask to use. 3.4.2. Make sure mask size is appropriate. 3.5 3.4.3 Adjust fit of nasal mask by adjusting forehead piece. 3.4.4 Loosen headgear straps. Nasal congestion caused by inflammation in the nares associated CPAP titration process. 3.5.1 Add humidity – Passover or heated. 3.5.2 If approved by medical director, use oxymetazolone (Afrin®) for short term relief. Contraindiction for patients with tachyarrhythmia. 3.5.3 Use saline spray. 3.5.4 Apply an external nasal dilator tape ( Breathe-Right® Nasal Strips) BACK TO TABLE OF CONTENTS 123 PAGE 7 TITLE: Titration of Positive Airway Pressure during Sleep 3.5.5 Discontinue CPAP titration and resume with baseline recording with thermistor for a period of time to allow nasal congestion to resolve, then re-initiate Nasal CPAP titration. 3.6 Cheyne Stokes respiration pattern. 3.6.1 Titrate pressure slowly based on arousal and desaturation. Increasing the pressure too rapidly as well as higher pressures may lead to increased duration of the central apnea component. 3.6.2 Change to Bi-Level PAP. 4.0 Bi-Level Positive Airway Titration (Bi-level PAP) Switch patient from CPAP to BIPAP when CPAP pressure needed is greater than or equal to 15 or persistent Hypoxemia despite adequate CPAP titration. 4.1 Terms defined. 4.1.1 Inspiratory positive airway pressure – IPAP. 4.1.2 Pressure required to open the airway on inspiration. 4.1.3 Expiratory positive airway pressure – EPAP. 4.1.4 Pressure required to maintain the airway open during expiration. 4.2 Explain the Bi-level PAP titration process so the patient will understand that there is a lower pressure on expiration. 4.3 Instruct the patient on how to contact technologists during PAP titration. 4.4 Follow steps 1.5 and 1.6 above. 4.5 Titration of Bi-level PAP. BACK TO TABLE OF CONTENTS 124 PAGE 8 TITLE: Titration of Positive Airway Pressure during Sleep 4.5.1 Increase IPAP pressure 1.0 cm higher than ending EPAP/CPAP pressure (ending optimal CPAP pressure if available). Switch to Spontaneous Mode. B-Level is now initiated. 4.5.2 If hypopneas, desaturations, respiratory arousals, or snoring is observed, increase IPAP pressure by 1.0 cm. If apnea (obstructive, mixed, central), increase EPAP pressure by 1.0 cm. Keep the difference between inspiratory and pressure at least 4cm H20 apart. 4.6 Starting pressure for bilevel titration. 4.6.1 Switch from CPAP start with EPAP presure of (4) cmh20 and IPAP presure of (8) cmh20. 4.6.3 Starting titration with BIPAP 4.6.3.1 If first time titration start with EPAP presure of 4 cmh20 and IPAP 8 cmh20 4.6.3.2 If retitration BIPAP or CPAP follow the instruction for switching from CPAP to BIPAP. BACK TO TABLE OF CONTENTS 125 Policy and Procedure TITLE: Protocol for Follow up Calls after CPAP ORIGINAL DATE: 11-11-2011 EFFECTIVE DATE: 11-11-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 Purpose ; To ensure patient compliance with treatment use and response to Pap therapy. Policy: Sleep Center of Kentuckiana believes that continuing medical care is as important as the initial treatment. As long as follow up calls will improve patient care and give our staff back up information regarding our service so we can improve service. Sleep Center of Kentuckiana is planning to perform follow up calls within 48 to 72 hours from the initial visit. Procedure: 1. Sleep Center of Kentuckiana personnel is going to perform these calls. 2. Introduce the facility and caller and position. 3. Ask for the patient (guardian if minor or demented). 4. Avoid giving any information to anyone except the patient or guardian. 5. Conversation should include Reason for call which includes the importance of Pap compliance and face to face follow up appointments with their Sleep Medicine Specialist. Patients should have a face to face appointment with the Sleep Medicine Specialist in 30, 60 and 90 days after titration then on yearly basis unless Pap compliance wasn’t met. The patient will follow up in 30 days after office visit if Pap compliance is less than 80% on any visit. Patient to bring their Smart Card to be down loaded to prove compliance. If the referring physician has not specified a DME, upon patient request a DME would be provided. If there is an answering machine or patient not available leave brief message for patient to call back only. The office is open Monday – Friday from 9am-5pm and our answering machine is on after hours and calls will be returned the next business day. BACK TO TABLE OF CONTENTS 126 ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Split Night Study EFFECTIVE DATE: 09-01-2006 REVISION DATE(s): 03/08/2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To provide a process to combine the diagnostic and diagnostic positive airway pressure (PAP) titration portions of the evaluation process. This includes both continuous PAP and bi-level PAP titration processes. POLICY: Split night studies require that specific requirements are met during the diagnostic portion to initiate PAP therapy. Technicians should explain to the patient that PAP therapy may be substituted during the night if the requirements in the split night study procedure. This policy will cover criterion for initiating PAP during a diagnostic study. These guidelines meet Centers for Medicare and Medicaid Services (CMS) requirements for home PAP use. Note: CMS allows sleep studies performed in a facility based sleep lab only. The Sleep Disorders Center medical director may designate adjustments in criterion below. PROCEDURE: 1.0 Criterion for initiating PAP during a diagnostic study. 1.1 2 hours of TST has occurred. 1.2 AHI ≥ 40/hour. 1.3 Hypopneas associated with a 4% drop in SpO2 from baseline SpO2. 1.4 AHI 20 – 40 with other symptoms: If patient has severe Hypoxia or Cardiac Arrythmias 1.4.1 1.4.2 1.4.3 Insomnia. Hypertension. Ischemic Heart Disease. BACK TO TABLE OF CONTENTS 127 PAGE 2 TITLE: Split Night Study 1.4.4 2.0 History of Stroke. Titration. 2.1 Allow 3 hours for titration procedure. 2.2 Follow CPAP titration protocol. BACK TO TABLE OF CONTENTS 128 Policy and Procedure TITLE: Oral/Nasal – Full Face Masks ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/8/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 To ensure proper equipment utilization and to maintain patient safety. POLICY: 1.0 Interface for positive airway pressure diagnostic evaluations. 1.1 Nasal masks or nasal pillows type of interface should be utilized first. 2.0 Oral leaks 2.1 Chin straps or other type of device such as Chin-Ups can be used for oral leaks. 2.2 Oral nasal or full face masks 2.2.1 Oral-nasal or full face masks may be used only when the precautions are followed: 2.2.1.1 The patient may not eat or drink during the sleep test. 2.2.1.2 The patient may not have eaten three (3) hours before wearing of the oral-nasal or full face mask. 2.2.1.3 The oral-nasal or full face mask must have a safety valve to enable the patient to breathe room air in case of power failure or equipment malfunction. 2.2.1.4 When applying the oral-nasal or full face mask, do not retract the jaw. 2.2.1.5 Patients with neuromuscular problem may not use the oralnasal or full face mask unless he/she is able to remove the mask quickly and without assistance. BACK TO TABLE OF CONTENTS 129 PAGE 2 TITLE: Oral/Nasal – Full Face Masks Procedure: 1.0 Fitting Oral-Nasal or Full Face Masks 1.1 Size with the mouth open. The bridge of the nose and below the lower lip should be used as the landmarks. Some manufacturers have measuring devices to aid in this process. 1.2 Instruct the patient about the proper usage of the mask. 1.2.1 Explain how to remove the mask quickly in the event of emesis. 1.2.2 Explain the safety valve feature to the patient. 1.2.3 Document on forms the reason(s) why the oral-nasal or full face mask was utilized. Include all of the masks that were attempted. BACK TO TABLE OF CONTENTS 130 Policy and Procedure TITLE: Monitoring Oxygen Saturation Levels and Administration of Oxygen during Polysomnography ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To maintain the highest standards of care in providing supplemental oxygen to patients. Oxygen saturation is monitored continuously during the polysomnogram with a pulse oximeter interfaced to the acquisition equipment. POLICY: 1.0 General Considerations 1.1 Obtain SPO2 baseline level during wake. 1.1.1 Prior to patient calibrations, apply oximeter probe to patient. 1.1.2 Request that the patient sit upright, be still and then record the waking SpO2 saturation level as it appears in the oximeter display after stabilization. 1.2 Document SpO2 level in the patient record. 1.2.1 Use of O2, liter flow and oximeter readings. 1.2.2 Include in patient chart and on polygraph. 1.3 For SpO2 baseline levels below 90%*. 1.3.1 Verify correct placement, adequate perfusion and insure functionality of oximeter probe. 1.3.2 Telephone physician on call or medical director as directed. BACK TO TABLE OF CONTENTS 131 PAGE 2 TITLE: Monitoring Oxygen Saturation Levels and Administration of Oxygen during Polysomnography. 1.0 Monitoring SpO2 levels during sleep. 1.1 1.2 2.0 In the absence of sleep disordered breathing (SDB), oxygen saturation levels should be maintained at 90%* or above. Should SpO2 baseline level remain below 90%, telephone physician on call or medical director to report finding as directed. Monitoring SpO2 levels during positive airway pressure (PAP) titrations. 2.1 If patient is using supplemental oxygen, discontinue at start of PAP titration. 2.1.2 If the patient begins to show signs of sustained hypoxemia (with a SpO2 below 88% for five (5) consecutive minutes¹) after elimination of respiratory events OR if patient is demonstrating desaturation swings and not returning to baseline within 30 seconds, telephone physician or medical director on call to report finding. 2.1.3 Cardiac conditions that may warrant supplemental O2. (Consult the medical director to determine lab specific policy.) 2.1.3.1 2.1.3.2 2.1.3.3 2.1.3.4 2.1.4 3.0 Frequent PVCs. Bigeminy Trigeminy Cheyne Stokes Respiration Congestive Heart Failure (CHF) or Overlap Syndrome patients may also benefit from supplemental oxygen as well as patients exhibiting ventricular arrythmias. (Consult the medical director in determining lab specific policy.) Supplemental Oxygen. 3.1 Supplemental oxygen administration. 3.1.1 Obtain order from physician for oxygen administration and provide documentation in the patient record. BACK TO TABLE OF CONTENTS 132 PAGE 3 TITLE: Monitoring Oxygen Saturation Levels and Administration of Oxygen during Polysomnography. 3.1.1.1 4.0 Initiate oxygen via nasal cannula using the physician prescribed flow range. 3.1.1.2 Increase oxygen flow in increments of 0.5 liters per minute (LPM) until prescribed range has been met. 3.1.1.3 Maximum amount of oxygen to be delivered via nasal cannula is 6.0 lpm². If a patient arrives in the center already on oxygen > 6 LPM, call the medical director for instructions. 3.2 Supplemental oxygen administration on PAP. 3.2.1 Obtain order from physician for oxygen administration and provide documentation in the patient record. 3.2.2 Entrain oxygen at prescribed flow to PAP machine. 3.2.2.1 Increase oxygen flow increments of 0.5 LPM until prescribed range has been met. Lab specific considerations. 4.1 Location of nasal cannulas. 4.2 Location of oxygen delivery device(s). 4.3 Use of flow meter. 4.3.1 Flow meters are of the compensated, Thorpe Tube design. 4.3.1.1 Easily push into the wall unit. 4.3.1.2 Built into the compressors or other gas delivery devices. 4.3.2 Set and read the flow meter. 4.3.2.1 Float device, typically a small steel ball, is suspended in the tube by the difference in pressure of the gas below it and above it. BACK TO TABLE OF CONTENTS 133 Page 4 TITLE: Monitoring Oxygen Saturation Levels and Administration of Oxygen during Polysomnography. 4.3.2.2 4.3.2.3 4.3.2.4 1. 2. Hash marks are associated with numbers that indicate the liter flow per minute usually in increments of 0.5 liters. Operate flow meter by turning the knob clockwise until the ball begins to float. Flow meter is properly set when the suspended float is in the middle of the hash mark. CMS R.A.D. guidelines. Clinical Application of Respiratory Care, Shaprio, 1991, p. 129. BACK TO TABLE OF CONTENTS 134 Policy and Procedure TITLE: Multiple Sleep Latency Test (MSLT) ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s):03-01-2007 3-08-2011 REVISION DATE(s):03-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 DEFINITION: MSLT provides information about somnolence (sleepiness) and the presence of abnormal sleep onset REMs (narcolepsy). POLICY: MSLT shall be performed during the day following a nocturnal polysomnography. Five (5) naps will be scheduled at two (2) hour intervals. The first nap will begin one and one-half to three (1-1/2 to 3) hours after the ending of the polysomnography. The testing room shall be free from noise. PROCEDURE: Instruct patient not to drink alcohol and/or caffeinated beverages before and during the test. Obtain a urine specimen from the patient. Document medications the patient is taking, dose and time taken. Use the standard MSLT montage. BACK TO TABLE OF CONTENTS 135 Page 2 TITLE: Multiple Sleep Latency Test (MSLT) Set up all equipment, prepare sensors. Attach all electrodes/sensors to patient. Perform a machine calibration before the fist nap and at the end of the last nap. Perform patient calibrations. Patient instructions: Do not move. Keep eyes open (30 seconds). Close eyes (30 seconds). Open eyes, keep head still, look up and then down. Repeat as necessary. Now look left then right with eyes only. Do not move your head. Blink your eyes five (5) times. Swallow, grit teeth and smile. Instruct patient to complete MSLT Questionnaire. Instruct patient to get in a comfortable sleep position and do not resist sleep. This begins #1 nap. Enter exact time and epoch number on observation form. Enter lights out, position tags in computer. If the patient has not fallen asleep within 20 minutes of lights out, the test is ended. If the patient falls asleep, the nap is continued for 15 minutes before ending. Document all observations. If the patient has fallen asleep, gently wake him/her up. Instruct patient to complete post-test questionnaire. BACK TO TABLE OF CONTENTS 136 ORIGINAL DATE: 10-03-2011 REVIEW DATE(s): APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Portable Testing EFFECTIVE DATE: 10-03-2011 REVISION DATE(s): TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: PURPOSE: To be used as a screening device for obstructive sleep apnea on patient population who would otherwise be unable to attend a routine polysomnography study in the lab. Pulse oximetry provides estimates of arterial oxyhemoglobin saturation (SaO2) by utilizing selected wavelengths of light to determine the saturation of oxyhemoglobin (SpO 2) in a noninvasive manner. NECESSITY/JUSTIFICATION: Morbidly obese patient who is unable to ambulate Hospital bound and or bed bound patient who is unable to be moved to attend a routine polysomnography testing. GENERALLY ORDERED FOR PATIENTS WHEN: All patients will be monitored with pulse oximetry, effort, Thermister, EKG. Portable equipment is appropriate for continuous and prolonged monitoring, such as during sleep. PATIENT OUTCOME: The following should be utilized to evaluate the benefit of pulse oximetry: SpO2 results should reflect the patient’s clinical condition (i.e., validate the basis for ordering the test). BACK TO TABLE OF CONTENTS 137 Page 2 TITLE: Portable Testing Documentation of results, therapeutic intervention (or lack of), and/or clinical decisions based on the SpO2 measurement should be noted in the medical record. EQUIPMENT/SUPPLIES: Portable