* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download http://emedicine
HIV and pregnancy wikipedia , lookup
Maternal health wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Prenatal development wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
Prenatal testing wikipedia , lookup
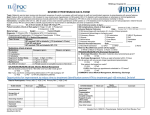
http://emedicine.medscape.com/article/1476919-overview Preeclampsia Author: Kee-Hak Lim, MD, Associate Professor, Department of Obstetrics and Gynecology, Harvard Medical School; Consulting Staff, Harvard Medical Faculty Physicians and Beth Israel Deaconess Medical Center Coauthor(s): Guy Steinberg, MD, MPH, MSc, Fellow in Maternal-Fetal Medicine, Beth Israel Deaconess Medical Center/Harvard Medical School Contributor Information and Disclosures Updated: Sep 4, 2008Print ThisEmail This Background Preeclampsia is a pregnancy-specific syndrome characterized by new-onset hypertension and proteinuria, occurring usually after 20 weeks' gestation. Although the etiology remains unknown, placental hypoperfusion and diffuse endothelial cell injury are considered be the central pathologic events. Preeclampsia is classified into mild and severe types and, in its extreme, may lead to liver and renal failure, disseminated intravascular coagulopathy, and central nervous system abnormalities, including seizures. Because the only cure is delivery, preeclampsia is associated with high maternal and neonatal mortality and morbidity. In the United States, preeclampsia is believed to be responsible for 15% of premature deliveries1 and 17.6% of maternal deaths.2, 3 Worldwide, preeclampsia and eclampsia are estimated to be responsible for approximately 14% of maternal deaths per year (50,000-75,000).4 Despite its impact on maternal and child health, efforts to predict and prevent the disease have been disappointing. Numerous strategies (low-dose aspirin, calcium, and vitamin C and E supplementation) have been shown to be of little benefit. Because our understanding of the pathogenesis of this disease is incomplete, these preventive strategies were proposed based on pathogenetic hypotheses that did not withstand the test of time. Recently, a number of investigators demonstrated and confirmed that an imbalance in angiogenic molecules play a major role in the pathogenesis of preeclampsia, raising the possibility that these molecules may be targeted for preventive measures and possible palliative therapy. See Medscape's Pregnancy and Hypertension Resource Centers. Pathophysiology The general consensus is that preeclampsia is an endothelial cell disorder resulting in mild-to-severe microangiopathy of target organs such as brain, liver, kidney, and placenta.5 While hypertension may be the most common presenting symptom, it should not be viewed as the initial pathogenetic process. Evidence of other organ involvement before hypertension becomes fulminant is not uncommon. Several circulating markers of endothelial cell injury have been shown to be elevated in women who develop preeclampsia before they became symptomatic. These include endothelin, cellular fibronectin, plasminogen activator inhibitor-1, and altered prostacyclin/thromboxane profile.6 Evidence to date suggests that oxidative stress; circulatory maladaptation; inflammation; and humoral, mineral, and metabolic abnormalities may all contribute to endothelial dysfunction and pathogenesis of preeclampsia. Many investigators believe that the placenta is the trigger for endothelial cell injury.7 Evidence suggests that hypoperfused placentas produce various factors that are capable of injuring endothelial cells. Recent data suggest that circulating factors that interfere with the action of vascular endothelial growth factor (VEGF) and placental growth factor (PlGF) play a major role in maternal manifestation of the disorder (see Angiogenic Factors in Preeclampsia). Placental hypoperfusion or ischemia in preeclampsia has many causes. Preexisting vascular disorders such as hypertension and connective tissue disorders can result in poor placental circulation. In cases of multiple gestation or increased placental mass, it is not surprising for the placenta to become underperfused. However, most women who develop preeclampsia are healthy and do not have underlying medical conditions. In this group of women, abnormally shallow placentation has been shown to be responsible for placental hypoperfusion. Placentation in Preeclampsia The shallow placentation noted in preeclampsia is a result of the inability of trophoblasts to invade the decidual vessels. In normal pregnancies, a subset of cytotrophoblasts called invasive cytotrophoblasts migrate through the implantation site and invade decidua tunica media of maternal spiral arteries and replace its endothelium in a process called pseudovascularization.8 As a result of these changes, these vessels undergo transformation from small muscular arterioles to large capacitance, low-resistance vessels. This allows increased blood flow to the maternal-fetal interface. Remodeling of these arterioles probably begins in the first trimester and ends by 18-20 weeks' gestation. However, the exact gestational age at which the invasion stops is unknown. In preeclampsia, this invasion of the decidual arterioles is incomplete. The invasive cytotrophoblasts fail to replace tunica media, resulting in mostly intact arterioles that are capable of vasoconstriction. Histologic evaluation of the placental bed demonstrates few cytotrophoblasts beyond the decidual layer. The trophoblast differentiation along the invasive pathway involves alteration in the expression of a number of different classes of molecules, including cytokines, adhesion molecules, extracellular matrix, metalloproteinases, and the class Ib major histocompatibility complex molecule, HLA-G.9, 10 For example, during normal differentiation, invading trophoblasts alter their adhesion molecule expression from those that are characteristic of epithelial cells (integrins alpha 6/beta 1, alpha V/beta 5, and E-cadherin) to those of endothelial cells (integrins alpha 1/beta 1, alpha V/beta 3, and VE-cadherin). The invasive cytotrophoblasts in preeclampsia fail to make this transition; they do not upregulate matrix metalloproteinase-9 (MMP-9) and HLA-G, 2 molecules noted in normally invading cytotrophoblasts. Primary cause for the failure of these invasive cytotrophoblasts to undergo pseudovascularization and invade maternal blood vessels is not clear. However, immunologic and genetic factors have been proposed. In addition, early hypoxic insult to differentiating cytotrophoblasts has been proposed as a contributing factor. However, these hypotheses need to be tested further. Systemic Endothelial Dysfunction Endothelium regulates vascular permeability, vassal tone, and coagulation cascade. While not all the factors produced by the placenta responsible for endothelial dysfunction have been characterized, recent data show that an imbalance of pro- and anti-angiogenic factors produced by the placenta may play a major role in mediating endothelial dysfunction. The circulating proangiogenic factors secreted by the placenta include VEGF and PlGF. The antiangiogenic factors include soluble fms-like tyrosine kinase I receptor (sFlt-1) (otherwise known as soluble VEGF receptor type I) and soluble endoglin (sEng). Other substances that have been proposed, but not proven, to contribute to this process include tumor necrosis factor, interleukins, various lipid molecules, and syncytial knots.11, 12 [#Angiogenic] Angiogenic Factors in Preeclampsia VEGF and PlGF Angiogenesis is critical for successful placentation. Both VEGF and PlGF promote angiogenesis by interacting with the VEGF receptor family. While both growth factors are produced by placenta, the serum level of PlGF rises much more significantly in pregnancy. Taylor et al demonstrated that the serum level of PlGF decreased in women who later developed preeclampsia.13 The fall in serum level was notable as early as the second trimester in women who developed preeclampsia and intrauterine growth restriction. In 2003, Maynard et al observed that the serum levels of both VEGF and PlGF were decreased in women with preeclampsia.14 However, the magnitude of decrease was less pronounced for VEGF since its serum level was not as high as PlGF, even in normal pregnancy. Others have confirmed this finding and showed that the serum level of PlGF decreased in women before they developed preeclampsia.15, 16 Soluble fms-like tyrosine kinase 1 receptor (sFlt-1) sFlt-1 is a soluble isoform of Flt-1, which is a transmembrane receptor for VEGF. While sFlt-1 lacks the transmembrane domain, it contains the ligand-binding region and is capable of binding circulating VEGF and PlGF, preventing these growth factors from binding to transmembrane receptors. Thus, sFlt-1 has an antiangiogenic effect. In addition to angiogenesis, VEGF and PlGF are important in maintaining endothelial homeostasis. Selective knockout of the glomerular VEGF gene has been shown to be lethal in rats, while the heterozygotes were born with glomerular endotheliosis (the renal lesion characteristic of