equipment and related accessories (probe of appropriate size). Stardust, PDX. BACK TO TABLE OF CONTENTS 138 ORIGINAL DATE: 10-03-2011 REVIEW DATE(s): APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Portable Testing Trainee EFFECTIVE DATE: 10-03-2011 REVISION DATE(s): TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: Position Summary A Portable Trainee develops competency in and performs the basics of polyosomnographic testing and associated interventions under direct supervision of a Registered Polysomnographic Technician and the Medical Director. Domains of Practice Gather and Analyze Patient Information Verify the medical order and protocol. Complete and verify documentation. Explain the procedure to the patient. Testing Preparation Procedures Prepare and examine the equipment required for testing to determine proper functioning. Apply electrodes and sensors according to accepted published standards. Which include the pulse oximetery, effort belts, thermistor, Eog, chin, legs and ekg Color-Coded Labels – located around the perimeter of the device, indicate where to connect the various sensor leads. The display shows the patient and Technician only the sensors that need to be connected. The sensor information and indicators help patients and Technicians place the sensors correctly and reduce the need for retesting due to application errors. Polysomonographic Procedures After applying the electrodes and sensors check the Good Study Indicator. The Good Study Indicator is predicated on airflow and oximeter signal quality. It displays the amount of "good quality data" needed for a study to be complete and valid. The indicator measures patient airflow, gathered by the nasal cannula and/or the oral thermistor, airflow from therapy devices, and pulse oximetry, gathered by the SpO2 sensor. BACK TO TABLE OF CONTENTS 139 Page 2 Portable Testing Trainee Without either of these signals, the sleep study would be declared diagnostically invalid because of insufficient data. Service Management and Professional Issues Comply with applicable laws, regulations, guidelines and standards regarding safety and infection control issues. Participate in equipment care and maintenance. Maintain current CPR certification. Demonstrate effective written and spoken communication skills. BACK TO TABLE OF CONTENTS 140 Fatigue, Sleepiness and Driving Excessive fatigue and sleepiness can be the result of a number of factors sleep deprivation, shiftwork, or a sleep disorder can contribute greatly to your inability to remain alert and attentive behind the wheel of a motor vehicle. The national highway traffic safety administration estimate that there are a minimum of 100,000 crashes and 1,500 deaths annually, as a direct result of driver fatigue. They also report that drowsiness plays a role in another 1 million crashes caused by driver inattention. In addition the national sleep foundation states that in an annual poll of adults ages 18-54, 60% of respondents report driving while feeling drowsy. With this information in mind, we feel it is our responsibility to advise each of our patient with symptoms of fatigue and daytime sleepiness of the need to remain alert while driving. If sleepiness is so intense that it impairs the ability to drive safely, we advise that driving be avoided altogether until diagnosis and treatment has eliminated the sleepiness. Please acknowledge that you have been advised of this information with your signature below. Signature:---------------------------------------- Date:--------------------------------- BACK TO TABLE OF CONTENTS 141 Quality Improvement Patient Name:-------------------------------------Sleep Tech Name:--------------------------------Safety _____ Location of emergency guidelines and phone number list _____ Location of fire extinguishers and their uses _____ Alert beeper location, uses, and reset button location _____ Disposes of sharps as needed _____ Understands fire protocol _____ Utilizes proper hand washing technique and protocol _____ Utilizes power/equipment failure protocol _____ Utilizes tornado protocol _____ Observes no smoking policy Equipment _____ Performs NPSG, CPAP/BIPAP acquisition setup on Alice 5 _____ Performs MSLT acquisition on Alice 5 _____ Calibrates Alice 5 to Oximeter, CPAP/BIPAP correctly _____ Impedance checked and corrected if needed _____ Bio Cals performed _____ Patient Cals before lights off and after lights on _____ Fits patient with proper masks and headgear _____ Correct oximeter and probe placement _____ Disinfects all equipment used and stores properly _____ Operates patient monitor and camera switch properly Tech needs improvement with: ____ Hook-Up ____ Artifact ____ Documentation ____ Satisfactory Technical Director ___________________ Medical Director _____________ BACK TO TABLE OF CONTENTS 142 Policy and Procedure TITLE: Maintenance of Wakefulness Test (MWT) ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President PURPOSE: Telephone: (502) 387-6133 The Maintenance of Wakefulness Test (MWT) is used as a quantitative polysomnography which measures daytime wakefulness / somnolence tendency during sleep-inducing circumstances. POLICY: 1.0 GENERAL CONSIDERATIONS 1.1 Completed prior to evaluation. 1.1.1 A sleep diary recommended based on clinical judgement of medical director. 1.2.1 Patient sleep questionnaire with medication log and drug history. 1.2 Recommend discontinuation of medications including stimulants, alcohol, and anti-depressants as determined by the sleep clinician. 1.3 Polysomnogram (PSG) testing is recommended based on clinical judgement of medical director. Examples of potential reasons for exclusion :MWT would be contraindicated in individuals with respiratory disturbance indexes (RDI) greater than 10, lowest oxyhemoglobin saturation less than 85%, periodic limb movement/arousal index less than ten, or significant reduction in total sleep time (TST). 1.4 MWT should be performed with patient dressed in street clothes. 1.5 The MWT consists of four 40-minute testing periods scheduled at twohour intervals.² 1.6 The patient must abstain from caffeine during the MWT procedure. BACK TO TABLE OF CONTENTS 143 PAGE 2 TITLE: Maintenance of Wakefulness Test (MWT) 1.7 A urine drug screen (UDS) may be obtained the morning of, or during the MWT to identify patients whom drug effects are suspected per recommendation of the sleep clinician. 1.7.1 If a UDS is deemed necessary, consent from patient must be obtained. 1.8 If light measurement device is available, a setting of 0.10 to 0.13 lux at the corneal level is recommended or a standardized 7.5 watt night light may be utilized. It is recommended that indirect lighting be placed in the testing room. 1.9 Patient should be placed in a comfortable sitting position. This can be accomplished by placing the patient in a comfortable chair or sitting in bed, back and head supported by a bed rest such that the neck is not uncomfortably flexed/extended. 1.10 Room temperature should be set to the patient’s comfort. 1.11 A technologist trained and skilled in conducting the MWT procedure must perform test. 1.12 Continuous observation between testing periods is essential. PROCEDURE: 1.0 General Protocol. 1.1 Obtain UDS per physician order. 1.1.1 Obtain consent from patient prior to UDS. 1.2 Follow the policy on Patient Arrival, Preparation and Electrode / Sensor Application on page 55. 1.3 Equipment and physiological calibrations should be done before and after the MSLT nap opportunity. Refer to policy on Physiological Calibration Procedures on page 59 and policy on Equipment Calibrations on page 63. BACK TO TABLE OF CONTENTS 144 PAGE 3 TITLE: Maintenance of Wakefulness Test (MWT) 1.4 Verify all information received from patient at time of evaluation. 2.0 Recording Parameters. 2.1 2.2 3.0 EEG (C3, C4, F3, F4, O1, O2) EOG (ROC, LOC) 2.2.1 Right Horizontal (or oblique) EOG 2.2.2 Left Horizontal (or oblique) EOG 2.3 EMG (Mental, Submental) 2.4 EKG Perform the MWT consistently in the following manner. 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 The first test period will be initiated one and a half to two hours from patient’s usual wake up time or the termination of the PSG, if recommended by the sleep clinician, and should be repeated at two-hour intervals until four tests have been performed. A quiet and dark room with minimal noise should be used. The patient should be in the testing position 10 minutes prior to the start of the test period. The patient should complete the Stanford Sleepiness Scale before each MWT test period. 5 minutes prior to lights out, patient should be in bed and the head box connected to the PSG data acquisition equipment. Instruct the patient to resist sleep without using any extraordinary measures of stimulation, such as singing, pinching, tapping feet, etc. Perform equipment and patient bio – calibrations. Instruct the patient “ Please sit still and remain awake as long as possible. Look directly ahead of you and do not look directly into the light.” Initiate the test period . BACK TO TABLE OF CONTENTS 145 PAGE 4 TITLE: Maintenance of Wakefulness Test (MWT) 4.0 5.0 3.10 Technologist should complete MWT Technical Documentation Procedure Form. 3.11 Termination of the test period. 3.10.1 40 minutes if no sleep occurs. 3.10.2 After unequivocal sleep is determined. 3.10.2.1 Sleep onset is defined as 15 seconds of cumulative sleep during a 30 second epoch. 3.10.2.2 Unequivocal sleep is defined as three consecutive 30-second epochs of stage 1; or any one 30-second epoch of any other stage of sleep. 3.12 Have the patient complete the MWT Post Questionnaire. 3.13 Repeat steps 3.1 to 3.11 for a total of four test periods. 3.14 Remove electrodes and follow discharge protocol. DOCUMENTATION 4.1 Complete the MWT Technical Procedure Documentation Form during each testing period. 4.2 Complete Stanford Sleepiness Scale before each testing period. 4.3 Complete the MWT Patient Questionnaire before and after each test period. SLEEP STAGE SCORING 5.1 Score sleep stages according to AASM scoring manual.³ 5.2 Sleep Latency (SL) is defined as the testing period onset (“Start Time”) to the first epoch of any sleep stage. 5.3 Sleep latency, total sleep time, total wake time and stages of sleep should be documented for each test period. BACK TO TABLE OF CONTENTS 146 PAGE 5 TITLE: Maintenance of Wakefulness Test (MWT) 6.0 7.0 REPORT 6.1 Lights out and lights on times of each nap or nap opportunity. 6.2 Sleep onset latency. 6.3 Mean sleep latency. INTERPRETATION 7.1 Impairment of wake tendency exists if the mean sleep latency (MSL) is less than 11 minutes. BACK TO TABLE OF CONTENTS 147 Policy and Procedure TITLE: Inter-Scorer Reliability Quality Assurance ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURPOSE: Regular assessment of all scoring parameters assures the inter-reliability among scorers. Because the evaluation of sleep stages, respiratory events, plms and arousals is critical in the diagnosis of sleep disorders, it is judicious to complete inter-scoring reliability comparison on 3 studies a quarterly basis for a total of 12 studies a year. The Studies will be reviewed and signed by the Medical Director. The Medical Director will make modifications as needed. Reliability measures should be reviewed quarterly by the quality assurance (QA) team made up of the ABSM certified clinician and/or Medical Director as part of the QA program. POLICY: To provide a mechanism for evaluating inter-scorer reliability. PROCEDURE: 1.0 Evaluation of scored polysomnographic studies 1.1 On a minimum of three studies quarterly, but ideally on a monthly basis, a previously scored sleep record will be selected at random by the sleep disorders center supervisor and/or medical director. 1.2 The record will be scored independently by another technologist who scores patient records on a regular basis. 1.3 The medical director will review the same record and enter those scores on an inter-scoring reliability worksheet 1.4 Results from the worksheet are entered on an inter-scoring reliability QA form for the same patient record where scores are compared. There are 4 parameters to compare ; sleep staging epoch by epoch, respiratory events, PLMSs and arousals on 200 consecutive epochs. BACK TO TABLE OF CONTENTS 148 PAGE 2 TITLE: Inter-Scorer Reliability Quality Assurance 1.5 A score of 90% or better is acceptable. 1.5.1 When the reliability comparison score falls below 90% discrepancies will be reviewed by the scoring sleep center technologist and medical director for further interpretation and mutual resolution. 1.5.2 In the event discrepancies are not understood, the scoring technologist will review the AASM scoring guideline. Those scores will be evaluated and accepted by the medical director and/or sleep disorders center supervisor before the technologists performs record analysis on unscorred records. BACK TO TABLE OF CONTENTS 149 Policy and Procedure TITLE: Quality Assurance Policy ORIGINAL DATE: 3-08-2011 EFFECTIVE DATE: 03-08-2011 REVIEW DATE(s): 03-08-2011 REVISION DATE(s): APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 Purpose : To outline quality assurance process utilized at Sleep Center of Kentuckiana. The QA reports on a quarterly basis will be reviewed by the Medical Director and recommendations for improvements as needed. Policy Statement : To assure high quality patient care for patients seen at Sleep Center of Kentuckiana. Procedure: 1. The following will be monitored on patients for sleep testing and may be use as a Quality Assurance metric: All patients will have hourly checklist form filled out on each standard and Pap titration study based on the patient’s condition and status. To ensure quality recordings the sleep studies are to be reviewed for artifact , documentation , hook up, equipment performance and over all satisfactory by the Clinical Coordinator and the Medical Director. The Medical Director will educate Technicians on corrections accordingly. Patient satisfaction will be monitored and reviewed by the Clinical Coordinator and Medical Director. Patient requiring PAP therapy will follow up at the Sleep Center of Kentuckiana for treatment response and compliance therapy. BACK TO TABLE OF CONTENTS 150 Page 2 Quality Assurance Policy Patients requiring any other treatment responses concerning Sleep Disorders or Pulmonary issues follow up at the Sleep Center of Kentuckiana for treatment. All patients, except for direct referrals, will be evaluated by a Sleep Medicine Specialist prior to scheduling their sleep study. Each patient will complete a consent form giving permission for photography, audio, and video recording during the testing process. All patients will have sleep studies scored and ready to be reviewed by a Sleep Medicine Physician in 3 business days. All patients will have the sleep studies reviewed, modified and signed by a Sleep Medicine Physician in 5 business days. The Medical Director or a staff Sleep Medicine Specialist physician will conduct a monthly meeting with the day and night staff. 2 Inter-scorer Inter-scorer reliability will be conducted per AASM guidelines with 90% agreement between the Sleep Physician and the scoring technologist. Three random studies on a quarterly basis will be reviewed and signed by the Medical Director There are 4 parameters to compare: sleep staging epoch by epoch , respiratory events, PLMSs and arousals on 200 consecutive epochs. If the comparison score is less than 90% the Medical Director will review and educate the Scoring Technician. BACK TO TABLE OF CONTENTS 151 2012 QA Review Quarter Interscorer reliability reports on ID Acq # Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Patient surveys Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Technical artifact, documentation and hook-up Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Follow up compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ CPAP compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records Scored and ready to review Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records reviewed and signed by Sleep Physician Comments_______________________________________ Action for improvement____________________________ _________________________________________________ ------------------------------------Kheder Kutmah M.D., DABSM BACK TO TABLE OF CONTENTS 152 2011 QA Review Quarter one Interscorer reliability reports on ID Acq # 21019, 21024, 21049 Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Patient surveys Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Technical artifact, documentation and hook-up Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Follow up compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Cpap compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records Scored and ready to review Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records reviewed and signed by Sleep Physician Comments_______________________________________ Action for improvement____________________________ _________________________________________________ ------------------------------------Kheder Kutmah M.D., DABSM BACK TO TABLE OF CONTENTS 153 2011 QA Review Quarter two Interscorer reliability reports on ID Acq # 10866, 40751, 21021 Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Patient surveys Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Technical artifact, documentation and hook-up Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Follow up compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ CPAP compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records Scored and ready to review Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records reviewed and signed by Sleep Physician Comments_______________________________________ Action for improvement____________________________ _________________________________________________ ------------------------------------Kheder Kutmah M.D., DABSM BACK TO TABLE OF CONTENTS 154 2011 QA Review Quarter three Interscorer reliablilty reports on ID Acq # 40787, 21068, 21061 Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Patient surveys Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Technical artifact, documentation and hook-up Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Follow up compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ CPAP compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records Scored and ready to review Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records reviewed and signed by Sleep Physician Comments_______________________________________ Action for improvement____________________________ _________________________________________________ ------------------------------------Kheder Kutmah M.D., DABSM BACK TO TABLE OF CONTENTS 155 2011 QA Review Quarter four Interscorer reliablilty reports on ID Acq # 10897, 1303, 1249 Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Patient surveys Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Technical artifact, documentation and hook-up Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Follow up compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ CPAP compliance Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records Scored and ready to review Comments_______________________________________ Action for improvement____________________________ _________________________________________________ Records reviewed and signed by Sleep Physician Comments_______________________________________ Action for improvement____________________________ _________________________________________________ ------------------------------------Kheder Kutmah M.D., DABSM BACK TO TABLE OF CONTENTS 156 Policy and Procedure TITLE: Employee Schedule and Time Off Requests ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 REVISION DATE(s): 03/08/2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: Telephone: TITLE: President (502) 387-6133 PURPOSE: To define a uniform process to make sure all employees understand the Sleep Disorders Center working hours. PURPOSE: To make sure all employees sign in and out at their scheduled work time. PROCEDURE: 1.0 Shift onset 1.1 Employees will clock in and out according to the shift they work. 1.2 Employees will not clock in any earlier than the listed starting time unless they have permission from management. 1.3 The following schedule is in effect: 1.4 2.0 1.3.1 DAY SHIFT: 8:00 a.m. – 5:00 p.m. (or until work is complete) 1.3.2 NIGHT SHIFT: 8:00 p.m. – 6:00 a.m. (or until work is complete) At the end of the employee’s work week put time sheets in folder marked and located in the tech room. Failure to do this is subject to incorrect pay. Unable to work shift 2.1 If unable to work your scheduled shift due to illness or some type of an emergency the Senior Technologist or Department Manager must be notified no later than 1300 hours (earlier when possible) to arrange for proper staffing or rescheduling patients. Failure to do this will be grounds for Disciplinary Action. BACK TO TABLE OF CONTENTS 157 PAGE 2 TITLE: Employee Schedule and Time off Requests 3.0 4.0 Vacation / Holiday Requests 3.1 Requests must be submitted prior to scheduling posting. 3.2 Requests made at the last minute may be granted at the discretion of the sleep disorders center supervisor. Adequate coverage must be maintained. 3.3 No more than one employee at a time will be granted prolonged vacation request depending on shift. 3.4 The sleep disorders center will be closed for most major holidays. 3.5 Requests for emergency leave for death or serious circumstance in the employee’s immediate family will be granted. Accrued PTO time will apply. If extended leave is necessary, contact the sleep disorders center to make arrangements. Changing shifts 4.1 Employees wishing to change days, shifts, etc., should work this out and submit the change in writing with employee’s signatures involved to the sleep disorders center supervisor for approval. Adequate coverage for each shift is to be maintained. BACK TO TABLE OF CONTENTS 158 Addendum – Documents for the Profession, Sample Forms and Policies Job Descriptions for the Polysomnographic Technology Profession………………121 Polysomnographic Trainee…………………………………………………123 Polysomnographic Technician……………………………………………...125 Polysomnographic Technologist……………………………………………127 Polysomnographic Technology Care Competencies Arrival Preparation and Electrode/Sensor Application……………………..129 Capnography………………………………………………………………...131 Maintenance, Cleaning, and Safety Precautions…………………………….133 Monitoring Pulse Oximetry………………………………………………….135 PAP Titration………………………………………………………………...137 Polysomnographic Montages and Equipment Calibration and Function……139 Scoring Sleep Stages and Clinical Events……………………………………141 Supplemental Low Flow Oxygen Titration…………………………………..143 Staff Ratios: Third Shift Staffing…………………………………………………….145 Epworth Sleepiness Scale……………………………………………………………147 MSLT Technical Documentation Form……………………………………………...149 MSLT Pre Sleep Questionnaire………………………………………………………151 MSLT Post Sleep Questionnaire……………………………………………………..153 MWT Technical Documentation……………………………………………………..155 Physician Order Sheet………………………………………………………………..157 Standing Order Policy………………………………………………………………..159 Fire/Evacuation Check List and Responsibilities……………………………………161 Bed Partner Questionnaire……………………………………………………………163 Cancellation Protocol…………………………………………………………………165 CPAP/Bi Level PAP Titration Log Form…………………………………………….167 Sleep Study Flow Chart………………………………………………………………169 Direct Referral Form………………………………………………………………….171 Infection Control Policy………………………………………………………………173 Assembly, Maintenance and Storage of Charts………………………………………175 BACK TO TABLE OF CONTENTS 159 Association of Polysomnographic Technologists The Association of Polysonographic Technologists (APT), the American Academy of Sleep Medicine (AASM), the Board of Registered Polysomnographic Technologists (BRPT) and the American Society of Electroneurodiagnostic Technologists (ASET) established a joint committee to provide recommendations that specifically address the minimum skills and competencies required for Polysomnographic Technologists. This project required the committee to develop a job description model that indicated progression through the learning and development cycle. The committee identified the need to create three levels for the Polysomnographic Technologist position. The first position Polysomnographic Trainee position is an entry-level position. The second position, Polysomnographic Technician indicates successful completion and mastery of certain tasks. The third, Polysomnographic Technologist indicates the individual has mastered tasks and successfully passed the certification process through the BRPT. The three job descriptions focus on qualifications needed for each position and the education and skills required to move to the next level. All three levels are under supervision of the sleep centers clinical director (MD, PhD, DO). The purpose of these job descriptions is to create consistent criteria that can be used on a national basis to show the development of polysomnographic technicians as they enter the profession and progress to become BRPT certified. The following job descriptions have been ratified by the the boards of directors of the APT, AASM, BRPT and ASET. BACK TO TABLE OF CONTENTS 160 Polysomnographic Trainee Position Summary A Polysomnographic Trainee develops competency in and performs the basics of polyosomnographic testing and associated interventions under direct supervision of a Polysomnographic Technician or a Polysomnographic Technologist. Domains of Practice Gather and Analyze Patient Information Verify the medical order and protocol. Complete and verify documentation. Explain the procedure and orient the patient to the sleep center. Testing Preparation Procedures Prepare and calibrate equipment required for testing to determine proper functioning. Apply electrodes and sensors according to accepted published standards. Perform appropriate physiologic calibrations to ensure proper signals. Perform routine positive airway pressure (PAP) mask fitting. Polysomonographic Procedures Follow procedural protocols (such as Multiple Sleep Latency Test (MSLT). Maintenance of Wakefulness Test (MWT), parasomnia studies, PAP and oxygen titration, etc.) to ensure collection of appropriate data. Follow “lights out” procedures to establish and document baseline values (such as body position, oxyhemoglobin saturation, respiratory and heart rates, etc.) Perform polysomnographic data acquisition while monitoring study-tracing quality to ensure signals are artifact-free. Identify and report signal abnormalities. Document routine observations, including sleep stages and clinical events, changes in procedure, and other significant events in order to facilitate scoring and interpretation of polysomnographic results. Assist with appropriate interventions (including actions necessary for patient safety and therapeutic intervention such as continuous and bi-level positive airway pressure, oxygen administration, etc.) Follow “lights on” procedures to verify integrity of collected data and complete the data collection process (e.g. repeats the physiological and instrument calibrations and instructs the patient on completing questionnaires, etc.) Demonstrate the knowledge and skills necessary to recognize and provide age specific care in the treatment, assessment, and education of neonatal, pediatric, adolescent, adult, and geriatric patients. Service Management and Professional Issues Comply with applicable laws, regulations, guidelines and standards regarding safety and infection control issues. Participate in equipment care and maintenance. Maintain current CPR or BCLS certification. Demonstrate effective written and spoken communication skills. BACK TO TABLE OF CONTENTS 161 Polysomnographic Trainee Demonstrate ability to follow direction. Education and/or Experience High school diploma or GED plus 6 months of direct patient care experience or 1 year of postsecondary education. OR Current enrollment in an accredited educational program leading to an associate degree with an emphasis in polysomnography. Physical Demands The physical demands described here are representative of those that must be met by an employee to successfully perform the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. While performing the duties of this job, the employee is frequently required to stand; use hands to finger, handle or feel; reach with hands and arms; climb or balance; and talk or hear. The employee is occasionally required to walk, sit, and stoop, kneel, crouch or crawl. The employee must regularly lift and/or move up to 10 pounds, frequently lift and/or move up to 25 pounds, and occasionally lift and/or move up to 50 pounds. Specific vision abilities required by this job include close vision, distance vision, color vision, peripheral vision, depth perception, and ability to adjust focus. Work Environment The work environment characteristics described here are representative of those an employee encounters while performing the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. In the performance of this job, the employee may be exposed to chemical vapors such as acetone, ether, or glutaraldehyde. There may also be skin contact with these substances. The employee may also be exposed to infectious agents including blood-borne pathogens. BACK TO TABLE OF CONTENTS 162 Polysomnographic Technician Position Summary A Polysomnographic Technician performs comprehensive polysomnographic testing and analysis and associated interventions under the general oversight of a Polysomnographic Technologist (RPSGT) and/or the clinical director (MD, PhD, DO) or designee. A Polysomnographic Technician can provide supervision of a Polysomnographic Trainee. Domains of Practice Gather and Analyze Patient Information Review history, physical information, medications, procedure request, and study protocol. Complete and verify documentation. Explain the procedure and orient the patient to the sleep center. Testing Preparation Procedures Prepare and calibrate equipment required for testing to determine proper functioning and make adjustments, if necessary. Apply electrodes and sensors according to accepted published standards. Perform appropriate physiologic calibrations to ensure proper signals and make adjustments, if necessary. Perform routine positive airway pressure (PAP) mask fitting. Polysomnographic Procedures Follow procedural protocols (such as Multiple Sleep Latency Test (MSLT), Maintenance of Wakefulness Test (MWT), parasomnia studies, PAP and oxygen titration, etc.) to ensure collection of appropriate data. Follow “lights out” procedures to establish and document baseline values (such as body position, oxyhemoglobin saturation, respiratory and heart rates, etc.) Perform polysomnographic data acquisition while monitoring study-tracing quality to ensure signals are artifact-free and make adjustments, if necessary. Document routine observations, including sleep stages and clinical events, changes in procedure, and other significant events in order to facilitate scoring and interpretation of polysomnographic results. Implement appropriate interventions (including actions necessary for patient safety and therapeutic intervention such as continuous and bi-level positive airway pressure, oxygen administration, etc.) Follow “lights on” procedures to verify integrity of collected data and complete the data collection process (e.g. repeats the physiological and instrument calibrations and instructs the patient on completing questionnaires, etc.) Demonstrate the knowledge and skills necessary to recognize and provide age specific care in the treatment, assessment, and education of neonatal, pediatric, adolescent, adult, and geriatric patients. Polysomnographic Record Scoring Assist with scoring sleep/wake stages by applying professionally accepted guidelines. Assist with scoring clinical events (such as respiratory events, cardiac events, limb movements, arousals, etc.) with center specific protocols. BACK TO TABLE OF CONTENTS 163 Polysomnographic Technician Assist with the generation of accurate reports by tabulating sleep/wake and clinical and event data. Service Management and Professional Issues Comply with applicable laws, regulations, guidelines and standards regarding safety and infection control issues. Perform routine equipment care and maintenance and inventory evaluation. Maintain current CPR or BCLS certification. Demonstrate effective written and spoken communication skills. Demonstrate appropriate social skills. Demonstrate ability to follow direction. Respond to study participant’s procedural-related inquiries by providing appropriate information. Education and/or Experience Successful completion of a polysomnography program, of no less than one year duration, associated with a state licensed and/or a nationally accredited educational facility. OR A minimum of 6 months of experience as a Polysomnographic Trainee with documented proficiency in all required competencies Physical Demands The physical demands described here are representative of those that must be met by an employee to successfully perform the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. While performing the duties of this job, the employee is frequently required to stand; use hands to finger, handle or feel; reach with hands and arms; climb or balance; and talk or hear. The employee must regularly lift and/or move up to 10 pounds, frequently lift and/or move up to 25 pounds, and occasionally lift and/or move up to 50 pounds. Specific vision abilities required by this job include close vision, distance vision, color vision, peripheral vision, depth perception, and ability to adjust focus. Work Environment The work environment characteristics described here are representative of those an employee encounters while performing the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. In the performance of this job, the employee may be exposed to chemical vapors such as acetone, ether, or glutaraldehyde. There may also be skin contact with these substances. The employee may also be exposed to infectious agents including blood-borne pathogens. BACK TO TABLE OF CONTENTS 164 Polysomnographic Technologist Position Summary A Polysomnographic Technologist works under the general supervision of the clinical director (M.D., D.O., or PhD) or designee to provide comprehensive evaluation and treatment of sleep disorders. This may involve polysomnography, diagnostic and therapeutic services or patient care and education. A Polysomographic Technician and may provide oversight of other staff. Domains of Practice Gather and Analyze Patient Information Collect, analyze, and integrate patient information in order to identify and meet the patient-specific needs (Physical/mental limitations, current emotional/physiological status regarding the testing procedure, pertinent medical/social history), and to determine final testing parameters/procedures in conjunction with the ordering physician or clinical director and laboratory protocols. Complete and verify documentation. Explain pre-testing, testing, and post-testing procedures to the patient. Testing Preparation Procedures Prepare and calibrate equipment required for testing to determine proper functioning and make adjustments if necessary. Apply electrodes and sensors according to accepted published standards. Perform appropriate physiologic calibrations to ensure proper signals and make adjustments if necessary. Perform positive airway pressure (PAP) mask fitting. Polysomnographic Procedures Follow procedural protocols (such as Multiple Sleep Latency Test (MSLT), Maintenance of Wakefulness test (MWT), parasomnia studies, PAP, oxygen titration, etc.) to ensure collection of appropriate data. Follow “lights out” procedures to establish and document baseline values (such as body position, oxyhemoglobin saturation, respiratory and heart rates, etc.) Perform Polysomnographic data acquisition while monitoring study-tracing quality to ensure signals are artifact-free and make adjustments, if necessary. Document routine observations including sleep stages and clinical events, changes in procedure, and significant events in order to facilitate scoring and interpretation of polyosomnographic results. Implement appropriate interventions (including actions necessary for patient safety and therapeutic intervention such as continuous and bi-level positive airway pressure, oxygen administration, etc.) Follow “lights on” procedures to verify integrity of collected data and complete the data collection process (repeats the physiological and instrument calibrations and instructs the patient on completing questionnaires, etc.) Demonstrate the knowledge and skills necessary to recognize and provide age specific care in the treatment, assessment, and education of neonatal, pediatric, adolescent, adult, and geriatric patients. Oversees and performs difficult and unusual procedures and therapeutic interventions. BACK TO TABLE OF CONTENTS 165 Polysomnographic Technologist Polysomnographic Record Scoring Score sleep/wake stages by applying professionally accepted guidelines. Score clinical events (such as respiratory events, cardiac events, limb movements, arousals, etc.) according to center specific protocols. Generate accurate reports by tabulating sleep/wake and clinical event data. Comply with applicable laws, regulations, guidelines and standards regarding safety and infection control issues. Perform routine and complex equipment care and maintenance. Evaluate sleep study related equipment and inventory. Maintain current CPR or BCLS certification. Demonstrate effective written and spoken communication skills. Demonstrate appropriate social skills. Respond to study participant’s procedural-related inquiries by providing appropriate information. Demonstrate the ability to analyze complex situations and apply policy. Comply with the BRPT Standards of Conduct. Education and/or Experience Successful completion of an accredited educational program leading to an associate degree with an emphasis in polysomnography. OR Successful completion of a polysomnography program of no less than one year duration associated with a state licensed and/or nationally accredited educational facility or equivalent experience and documented proficiency at all competencies required of a Polysomnographic Technician. OR Cerification by the Board of Registered Polysomographic Technologists as a Registered Polysomnographic Technologists or equivalent. Physical Demands The physical demands described here are representative of those that must be met by an employee to successfully perform the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. While performing the duties of this job, the employee is frequently required to stand; use hands to finger, handle or feel; reach with hands and arms; climb or balance; and talk or hear. The employee must regularly lift and/or move up to 10 pounds, frequently lift and/or move up to 25 pounds, and occasionally lift and/or move up to 50 pounds. Specific vision abilities required by this job include close vision, distance vision, color vision, peripheral vision, depth perception, and ability to adjust focus. BACK TO TABLE OF CONTENTS 166 Polysomnographic Technologist Work Environment The work environment characteristics described here are representative of those an employee encounters while performing the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions. In the performance of this job, the employee may be exposed to chemical vapors such as acetone, ether, or glutaraldehyde. There may also be skin contact with these substances. The employee may also be exposed to infectious agents including bloodborne pathogens. Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] BACK TO TABLE OF CONTENTS 167 Core Competencies CORE COMPETENCY: ARRIVAL PREPARATION AND ELECTRODE/SENSOR APPLICATION IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To document the knowledge and skills required in preparing the sleep disorders center for patient arrival and to describe the knowledge and skills required to apply electrodes and sensors to the patient for polysomnographic evaluation and to perform physiological calibrations. DEFINITION: Arrival preparations are those measures taken to set up the recording environment for a polysomnographic evaluation. Electrodes and sensor application is the process of attaching devices securely and comfortable to the patient for the measurement of multiple physiological parameters during the polysomnographic evaluation. Physiological calibrations is the process conducted pre and post testing where a series of instructions are given to the patient to elicit responses that are displayed on the polysomnogram and verify the signal integrity. SETTING: This guideline is confined to arrival preparations, application of electrodes and sensors, and physiologic calibrations for the polysomnographic evaluation. The polysomnographic evaluation must be performed in a facility-based sleep disorders center, and not in the home or in a mobile facility. INDICATIONS: Electrodes and sensors are applied to obtain physiologic data that are displayed and recorded during the polysomnographic evaluation. Proper application, placement and attachment are essential to insure signal integrity, minimize patient discomfort, and to reduce the need of disrupting the patient’s sleep due to interventions to maintain signal integrity. Physiological functions change during the sleeping state and many disorders are specifically induced by sleep, thus physiological calibrations establish comparative awake baseline data, and allow for adjustment of sensors and/or changes to sensitivity and filter settings to assure optimal display and signal integrity prior to lights out. CONTRAINDICATIONS: Contraindications to electrode and sensor application may include but are not limited to sensitivity or allergies to latex, tape, collodian conducting mediums and solutions used to clean and lower the skin impedances. Certain precautions need to be taken into consideration for patient’s with medical conditions. OUTCOME ASSESSMENT: Outcome is determined by assessment of electrode impedance and the quality of the polysomnographic recording at lights out. The following competency evaluation tool allows for an objective assessment of the performance level of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 168 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performanace of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Preparation for Patient Arrival Preparation and Application of Electrodes Correct Sensor use and Placement Patient Interaction Physiological Calibrations Monitoring During Calibration Patient Safety DEMONSTRATES KNOWLEDGE OF/SKILLS IN P OR NI COMMENTS *Preparing acquisition system to include pertinent data input. *Assuring room is prepared for patient use. *Assembling appropriate supplies for electrode/sensor application. *Selecting questionnaires and forms for completion by patient per facility protocol. *Utilizing the International 10/20 System of Electrode Placement. *Accurately measuring and marketing the placement position for each electrode. *Adjusting the electrode site to insure appropriate signal. *Using materials and techniques to assure optimal electrode site preparation while minimizing patient discomfort *Verifying appropriate impedance levels and correcting as indicated when impedance is high. *Applying pulse oximeter sensor allowing for patient comfort and accuracy of reading. *Familiarity with multiple types of sensors that monitor the following: Flow, chest and abdominal effort, snore level, (electrocardiogram, limb movement, oxygen saturation (SaO2) *Utilizing correct application method for each sensor. *Recognizing a distorted signal, improper sensor placement, improper impedence. *Reviewing pertinent information in patient chart including history and physical, sleep questionnaire and/or other collected information prior to and after patient arrival. *Greeting patient and introducing self by name. *Verifying patient i.d. prior to providing services by checking the patient i.d. band or other identifying method. *Explaining application of electrodes to patient during hook-up procedure. *Identifying impact of patient’s physical/mental status on the outcome of the procedure through observation and interview to verify background information and identify patient specific needs during testing (i.e. physical/mental limitations, current emotional and psychological status regarding the testing procedure, pertinent medical and social history. etc) *Analyzing and integrating collected information to perform appropriate sleep study, meet patient’s special requirements, and determine testing parameters/procedures. *Communicating appropriate information to patient in a respectful, ageappropriate manner. *Assisting patient as needed. *Explaining calibration procedure to patient. *Assuring proper function of audio/video system. *Giving parameter specific instructions and assessing signal response. *Documenting on recording each instruction given. *Making appropriate adjustments to sensors, sensitivity and filter settings to assure optimal signal quality. *Performing machine calibrations *Verifying accuracy of input signal during physiological calibration. *Making appropriate adjustments if calibration signal is accurate. Performing physiological calibration according to policy. *Recognizing the need to contact Medical Director or supervisor according to facility protocol. *Procedures for basic life support. *Facility specific emergency intervention protocol. ADOPTED BY THE ASSOCIATION OF POLYSOMNOGRAPHIC TECHNOLOGISTS (APT) ON OCTOBER 15, 2004. BACK TO TABLE OF CONTENTS 169 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] Core Competency: Capnography CORE COMPETENCY: CAPNOGRAPHY IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To describe the knowledge and skills required to use capnography in a sleep recording to define a quantifiable method for measurement of End Tidal CO2 (EtCO2) or Transcutaneous CO2 (TcCO2) during overnight polysomnogram. DEFINITION: EtCO2 assesses ventilation, by measuring carbon dioxide in the exhaled gas. TcCO2 assesses ventilation by measuring carbon dioxide through the skin. SETTING: This guideline is confined to the use of capnography in the sleep laboratory setting as a method of assessing airflow during polysomnographic evaluation. The polysomnographic evaluation must be performed in a facility-based sleep study laboratory, and not in the home or in a mobile facility. INDICATIONS: Capnography is useful in the assessment of apnea, hypoventilation, hypopnea and rebreathing of CO2. Primary indications are: 1.) Pediatric Polysomnography, 2.) Patients with history of lung disease, 3.) COPD patients with history of CO2 retention who require oxygen titration and/or non-invasive ventilation support, 4.) Patient’s with neuromuscular disorders affecting the respiratory muscles and 5.) Patients with tracheostomy. CONTRAINDICTIONS: None PRECAUTIONS: There is a potential for localized erythema or skin burns from the TcCO2 electrode at high heater temperatures. OUTCOME ASSESSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response. The following competency evaluation tool allows for an objective assessment of the performance of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 170 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performance of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing environment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE DEMONSTRATES KNOWLEDGE OF/SKILLS IN P OR NI COMMENTS COMPETENCY Equipment Specific *Assure proper function of EtCO2 / TcCO2 device. Operation / Calibration *Knowledge of operation EtCO2 / TcCO2 device. *Calibrate EtCO2 / TcCO2 device to polygraph and gas calibration as indicated by acquisition equipment as required. Nasal Cannula *Knowledge of how to fit appropriate nasal cannula for monitoring EtCO2 / TcCO2 allowing for patient comfort and compliance. *Adjust and proper fit. TcCO2 Electrode *Knowledge of appropriate sites for application of TcCO2 Application electrode. *Proper application and fixation of electrode. Patient Interaction *Explain EtCo2 / TcCO2 procedure t o patient during PreTesting Procedure. *Communication skills. Use of Equipment *Identify when to use EtCO2 /TcCO2 monitoring during NPSG. *Understands the basic theory of EtCO2 / TcCO2 monitoring. *State normal values for EtCO2 / TcCO2 and factors that can affect observed values. *Clinical reasoning. *Identify event characteristics (i.e., respiratory, cardiac, sleep stage, etc.) Documentation *Document and record changes in noted during NPSG on polygraph and technical note forms. *Identify, document and inform supervisor of equipment problems and EtCO2 / TcCO2 monitoring supply needs. Patient Safety *Identify when to contact Medical Director. *Identify when to change the TcCO2 site if using higher electrode temperatures. *Basic trouble shooting of device and possible solutions. Infection Control *Proper disposal of interface device. *Proper cleaning and disinfection of non-disposable items. Adopted by the Association of Polysomnographic Technologists June 3, 2003 BACK TO TABLE OF CONTENTS 171 Core Competencies CARE COMPETENCY: MAINTENANCE, CLEANING, AND SAFETY PRECAUTIONS IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To maintain a safe environment for patients and employees. To demonstrate knowledge of procedures for cleaning and maintaining equipment utilized during polysomnographic evaluations. To demonstrate knowledge of procedures to assure the electrical safety of devices employed in the sleep disorders facility. Equipment includes electrodes, sensors, acquisition equipment. Positive Airway Pressure (PAP) equipment, ancillary equipment, and beds used for recording the patient during the polysomnogram. DEFINITION: Maintenance refers to tasks performed at manufacturer recommended intervals top assure the proper functioning of a device. Cleaning is the process of washing soiled items, and may include use of disinfecting or sterilization procedures. Safety precautions are those steps taken to minimize the risk of harm from potentially hazardous materials or situations. SETTING: This guideline is confined to the cleaning and maintenance of equipment, sensors, electrodes and safety precautions. INDICATIONS: Maintenance of electrodes and sensors with proper application and removal techniques will provide for quality recordings and patient comfort. Equipment and safety precautions minimize risk to patients and employees. CONTRAINDICATIONS: No contraindications to cleaning and maintaining equipment, facility, reusable electrodes and sensors in the sleep disorders center are present. OUTCOME ASSESSMENT: Outcome is determined by assessment of the frequency of replacing reusable electrodes, sensors and equipment. The following competency evaluation tool allows for an objective assessment of the performance level of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 172 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performanace of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Maintenance of Reusable Electrodes and Sensors Cleaning Reusable Sensors and Electrodes Patient/Employee Safety Single Use Disposals Equipment Cleaning Prior to Patient Use Verification of Cleaning Prior to Patient Use Facility Cleaning and Maintenance DEMONSTRATES KNOWLEDGE OF/SKILLS IN *Properly applying electrodes and sensors. *Properly removing electrodes and sensors. *Proper storage techniques for electrodes and sensors. *Cleaning and disinfecting according to manufacturer’s Specifications, state and local health policies, and Occupational Safety and Health Administration guidelines *Seperating of clean and soiled sensors and electrodes. *Cleaning interface devices (e.g. CPAP mask), according to Manufacturers specifications. *Use of Universal Precautions. *Using proper hand washing techniques. *Awareness of latex sensitivity. *Appropriate use, disposal, and storage of hazardous mtrls. *Disposal of sharps, such as blunt tip needles. *Using Personal Protective equipment. *Procedures/equipment for disposal of contaminated items. *Identifying the need to contact appropriate personnel regarding issues to maintain facility for patient safety. *Chemical storage and use. *Obtaining and understanding Material Safety Data Sheets (MSDS) *Appropriate use of and proper disposal of single use disposable sensors and electrodes. *Familiarity with Occupational Safety and Health Administration (OSHA) requirements. *Implementing facility specific policy for identifying and reporting defective equipment *Maintaining log of equipment maintenance checks *Documenting replacement of equipment *Equipment-specific disinfection of sterilization techniques *Verifying electrodes or sensors have been properly cleaned According to department infection control, safety and hazardous material policies before being applied to the patient *Taking appropriate measures if it is determined electrodes or Sensors are not properly cleaned before attaching patient *Awareness of Occupational Safety and Health Administration (OSHA) requirements. *Maintaining a clean and safe workplace according to facility Policy. *Insuring that linens are changed daily for patient use. *Identifying and correcting any hazards or conditions which pose a risk to the safty of patients or staff P or NI COMMENTS ADOPTED BY THE ASSOCIATION OF POLYSOMNOGRAPHIC TECHNOLOGITS (APT) ON OCTOBER 15, 2004. BACK TO TABLE OF CONTENTS 173 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] Core Competency: Pulse Oximetry CORE COMPETENCY: MONOTORING PULSE OXIMETRY IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To describe the knowledge and skills required to analyze sleep recordings to define a quantifiable method for performance measurement of oxygen saturation during overnight polysomnogram. DEFINITION: Pulse oximetry is a well-established non-invasive method of monitoring the percentage of hemoglobin (Hb) which is saturated with oxygen. This is done with a sensor which is usually attached to the patient’s finger. SETTING: This guideline is confined to the use of monitoring pulse oximetry in the sleep laboratory setting to identify those respiratory events that meet the sleep laboratory protocol and implement appropriate therapeutic intervention. The polysomnographic evaluation must be performed in a facility –based sleep study laboratory, and not in the home or in a mobile facility. INDICATIONS: Oxygen saturation during polysomnography is used to identify associated respiratory related desaturations and helps determine the severity of the sleep apnea syndrome. CONTRAINDICATIONS: No contraindications to monitoring pulse oximetry in the sleep laboratory. OUTCOME ASSESSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response to therapy. The following competency evaluation tool allows for an objective assessment of the performance of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 174 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performanace of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Equipment Specific Operation / Calibration Pulse Oximeter Sensor Fit Patient Interaction Monitor Oximetry During PSG Documentation Patient Safety Infection Control DEMONSTRATES KNOWLEDGE OF/SKILLS IN *Knowledge of operation of pulse oximeter devices. *Calibrate pulse oximeter device to polygraph as indicated by acquisition equipment as required. *Knowledge of adjusting the sampling rate/trend settings on pulse oxmeter. *Knowledge of how to appropriately fit pulse oximeter sensor allowing for patient comfort and compliance. *Ability to recognize when improper sensor placement is affecting reading on polygraph. *Explain use of pulse oximetry to patient during pre-testing procedure. *Identify impact of patient’s physical/mental limitations on the outcome of the procedure. *Communication skills. *Verify accuracy of pulse oximetry readings during NREM and REM sleep. *Recognize when patient is experiencing desaturation with respiratory events. *Recognize when patient is experiencing low baseline saturation levels. *Identify artifact in pulse rate and/or oximetry readings *Identify corresponding event characteristics (i.e respiratory, cardiac, sleep stage, etc.) *Document and record oxygen saturation levels during NPSG on polygraph and technical note forms as indicated in laboratory protocol. *Identify, document and inform supervisor of equipment problems and sensor supply needs. *Identify when to contact Medical Director. *Identify when to use supplemental oxygen due to low saturations. *Proper cleaning of interface device. P or NI COMMENTS ADOPTED BY THE ASSOCIATION OF POLYSOMNOGRAPHIC TECHNOLOGISTS JUNE 3, 2003. BACK TO TABLE OF CONTENTS 175 Policy and Procedure Manual for Sleep Center of Kentuckiana Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] Core Competency: PAP CORE COMPETENCY: PAP Titration in Polysomnographic Technology OBJECTIVE: To describe the knowledge and skills required to analyze sleep recording to define a quantifiable method for performance measurement of titrating Positive Airway Pressure (PAP) during overnight polysomnogram. DEFINITION: Positive Airway Pressure is the delivery of positive air pressure through the nasal passage forming an air splint of the upper airway to provide continuous air exchange during sleep in patients with Obstructive Sleep Apnea/Hypopnea Syndrome. SETTING: This guideline is confined to the use of PAP in the sleep laboratory setting to implement appropriate therapeutic intervention to titrate PAP to eliminate or reduce the apnea/hypopnea index. The polysomnographic evaluation must be performed in a facility-based sleep study laboratory, and not in the home or in a mobile facility. (1) INDICATIONS: 1) AHI greater than 15, or (2) AHI greater than 5 and less than or equal to 14 with documented symptoms of excessive daytime sleepiness, impaired cognition, mood disorders or insomnia, or documented hypertension, ischemic heart disease or history of stroke. (1) The AHI is equal to the average number of episodes of apnea and hypopnea per hour and must be based on a minimum of 2 hours of sleep recorded by polysomnography using actual recorded hours of sleep (i.e. the AHI may not be extrapolated or projected or projected.) Two hours of recorded sleep in consistent with current practice. Apnea is defined as a cessation of airflow for at least 10 seconds. Hypopnea in the adult is defined as a cessation of airflow for at least 10 seconds with at least a 30% reduction in thorocoabdominal movement or airflow as compared to baseline, and with at least 4% oxygen desaturation. (1,2) (1) CMS guideline for Continuous Positive Airway Pressure (CPAP) Therapy Used in the Treatment of Obstructive Sleep Apnea (OSA) (#CAG-00093R) http://www.hefa.gov/coverage /8b3-bbb2.htm (2) “Hypopnea in Slee-Disordered Breathing in”, AASM Position Paper, SLEEP, vol. 24, No. 4, 2001 http://www.aasmnet.org/PDF/hyponeaposition.pdf CONTRAINDICATIONS: No absolute contraindications to PAP therapy in the sleep laboratory exist when the above indications are present. OUTCOME ASSESSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response to therapy. The following competency evaluation technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 176 ORIGINAL DATE: 09-01-2006 REVIEW DATE(s): 03-01-2007 APPROVAL(s): SIGNATURE: Policy and Procedure TITLE: Medical Emergency EFFECTIVE DATE: 09-01-2006 REVISION DATE(s):03-08-2011 TITLE: Medical Director Telephone: (859) 992-4660 TITLE: President Telephone: (502) 387-6133 SIGNATURE: Policy: As a medical facility SCK is going to be a target for incoming calls regarding medical issues, as long as this is going to be part of our goal serving the community SCK is planning to accommodate incoming calls as appropriate. Procedure: 1. Introduce the facility and your position. 2. Ask the patient what the call is regarding: A. Life threatening (unconscious, severe breathing problem, or sign of stroke / major trauma (not limited to extremities or small organ, ear, eye…) 1. Patient / Employee should dial 911 2. Start CPR protocol 3. Inform Medical Doctor Kheder Kutmah 1-859-992-4660 4. Contacting Norton Hospital emergency department with the Information about the condition. 1-502-629-8000 B. All other call: 1. List all patient information A. Name, age, sex B. Phone number C. Symptoms D. Preferred Pharmacy ( if available) E. Name of the Family Physician F. Date of Birth G. Explain to patient that you must consult with the doctor and either yourself or the doctor will return their phone call A.S.A.P. (give on-hold option if possible) 3.Give the doctors all information, in addition to old record if available. 4.Document the call and the response in patient chart or create one. BACK TO TABLE OF CONTENTS 177 Sleep Center of Kentuckiana Serving Community is our goal CONFIDENTIALITY OF PATIENT INFORMATION POLICY AND MEDICAL RECORDS: Information regarding the diagnosis, treatment and condition of patient is confidential and our employees are bound to keep all such information in confidence. 1. Discussion of confidential medical information is responsible only in the context of providing treatment and follow-up. 2. Discussion of confidential information with anyone other then appropriate medical personnel for any other purposes will subject the employee to disciplinary action up to and including termination. Discussion of patients is not heard in public areas. 3. Medical information requested regarding a patient treated in our offices might be disclosed for patient related purposes with the patient’s written authorization. Release of medical information to a primary care physician or a specialist physician is permitted with patient’s authorization. 4. Family members, attorneys or officers of the law will not get access to medical information or medical records without the patient’s written authorization or court ordered. 5. Employers (for our industrial accounts and workers compensation) may have medical record information concerning their employees if the reason is related to employment after patient authorization. 6. Identified agents of child welfare agencies may have access to medical records in cases of suspected child abuse. They must provide official identification prior to being given access to the records. 7. All employees will sign a confidentiality statement. This document will be kept in the employee’s personal file at their respective office. 8. Medical records kept in secure office (with sign at the door) without any access to public or patients, only employee authorization can have access to it. 9. Transporting, mailing, or faxing medical information will follow HIPAA regulations. 10. In care of Business Closure the Patient Medical records shall be transported and stored in a new secured location which is the Medical Director address 5107 Craig Creek Dr. Louisville, KY 40214. BACK TO TABLE OF CONTENTS 178 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performance of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Equipment Specific Operation/Calibration PAP Mask Fit Patient Interaction Adjust PAP During PSG Documentation Patient Safety Infection Control DEMONSTRATES KNOWLEDGE OF SKILLS/IN *Assure proper function of PAP device. *Knowledge of operation of PAP device and humidification devices. *Calibrate PAP device to polygraph as indicated by acquisition equipment as required. *Knowledge of use of auto-titrating PAP device. *Knowledge of how to fit appropriate mask for delivery of PAP allowing for patient comfort and compliance . *Adjust and fit proper headgear. *Explain PAP titrating procedure to patient during hook up preparation. *Identify impact of patient’s physical/mental limitations on the outcome of the procedure. *Communication skills. *Identify when to adjust PAP to achieve optimal therapeutic level, i.e. decrease snoring, respiratory events, desaturations and arousals. *Verify optimal pressure during supine and Stage REM sleep when applicable. *Recognize when patient is unable to tolerate PAP procedure. *Knowledgeable in possible side effects of PAP therapy. *Clinical reasoning. *Identify event characteristics (i.e., respiratory, cardiac, sleep stage, etc.) *Identify sleep fragmentation related to respiratory events and snoring. *Identify event characteristics demonstrating need to change to BiLevel PAP. *Identify when to use auto-titrating PAP device. *Document and record changes in PAP during NPSG on polygraph and technical note forms. *Describe reason for changes in PAP. *Identify, document and inform supervisor of equipment problems and PAP supply needs. *Identify when to contact Medical Director. *Identify when to discontinue PAP therapy due to patient intolerance. *Proper cleaning of interface device. *Proper maintenance of equipment. P OR NI Adopted by the Association of Polysomnographic Technologists June 3, 2003. BACK TO TABLE OF CONTENTS COMMENTS 179 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] Core Competencies CORE COMPETENCY: POLYSOMNOGRAPHIC MONTAGES AND EQUIPMENT CALIBRATION AND FUNCTION IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To describe the knowledge and skills required in assuring proper calibration of polysomnographic acquisition systems and ancillary equipment. To verify the knowledge and skills required in selecting the appropriate polysomnographic montage for monitoring physiological parameters necessary to assist in identifying various sleep/wake disorders and to provide for consistency in the recording and accuracy of data analysis. DEFINITION: Calibration is the process in which a known input standard is introduced into the acquisition system and the output to that standard is measured. The polysomnographic montage specifies the parameters recorded for data analysis and to assist in the indentification of sleep/wake disorders. SETTING: This guideline is confined to the process of equipment calibration and selection of polyosmnographic montages for data acquisition and equipment calibration in the sleep disorders center setting to insure appropriate diagnostic evaluation. The polysomnographic evaluation must be performed in a facility-based sleep disorders center, and not in the home or mobile facility. INDICATIONS: Acquisition systems and ancillary equipment must be calibrated pre and post testing to verify the integrity of the acquisition system. This helps to insure accuracy for determination of sleep stages, event recognition an din differentiating expected waveforms from artifact during the recording process. This selection of an appropriate recording montage is critical to insure that all relevant physiological parameters are included in the polysomnographic recording, and will vary according to the specific disorder being evaluated. CONTRAINDICATIONS: No absolute contraindications to equipment calibration and montage selection on the acquisition system in the sleep disorders center are present. OUTCOME ASSESSMENT: Outcome is determined by record review, adherence to sleep disorders center policy and to established guidelines. The following competency evaluation tool allows for an objective assessment of the performance level of the polysomnographic technologist, polysomnographic techniciam and polyosmnographic trainee. BACK TO TABLE OF CONTENTS 180 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performanace of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Equipment Specific Operation/Calibration Selection of Montage Demonstrate Appropriate Clinical Reasoning Skills Documentation DEMONSTRATES KNOWLEDGE OF/SKILLS IN *Calibrating acquisition per manufacturer’s recommendations to assure accurate functioning of equipment. *Verifying appropriate sensitivity, low frequency filter setting (high pass filter), high frequency filter setting (low pass filter) for each channel. *Determining appropriate utilization of alternating current (AC) and direct current (DC) amplifiers. *Knowledge of differential amplifiers (e.q. common mode rejection) *Interfacing ancillary equipment to acquisition system, calibrating and adjusting for optimal signal display. *Reviewing patient information including history and physical, provisional diagnosis and sleep questionnaire. *Identifying appropriate montages for evalution of a variety of sleep related disorders. *Utilization of montage according to center policy and physician order. *Recognizing the difference between acquisition and display montage. *Adjusting sensitivity and filter settings during acquisition for optimal display and signal integrity per facility policy. *Utilizing systematic troubleshooting procedures and methods to correct artifacts and maintain signal integrity. *Discriminating between patient or device induced artifact . *Identifying waveform and event characteristics to distinguish from artifact. *Recognizing the need for timely intervention to assure signal and data integrity. *Documenting pre-study and post-study montage settings. *Documenting changes made to the acquisition system (filters and sensitivity) during the polysomnogram. *Documenting the steps taken to correct artifact during the polysomnogram. P OR NI COMMENTS ADOPTED BY THE ASSOCIATION OF POLYSOMNOGRAPHIC TECHNOLOGISTS (APT) ON OCTOBER 15, 2004 BACK TO TABLE OF CONTENTS 181 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] CORE COMPETENCIES CORE COMPETENCY: SCORING SLEEP STAGES AND CLINICAL EVENTS IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To describe the knowledge and skills required to accurately score sleep stages and clinical events recorded during the polysomnographic evaluation. To describe the knowledge and skills necessary to generate a comprehensive and accurate report. DEFINITION: Scoring is the process of reviewing, analyzing, classifying and tabulating sleep staging and clinical events from the polysomnogram according to published professional standards and guidelines. Recordings are staged in 30 second epochs. Clinical eventc include, but not limited to, sleep related movements; arousals; cardiac arrhythmias; sleep disorder breathing; oxygen saturation level; Carbon Dioxide CO2) levels. SETTING: This guideline is confined to sleep state recognition, clinical event scoring and report generation. INDIACTIONS: This report is the single most important element of the nocturnal polysomnographic examination and the preparation should be thorough and systematic. Scoring according to professionally accepted guidelines is necessary because much of its diagnostic utility depends on the ability to correlate specific changes or abnormalities of one physiological parameter with specific conditions defined by another parameter or parameters. The generation of an accurate report is a significantly more powerful and complex tool than could be provided by individual and independent measurements of each variable. The methods and requirements for scoring each of the variables and their integration through the technical report are provided to the medical director with part of the information for making a diagnostic recommendation. The interpreting physician of the sleep disorders center must complete the clinical impression. CONTRAINDICATIONS: No contraindications in the sleep disorders center are present. OUTCOME ASSESSMENT: Outcome is determined by assessment of the inter-scorer reliability. The following competency evaluation tool allows for an objective assessment of the performance level of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 182 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] INSTRUCTIONS: The validator evaluates the employee in the performanace of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing evnvironment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCY Sleep Stage Scoring Clinical Event Scoring/Recognition Report Generation Inter-scorer Reliability DEMONSTRATES KNOWLEDGE OF/SKILLS IN *Professionally accepted guidelines for scoring sleep stage. *Utilizing scoring software to score sleep stage. *Recognizing sleep state, normal, and abnormal EEG waveforms. *Identifying artifact. *Recognizing the need for a manual review of all computerized scoring. *Professionally accepted guidelines for scoring clinical events. *Differentiating between normal and abnormal clinical events. *Identifying and scoring arousals according to accepted guidelines. *Ability to identify artifact. *Using scoring software to mark and label event type. *Identifying alpha intrusion. *Identifying hypersynchronous theta. *Identifying beta spindling. *Identifying asymmetrical activity. *Identifying seizure activity. *Identifying sleep disorder breathing and denote duration of apneic and hypopneic events according to accepted guidelines. *Cheyne-Stokes respiration *Obstructive sleep apnea *Central sleep apnea *Mixed Apnea *Obstructive hypopnea *Non event hypoxemia *Identifying oxygen desaturation levels. *Identifying CO2 levels. *Identifying and denote periodic limb movements of sleep according to accepted guidelines. *Identifying cardiac arrythmias, and recognizing their relationship to event or sleep stage. *Identifying bruxism. *Using analysis software for report generation. *Manually calculating data in report. *Insuring correct and complete patient information in report. *Providing printed samples of sleep stage and/or clinical events per facility protocol. *Reviewing final report for errors. *Maintaining correlation of 80% or greater with medical director and scoring technologists. P OR NI COMMENTS ADOPTED BY THE ASSOCIATION OF POLYSOMNOGRAPHIC TECHNOLOGISTS (APT) ON OCTOBER 15, 2004. BACK TO TABLE OF CONTENTS 183 Association of Polysomnographic Technologists One Westbrook Corporate Center · Suite 920 · Westchester, IL 60154 Phone 708-492-0796 · Fax 708-273-9344 · [email protected] CORE COMPETENCY: LOW FLOW OXYGEN CORE COMPETENCY: SUPPLEMENTAL LOW FLOW OXYGEN TITRATION IN POLYSOMNOGRAPHIC TECHNOLOGY OBJECTIVE: To describe the knowledge and skills required to analyze sleep recordings to define quantifiable method for measurement and titrating low flow supplemental oxygen during overnight polysomnogram. DEFINITION: Supplemental low flow oxygen therapy during polysomnography is the administration of oxygen at concentrations greater than room air to reduce or eliminate hypoxemia that occurs during sleep. Supplemental low flow oxygen therapy can be delivered either with a nasal cannula or entrained in the circuit during titration of Nasal Continuous or Bi-Level Positive Airway Pressure Titration. SETTING: This guideline is confined to the use of supplemental low flow oxygen in the sleep laboratory setting to implement appropriate therapeutic intervention to titrate supplemental oxygen to maintain oxygen saturation level per medical director’s protocol or direct order. The polysomnographic evaluation must be performed in a facility-based sleep disorders facility, and not in the home or mobile facility. INDICATIONS: Supplemental oxygen therapy should be instituted upon receipt of a physician order under specific circumstances: 1.) the patient is currently under treatment of a physician and supplemental oxygen therapy is prescribed; 2.) the patient is undergoing a polysomnographic study for titration of Nasal PAP therapy and is still experiencing desaturation, per facility protocol, after reaching optimal PAP level to eliminate respiratory events and arousals and no signs of CO2 retention are present; 3.) the patient is unable to tolerate Nasal PAP therapy and is experiencing significant desaturation with respiratory events. CONTRAINDICTATIONS: No absolute contraindications to oxygen therapy in the sleep disorders facility exist when the above indications are present. PRECAUTIONS and/or POSSIBLE COMPLICATIONS: In patients with chronic obstructive pulmonary disease, adding supplemental oxygen may lead to an increase in PaCO2 and a decrease in the drive to breathe which impairs the hypoxic drive. Fire hazard is increased with the use of oxygen in the sleep disorders facility. Power outage can lead to inability to use the oxygen concentrator and adequate back up should be in place. OUTCOME ASSESSMENT: Outcome is determined by clinical and physiologic assessment to establish adequacy of patient response to therapy. The following competency evaluation tool allows for an objective assessment of the performance of the polysomnographic technologist, polysomnographic technician and polysomnographic trainee. BACK TO TABLE OF CONTENTS 184 CORE COMPETENCY: SUPPLEMENTAL LOW FLOW OXYGEN TITRATION IN POLYSOMNOGRAPHIC TECHNOLOGY INSTRUCTIONS: The validator evaluates the employee in the performance of the competency, indicating either a pass (P) or need improvement (NI) for each critical performance event step. For each NI, a plan for correction is specified in the comments section. An employee cannot be passed on a competency if the safety/organization preparations have not been completed, such as patient identification, patient allergies (if appropriate), gathering supplies, preparing patient in advance for procedure, preparing environment for procedure, and adherence to hand washing/universal precautions/sterile technique where applicable. CORE COMPETENCIES Equipment Specific Operation/Calibration Oxygen Interface Fit Patient Interaction Adjust Supplemental Oxygen During PSG Documentation Patient Safety Infection Control DEMONSTRATES KNOWLEDGE OF/SKILLS IN *Assure proper function of oxygen concentrator or other methods of delivery. *Demonstrate how to increase oxygen flow using the regulator. *Review the patient’s history and physical when available to determine need for supplemental oxygen. *Assess patient’s need for supplemental oxygen using oximeter upon patient arrival to sleep disorders facility. *Assess patient’s need for supplemental oxygen using oximeter during the overnight polysomnographic evaluation. *Knowledge of how to fit and adjust nasal cannula for delivery of oxygen allowing for patient comfort and compliance. *Knowledge of how to entrain supplemental oxygen in PAP circuit at the mask, or according to facility protocol, with and without humidification devices. *Explain procedure to patient and method of delivery of supplemental oxygen as indicated. *Identify impact of patient’s physical/mental limitations on the outcome of the procedure. *Communication skills. *Identify when to adjust supplemental oxygen to achieve optimal saturation level according to facility protocol. *Recognize when patients requires supplemental oxygen according to facility protocol. *Knowledgeable in possible side effects of supplemental oxygen therapy. *Demonstrates clinical rationale. *Identify event characteristics (i.e., respiratory desaturations that do not respond to PAP therapy, cardiac, sleep stage, etc.) to change to supplemental oxygen level. *Identify signs that patient’s drive to breathe is becoming diminished. *Identify corrective actions that need to be implemented if patient’s drive to breathe is affected. *Verify optimal supplemental oxygen level during all sleep stages. *Document and record changes in oxygen during PSG on polygraph and technical note forms. *Identify, document, and inform supervisor of equipment problems and oxygen supply needs. *Identify when to contact Medical Director. *Identify when to begin supplemental oxygen therapy due to patient’s responsiveness to PAP therapy. *Recognize complications and contraindications for supplemental oxygen therapy. *Recognize complications and contraindications for supplemental oxygen therapy. *Identify routine maintenance of device filters. *Identify proper sequence of adding oxygen. *Proper disposal of single patient use nasal cannula. *Proper cleaning of interface device when entrained in PAP circuit. P OR NI BACK TO TABLE OF CONTENTS COMMENTS 185 POSSIBLE THIRD SHIFT STAFFING PATTERNS 1.0 Staffing patterns are to be established by time, night and number of beds. 2.0 Indicate shift overlap needs as warranted to provide for additional staffing as needed. 3.0 Possible third shift staffing patterns for alternative workweeks to cover staffing needs for polysomnographic evaluations. 3.1 Three twelve hour shifts (36 hours per week). 3.1.1 4.0 5.0 Employment regulations vary per state and need to be verified. 3.1.1.1 Overtime. 3.1.1.2 Lunch periods. 3.1.1.3 Breaks. Four ten hour shifts (40 hours per week). 4.1 Ten hour work shift agreement if required by state regulations. 4.2 Additional coverage to allow for adequate recording time as needed. Eight hour shifts (40 hours per week). 5.1 Additional coverage to allow for adequate recording time of polysomnogram as needed. BACK TO TABLE OF CONTENTS 186 SLEEP CENTER OF KENTUCKIANA EPWORTH SLEEPINESS SCALE NAME:__________________________________________________ In contrast to just feeling tired, how likely are you to doze off or fall asleep in the following situations. (This refers to your usual life in recent times, even if you have not done some of these recently; try to work out how they would have affected you.) Use the following scale to choose the most appropriate number for each situation. 0 = Would never doze 1 = Slight chance of dozing 2 = Moderate chance of dozing 3 = High chance of dozing SITUATION CHANCE OF DOZING Sitting and reading _____________________ Watching TV _____________________ Sitting inactive in a public place (i.e. a theater or meeting) _____________________ As a passenger in a car for an hour Without a break _____________________ Lying down to rest in the afternoon When circumstances permit _____________________ Sitting and talking to someone _____________________ Sitting quietly after lunch without alcohol _____________________ In a car, while stopping for a few minutes _____________________ TOTAL _____________________ (>8 are significant) BACK TO TABLE OF CONTENTS 187 SLEEP CENTER OF KENTUCKIANA MSLT Pre Sleep Questionnaire Patient:________________________________ ID#_________________________ Date:______________________ 1. Have you taken any medications in the last 24 hours? Yes____ No_____ If what?________________________________________________________ yes, 2. Have you felt ill today? Yes____ No_____ If yes, describe______________ __________________________________________________________________ 3. Did anything out of the ordinary happen recently to upset you? Yes__ No___ 4. What time did you eat your last meal?__________________________ am/pm Check the one that best applies How TIRED do you feel right now? How SLEEPY do you feel right now? How ALERT do you feel right now? Nap # 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 Not At All A Little Quite A Bit BACK TO TABLE OF CONTENTS Extremely 188 SLEEP CENTER OF KENTUCKIANA MSLT Post Sleep Questionnaire Patient:______________________________________ ID#____________________ Date:_________________________ 1. Compared to the way you felt before lying down, how do you feel now? ________ More Rested _________Less Rested ________Same 2. Did you experience any strange muscle sensations, sights or sounds? Yes______ No________ If yes, describe__________________________________ Check the one that best applies Nap# How TIRED do you feel right now? How SLEEPY do you feel right now? How ALERT do you feel right now? How did you sleep Not At All A Little Quite A Bit 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 YES Did you dream? 1 2 3 4 5 MWT Technical Procedure Documentation Form BACK TO TABLE OF CONTENTS NO Extremely 189 Patient Name:________________________________________ ID#_____________ Date:________________________ Time of Drug Screen:________________ Patient Position:_________________ Breakfast Served:___________________ Lunch Served:___________________ Document prior to each MWT test period the following observations Documentation MWT 1 MWT 2 MWT 3 MWT4 Room Lighting Lux Readings Window Lighting 7.5 Watt Night Light Temperature of Room Start Time Sleep Latency End Time “Did you sleep?” (Patient perception) Stanford Sleepiness Scale Rating Stanford Sleepiness Scale. Show the patient the Stanford Sleepiness Scale and ask them to rate the alertness level at start time and end time. Feeling active, vital, alert, wide awake Functioning at a high level but not at peak, able to concentrate Relaxed, awake but not fully alert, responsive A little foggy, let down. Foggy, beginning to lose track, difficulty in staying awake. Sleepy, prefer to lie down, woozy. Almost in reverie, cannot stay awake, sleep onset appears imminent. BACK TO TABLE OF CONTENTS 190 SLEEP CENTER OF KENTUCKIANA Phone: (502) 964-2440 Fax (866) 845-0491 Physician’s Order Sheet Patient_______________________________ Physician_____________________ Date of Study__________________________ Diagnosis_____________________ Please circle all that apply and indicate any conditions or deviations from Lab protocol, which also apply: Polysomnogram (95810 – TC) Polysomnogram with Continuous Positive Airway Pressure (96811 – TC) Other_______________________________________________________________ Indicate deviations from or additions to standard CPAP & Split study protocols: _______________________________________________________________ _______________________________________________________________ Multiple Sleep Latency Testing (MSLT – 95805), Please indicate below under the MSLT is to be performed. (Circle One) Regardless of previous night’s PSG study results If patient had RDI < 15 on previous night’s PSG study Only under the following conditions (i.e. no overnight PSG): _______________________________________________________________ Maintenance of Wakefulness Test (MWT – 95805) what conditions Ambien 10 mg P.O. if unable to fall asleep within 1 hour of “lights out”. Ambien 10 mg per center protocol Will patient need oxygen during their test? ____________ liters per minute CAUTION: PATIENT INSTRUCTED NOT TO TAKE FOLLOWING MEDICATION PRIOR TO SLEEP STUDY: _______________________________________________ CONFIRMATION:______________________________________________________ _____________________________ Physician Signature _____________________________ Date Include demographic information and history and physical. BACK TO TABLE OF CONTENTS 191 SLEEP CENTER OF KENTUCKIANA Standing Physician Order – Dispensing Medications POLICY: As ordered by the physician and compliant with local, state and federal regulations, a nurse (RN and LPN), Registered Polysomnographic Technologists (RPSGT) may dispense: Afrin Nasal Spray – 2 sprays in each nostril every 12 hours and PRN for stuffiness. Prescribed Nasal Spray – 2 sprays in each nostril every 12 hours and PRN, if Afrin nasal spray is not effective for nasal stuffiness and congestion. Ocean Nasal Spray – 2 sprays per nostril for nasal dryness and congestion during CPAP and BIPAP tritration. Tylenol 500 mg or Tylenol 325 mg tablets – 1-2 by mouth every 4 hours as needed for headache and pain. Tums or other antacid tabs or liquid (as directed) –as needed between meals and at bedtime for heartburn or upset stomach. Ambien 10 mg Tablet – 1 tablet by mouth if patient is unable to fall asleep within 1 hour of lights out. ______________________________ Attending Physician ______________________________ Director Sleep Disorders Center ______________________________ Attending Physician ________________________________ Medical Director Sleep Disorders Center BACK TO TABLE OF CONTENTS 192 FIRE / EVACUATION CHECKLIST AND REPONSIBILITIES FOR SLEEP TECHNOLOGISTS (Post in Patient Monitoring Area) CALL 911 ON CORDLESS PHONE. CHECK SLEEP ROOMS FOR PATIENTS / VISITORS ASSIST PATIENT / VISITORS OUT OF SLEEP ROOMS TO THE NEAREST EXIT. CLOSE DOORS TO ROOMS AFTER EXITING. TAKE FLASHLIGHT AND ASSIST PATIENTS TO NEAREST STAIRWELL ASSIST WHEELCHAIR-DEPENDANT PATIENTS / VISTORS TO MAIN ELEVATOR AREA AND . ONE STAFF MEMBER WILL REMAIN WITH PATIENTS UNTIL ASSISTANCE ARRIVES AFTER HELP ARRIVES, ASSIST WITH EVACUATION OF PATIENTS / VISITORS AS NEEDED USING NEAREST STAIRWELL GO OUT THE WEST SIDE ENTRANCE OF BUILDING DOWN STAIRS IF POSSIBLE. USE ALTERNATE ROUTE EAST SIDE OF BUILDING DOWN STAIR WAY. DESIGNATE AN AREA TO MEET FOR ROLL CHECK REMAIN IN AREA UNTIL “ALL CLEAR” IS GIVEN BY MANAGER/SENIOR TECHNOLOGIST OR EMERGENCY RESPONSE PERSONNEL. ***IN THE EVENT OF A BOMB THREAT, TAKE PURSES AND BAGS IF POSSIBLE. PROCEED WITH EVACUATION USING ELEVATOR UNLESS OTHERWISE NOTIFIED. BACK TO TABLE OF CONTENTS 193 Bed Partner Questionnaire PATIENT NAME:________________________________________________ Your relationship to patient:__________________________________________ How often have you observed this person’s sleep? ______Never ______Once or Twice ______Often _______Every Night Has this person fallen asleep during normal daytime activities or in dangerous situations? If yes explain:___________________________________________________________ What behaviors have you observed in this person while he or she was asleep? Check all that apply. Please describe the checked behaviors in more detail in the space at the end of the list. Include a description of the behavior, when it occurs during the night, frequency during the night, and how often it occurs (every night, 4 times a week, etc.) _____ Light Snoring _____ Loud Snoring _____ Awakening with Pain _____ Teeth Grinding _____ Leg or Arm Twitching _____ Sitting Up in Bed _____ Occasional Loud Snorts _____ Leg Kicking _____ Head Rocking/Banging _____ Choking _____ Shaking or Rocking _____ Sleepwalking _____ Pauses in Breathing _____ Becoming Very Rigid _____ Bedwetting _____ Limb Movement Every 10-20 Seconds _____ Doing an Unusual Activity _____ Other_____________________________________________________________ Explanation of Items Checked: ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________ BACK TO TABLE OF CONTENTS 194 Sleep Center of Kentuckiana Policies and Procedures Cancellation Protocol 1. 2. 3. 4. All efforts will be made by the scheduler to fill a sleep study opening when calls during the day to cancel the study. a. The scheduler will check those patients scheduled for a return sleep study for titration of CPAP to fill the vacated night. b. The scheduler will check for patients who indicated they would be able to move to an earlier date with little notice. c. The scheduler will check those patients scheduled farthest out from the vacated night to fill the vacated night. d. The scheduler will check with the remainder of patients to fill the vacated night. the patient The scheduler is unable to reach any patient to fill the vacated night by 5:00 pm, the scheduler will notify the night technicians of the status. a. The scheduler can give the night tech information pertaining to the search if there are still patients to contact then the night tech can continue the search. b. If no patient is found to fill the vacated night, the night techs will determine the priority for working that night. The night tech comes into work, checks the messages and finds that the patient has called and cancelled after working hours. a. The tech will make an effort to contact patients following the guidelines under item 1 to fill the vacated night. b. The tech will contact those patients living in close proximity to the sleep lab. The night tech is unable to find a patient to fill the vacated night by 9 pm, then efforts will be discontinued. The night techs will determine the priority for working that night. BACK TO TABLE OF CONTENTS 195 Policy and Procedure Manual for Sleep Center of Kentuckiana CPAP/BIPAP Titration Log form Patient Name:_________________________________________ Date:_____________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ TX _______cm from _____to_____ Estimated AHI______ Lowest SaO2____________ Changed because___________________________________________________ Comments:____________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________ BACK TO TABLE OF CONTENTS 196 Referral Form Please fill out the information below and fax it to (866) 845-0491. We will be in contact with your patient within 24 business hours. Today’s Date: ________________ Referring Physician Signature: _____________ PATIENT INFORMATION Patient’s Name: _________________________________________________ Patient’s Address: ______________________________________________ Home Phone: __________________________________________________ Alternate Phone: _______________________________________________ Patient’s DOB: ______________________ SS#: ______________________ Chief Complaint(s) of patient (check all that apply): Excessive Daytime Sleepiness Circadian Rhythm Disorder Snoring/Sleep Apnea Night Terrors Insomnia Sleep walking/talking/eating Possible Narcolepsy Restless Legs Syndrome Other (please specify ):_________________________________________ _________________________________________ INSURANCE INFORMATION You can either fill out the information below or fax a legible copy of the insurance card along with this form. Name of Insurance Company: ___________________________ Type: HMO PPO EPO POS Other: ___________ Primary Card Holder’s Name: ___________________________ Member ID number: ___________________________________ Customer Service #:____________________________________ BACK TO TABLE OF CONTENTS 197 PPH HY YSSIIC CIIA AN NO OR RD DEER RSS PATIENT NAME: ____________________________ DOB_____________________ PHYSICIAN: Dr. Kutmah PROBABLE OSAS DIAGNOSIS: INSOMNIA PLAN: NO STUDY WORK: NARCOLEPSY HYPOXIA Date of Sleep Study: ___________ PLMS HYPERSOMNIA NPSG Only CPAP/BIPAP Only Split (NPSG/CPAP) if RDI> _______ NPSG/MSLT/MWT LAB Dr. Draw Ferritin Thyroid Profile MWT Only CPAP________cm/MSLT OTHER_________________________________ Serum Fe HLA T4 TSH OTHER: __________________________________ PULMONARY: O2 DURING STUDY @__________________L/M OTHER: _______________________________________ MEDICATIONS: D/C DURING STUDY? (Please List)_______________________ _______________________________________________________________________ STANDING ORDERS: _____ TYLENOL EXTRA STRENGTH 1-2 TABS (500 MG ES) PO PRN _____ AMBIEN 10 MG @ BEDTIME PRN MAY NOT BE GIVEN AFTER 1:00AM _____AMBIEN 5 MG @ BEDTIME PRN PT >60YRS OLD MAY NOT BE GIVEN _____AFRIN NASAL SPRAY FOR “STUFFY” NOSE WITH CPAP OR BIPAP _____BREATHE EASY STRIPS PRN _____OXYGEN THERAPY @ 2L/M FOR SA O2<88% W/O APNEA/HYPOPNEA _____URINE OF UDS IF STAYING FOR MSLT/MWT _____SONATA 10 MG @ BEDTIME PRN MAY NOT BE GIVEN AFTER 1:00 AM BACK TO TABLE OF CONTENTS AFTER 12:00 Midnight 198 Technician Observation Form Study Date ____ / ____/ _____ Patient Name: __________________________ Patient Number: _____________________ DOB: ________ Ht:______ Wt:______ Study #: _____________ Acquisition #: ____________ Unit #: ___________ Room #:___________ Tech Name: _________________________ Ordering Physician: __________________________ Referring Physician: ________________________ Study Ordered: __________________ Medications: ______________________________________________________________________________________________________ _______ Were Unit Cals Performed ( )YES ( )NO Light Out:___________ Time Pos SaO2 Were Bio Cals Performed? ( ) YES ( )NO All Impedences below 10,000 at Lights Out? ( )YES ( )NO Lights On: __________ Resting SaO2:__________% Resting Heart Rate:__________ HR Stage Oxygen Snore Snore: 0 = None 1 = Mild 2 = Moderate 3 = Loud CPAP OH OA CA MA Comments Pos: S = Supine R = Right L = Left P = Prone BACK TO TABLE OF CONTENTS 199 Time Pos SaO2 HR Technician Observation Form ( Cont’d) PAGE 2 Stage Oxygen Snore CPAP OH OA CA MA Comments ______________________________________________________________________________________________________ ___________________________ AMBIEN: (Reminder: Pt. must be 18 or older. Do not give to patients staying for MSLT’s) (circle one) N/A or YES _________mgs. Taken at ___________ am/pm ( ) standing physician order at bedtime _________mgs. Takes at ___________ am/pm. ( ) patient failed to initiate sleep for 1 hour post lights out ______________________________________________________________________________________________________ ___________________________ CPAP SUMMARY: Starting CPAP/Bi-Level Pressure _________cm/H2O Ending CPAP/Bi-Level Pressure _________cm/H2O Optimal Level___________cm/H2O Mask Chosen By Patient:_______________________ Size:______________ Masks Shown:________________________________________________ ( ) Chin Strap Used ( ) Heated Humidifier Used ( ) Patient refused/intolerable and signed waver ______________________________________________________________________________________________________ ___________________________ OXYGEN ADMINISTRATION: Starting:_________LPM Ending ________LPM Baseline SaO2 w/o O2:_________% SaO2 at Final O2 Level: _________% ______________________________________________________________________________________________________ ___________________________ EKG Abnormalities observed: (circle one) Yes or No Type: ___________________ Scored By:________________________ Date:_________________ BACK TO TABLE OF CONTENTS 200 Pre-Sleep Questionnaire Name: _____________________________________ Has today been an unusual day in any respect? □ Yes □ No If yes, please explain: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ ______________ 1. 2. How much sleep did you have last night? 3. Did you take a nap today? If yes, how long did you nap? 4. Please indicate if you had alcohol, coffee, tea or soft drinks today. Specify approximate amounts and times: Type _________________ _________________ _________________ _________________ 5. □ Yes □ No ____________________ Minutes Amount _______ _______ _______ _______ Time ________ ________ ________ ________ List below any medications you took today (including prescription and over-the-counter): Medications _________________ _________________ _________________ _________________ 6. __________________ Hours Amount _______ _______ _______ _______ Do you have any physical complaints right now? Time ________ ________ ________ ________ □ Yes □ No If yes, please explain:________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ ___________________________ BACK TO TABLE OF CONTENTS 201 7. Pre-Sleep Questionnaire (continued) Check the one statement that best describes how you feel right now: □ Active and vital; alert; wide awake □ Functioning at high level, but not at peak; able to concentrate □ Relaxed; awake; not at full alertness; responsive □ A little foggy; not at peak; let down □ Foggy; beginning to lose interest in remaining awake □ Sleepy; prefer to be lying down; fighting sleep; woozy □ Almost in a trance; sleep onset soon; losing struggle to remain Awake. 8. Please indicate your desired bedtime tonight: _____________ 9. Please indicate at what time you wish to have the technician wake you in the morning The study you are undergoing is a medical procedure. To obtain the best, most informative data to aid the interpreting physician in diagnosing and treating any sleep disorder you may have, it may be necessary for the technician to allow you to sleep later than your specified wake-up time. 10. Please add any additional comments you might have: _____________________________________________________________ If you are now returning to the Sleep Disorders Center for a second study, please fill out the following section: 11. 12. Have you had any recent surgery or have you started taking any new medications (prescribed or over-the-counter) since your last sleep study? □ Yes □ No If yes, please describe: ______________________________________________________________________ ______________________________________ Have there been any changes in your quality of sleep or sleep patterns since your last sleep study? □ Yes □ No If yes, please describe: __________________________________________________________________________ 13. Has your weight changed in any way since your last sleep study? □ Yes □ No If yes, please describe: _____________________________________________________________________________________ ______________________ BACK TO TABLE OF CONTENTS 202 POST-SLEEP QUESTIONNAIRE Name: _______________________________________ 6/29/2017 10:11 PM 1. How long do you think it took you to fall asleep last night? ________________ 2. What is the total time you think you spent asleep? 3. How does this time compare to your usual time asleep? Longer ____ Same ____ Shorter ____ 4. How would you say your sleep last night compares with your typical night? Better _____ Same _____ Worse _____ 5. How many times do you remember waking up last night? 6. How long were you awake during the night? ________________ 7. Do you remember any dreams from last night? Yes No If yes, please briefly describe them: __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ 8. Did you get enough sleep? 9. Were you bothered by sleeping in our Sleep Center? Yes No If yes, please explain: ________________________________________________ ________________ ____________ Too little___ Just right___ Too much___ _______________________________________________________________________________ __________________________________________________________________ 10. Check the statement that best describes how you feel right now: □ Active and vital; alert; wide awake □ Functioning at a high level, but not at peak; able to concentrate □ Relaxed; awake; not at full alertness; responsive □ A little foggy; not at peak; let down □ Foggy; beginning to lose interest in remaining awake □ Sleepy; prefer to be lying down; fighting sleep; woozy □ Almost in a trance; sleep onset soon; losing struggle to remain awake 11. Please add any additional comments you might have: ______________________ BACK TO TABLE OF CONTENTS 203 MEDICATION ACKNOWLEDGEMENT FORM By signing this form, I acknowledge that I have received 5 mg/10mg of Ambien or 5 mg/10mg of Sonata, to aid with the onset of sleep during my NPSG (nocturnal polysomnography) and/or CPAP titration. __________________________________ Patient Signature __________________________________ Date __________________________________ Technician Signature BACK TO TABLE OF CONTENTS 204 NAME: _______________________________________________ NAP 1 NAP 2 NAP 3 NAP 4 NAP 5 6/29/2017 10:11 PM SSS TIME SLEEP LAT REM LAT Did You Subjective Duration Did You Sleep? Latency Dream? ____ ____ ____ ____ ____ _______ _______ _______ _______ _______ _____ _____ _____ _____ _____ ______Mins ______Mins ______Mins ______Mins ______Mins _____Mins _____Mins _____Mins _____Mins _____Mins _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ ________ ________ ________ ________ ________ AVERAGE SLEEP LATENCY __________Mins SLEEP LATENCY (MINS) 20 15 14 13 12 11 10 09 08 07 06 05 04 03 02 01 0 1 2 3 4 5 TECHNICIAN COMMENTS: ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ _____________________________________________________________________________________ BACK TO TABLE OF CONTENTS 205 MSLT INSTRUCTION SHEET 1. There will be five naps with the possibility of a fifth nap. 2. The first nap starts 2 hours after awakening and the other naps will be at two hour intervals (i.e. 9:00, 11:00, 1:00, 3:00, 5:00). 3. You have twenty minutes to fall asleep for each nap. If you do not fall asleep in this amount of time, the nap is over. If you do fall asleep within twenty minutes, then I will allow you to sleep for fifteen minutes and then awaken you. 4. At the beginning of each nap, I will ask you to lie in bed on you back such that you can go through some eye movements. These are similar to the ones you did last night (look up, look down, etc.). I will give you instructions for these over the intercom. After the eye movements are completed, I will tell you to get comfortable and try to fall asleep. At this time, you may turn to any position which is most comfortable for you to sleep. 5. You will only have on the electrodes that you do right now. We will not be adding any to these. I will replace any electrodes throughout the day as needed. 6. You must wear street clothes. 7. It is important for you to stay awake between naps, since we are trying to see how sleepy you are. If you feel yourself nodding off, get up and move around a little, 8. Lunch is served at approximately 11:30 am. 9. We have some refreshments here in the Center, so if you would like something to drink please let me know. 10. Do you have any questions? Someone will be in soon to answer any questions that You may have. BACK TO TABLE OF CONTENTS 206 Policy and Procedure TITLE: 24 hr Phone Access ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s)03-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURP OSE: To make sure patient care is available 24 hours POLICY: Answering machine available 24 hours to leave message and answering service phone number given on message PROCEDURE: Message able to be left if response needed next day. If a return call is needed the answering service is available at that time. BACK TO TABLE OF CONTENTS 207 Policy and Procedure TITLE: 24 hr on Call for Doctor ORIGINAL DATE: 09-01-2006 EFFECTIVE DATE: 09-01-2006 REVIEW DATE(s)03-01-2007, 3-08-2011 REVISION DATE(s):3-08-2011 APPROVAL(s): SIGNATURE: TITLE: Telephone: Medical Director (859) 992-4660 SIGNATURE: TITLE: President Telephone: (502) 387-6133 PURPOSE: To make sure patient care is available 24 hours from physician POLICY: Answering machine available 24 hours and answering service phone number given on message to contact physician. PROCEDURE: When a return call is needed a call from the physician may be requested from the answering service. BACK TO TABLE OF CONTENTS 208 Policy and Procedure Manual for Sleep Center of Kentuckiana POLICY AND PROCEDURE TITLE: INFECTION CONTROL PURPOSE: To insure the safety of sleep laboratory pr center staff and patients controlling the spread of infection. POLICY: Universal Precautions and Blood Borne Pathogen Standards will be followed when caring for patients. PROCEDURE: 1.0 Universal Precautions 1.1 Wash hands before and after contact with each patient during hookup, the polysomnographic evaluation, and removal of electrodes. 1.2 2.0 Gloves, when used, should be disposed of after contact with each patient. Infectious Conditions 2.1 Document infectious conditions. 2.1.1 2.1.2 procedure. 2.2 Needles used by patients for self-injections, i.e. insulin. Personal Protective Equipment (PPE) 4.1 5.0 Bag laundry according to facilities protocol. Sharps Container 3.1 4.0 Information obtained while talking with the patient during the hook up Laundry. 2.2.1 3.0 Review patient questionnaire and medical records. PPE is acquired by calling materials management. Single Use Supplies 5.1 Dispose of single use supplies, i.e. nasal cannulas, stick on electrodes, etc. after removed from patient. 6.0 Multiple Use Sensors and Supplies BACK TO TABLE OF CONTENTS 209 PAGE 2 TITLE: INFECTION CONTROL 6.1 Clean with an agent such as Control III or Sporiciden according to manufacturer recommendations. 6.2 Designate separate location for clean and dirty sensors and supplies. 7.0 Safety and Infection Control In-Service 7.1 New patient orientation/yearly thereafter. Records are kept by these mandatories by the Education Department. BACK TO TABLE OF CONTENTS 210 PAGE: 3 TITLE: ASSEMBLY, MAINTENANCE AND STORAGE OF CHARTS PURPOSE: A centralized chart is critical to follow the progress of the patient during evaluation in the sleep laboratory or center. POLICY: 1.0 A chart is assembled for each patient. Charts should be well organized, easily identified and readily accessible by the center staff. 2.0 The chart reflects the patient’s interactions in the sleep laboratory or center, including initial evaluation, testing (if any), diagnosis, treatment and follow-up. 3.0 Records pertaining to the patient will be treated as confidential, and the sleep laboratory or center has the obligation to safeguard the records against unauthorized disclosure. 3.1 Appropriate release will be filed in the chart when outside information is requested or if the sleep disorders records are sent out. PROCEDURE: 1.0 Chart Assembly 1.1 Identification Data 1.2 Insurance Information 1.3 Medical History will be provided by referring physician and/or self-report on initial questionnaire. 1.3.1 2.0 Medications 3.0 Physical Exam 3.1 4.0 5.0 The history should be sufficiently detailed to provide a qualified assessment for the physician or technologist responsible for testing. Information should include: 1.3.1.1 Chief Complaint 1.3.1.2 Sleep History 1.3.1.3 Details of Present Illness 1.3.1.4 Relevant past, social and family histories The physical examination should reflect a comprehensive inventory of body sytems. Diagnostic Orders 4.1 Appropriate authorizations from third party payers 4.2 Signed consents for procedures will be kept by Medical Records Department Reports BACK TO TABLE OF CONTENTS 211 Page: 3 TITLE: ASSEMBLY, MAINTENANCE AND STORAGE OF CHARTS 5.1 Sleep study reports are to be generated by the scoring technologist. 5.2 The interpreting physician correlates the report with the raw data and does an interpretation. The interpretation will include the diagnosis and treatment recommendations. The interpretation will be in the form of a dictated report. 6.0 Recording samples as necessary 7.0 Interpretation and treatment recommendations will be in the form of a dictated report 8.0 Progress Notes 8.1 All communication with patient or regarding the patient shall be noted, dated, and initialed on the progress note in black ink. 8.2 Communication should be documented at the time of contact. 9.0 Chart Maintenance 9.1 Clinical leader and staff will maintain current charts at designated location. 9.2 Clinical leader will resume responsibility for purging and/or archiving charts. 10.0 Chart Storage 10.1 Current charts will be stored at the sleep laboratory or center in securable file cabinets. 10.2 Charts that have been archived will be stored per Advocate Health Care Medical Records policy. BACK TO TABLE OF CONTENTS