preeclampsia) and eventually renal failure. Furthermore, sFlt-1, when injected into pregnant rats, produced hypertension and proteinuria along with glomerular endotheliosis.14 In addition to animal studies, multiple studies in humans have demonstrated that excess production of sFlt-1 is associated with an increased risk of preeclampsia. In a case-control study that measured levels of sFlt-1, VEGF, and PlGF, the investigators showed that the serum level of sFlt-1 increased earlier and higher in women who developed preeclampsia (21-24 wk) in comparison with women who did not develop preeclampsia (21-24 wk vs 33-36 wk), while the serum levels of VEGF and PlGF deceased. Furthermore, the serum level of sFlt-1 was higher in women who developed severe preeclampsia or early preeclampsia (<34 wk) than those in women who developed mild preeclampsia at term.15 Soluble endoglin (sEng) sEng is a soluble isoform of co-receptor for transforming growth factor beta (TGF-beta). Endoglin binds to TGF-beta in association with the TGF-beta receptor. Because the soluble isoform contains the TGFbeta binding domain, it can bind to circulating TGF-beta and decrease circulating levels. Since TGF-beta is a proangiogenic molecule, the net effect of high levels of sEng is anti-angiogenic. Several observations support the role of sEng in the pathogenesis of preeclampsia. It is found in the blood of women with preeclampsia up to 3 months prior to the clinical signs of preeclampsia, its level in maternal blood correlates with disease severity, and the levels of sEng in the blood drops after delivery.17 In studies on pregnant rats, administration of sEng results in vascular permeability and causes hypertension. It also has a synergistic relationship with sFlt-1, as it increases the effects of sFlt-1 in pregnant rats, resulting in HELLP syndrome, as evidenced by hepatic necrosis, hemolysis, and placental infarction.18 Moreover, sEng inhibits TGF-beta in endothelial cells and inhibits TGF-beta-1 activation of nitric oxide mediated vasodilatation. Epidemiology and Risk Factors The incidence of preeclampsia in the United States is estimated to range from 2-6% in healthy nulliparous women.19, 20, 21 In the developing world, the incidence is reported to be 4-18%.22, 23 The disease is mild in 75% of cases and severe in 25%.24 Of all cases of preeclampsia, 10% occur in pregnancies of less than 34 weeks' gestation. Eclampsia is estimated to occur in 1 in 200 cases of preeclampsia when magnesium prophylaxis in not administered.25, 26 The incidence is higher in women with a history of preeclampsia, multiple gestations, chronic hypertension, and underlying renal disease. (For related information, see Medscape's CME Activity Preeclampsia May Increase Risk for End-Stage Renal Disease.) In addition, obesity, diabetes, thrombophilia, and age older than 40 years are risk factors that put a woman at an increased risk of developing preeclampsia. Table 1 lists the risk factors and their odds ratio for preeclampsia.27 Some risk factors contribute to poor placentation while others contribute to increased placental mass and poor placental perfusion secondary to vascular abnormalities. Table 1. Risk factors for preeclampsia* Open table in new windowNulliparity 3:1 Age >40 y 3:1 African-American race 1.5:1 Family history 5:1 Chronic renal disease 20:1 Chronic hypertension 10:1 Antiphospholipid syndrome Diabetes mellitus 2:1 Twin gestation 4:1 High body mass index 3:1 Angiotensinogen gene T235 Homozygous 20:1 Heterozygous 4:1 10:1 *Adapted from ACOG Technical Bulletin 219, Washington, DC 199628 Classifications The National High Blood Pressure Education Program (NHBPEP) Working Group classifies hypertensive diseases in pregnancy into 4 groups: chronic hypertension, preeclampsia, preeclampsia superimposed on chronic hypertension, and gestational hypertension.29 The classification of hypertensive diseases in pregnancy according to the NHBPEP Working Group is as follows:29 Gestational hypertension BP of 140/90 mm Hg or greater for the first time during pregnancy No proteinuria BP returns to normal less than 12 weeks' postpartum Final diagnosis made only postpartum Chronic hypertension BP 140/90 mm Hg or greater before pregnancy or diagnosed before 20 weeks' gestation not attributable to gestational trophoblastic disease or Hypertension first diagnosed after 20 weeks' gestation and persistent after 12 weeks' postpartum. Preeclampsia/eclampsia BP of 140/90 mm Hg or greater after 20 weeks' gestation in a women with previously normal blood pressure and with proteinuria (>0.3 g protein in 24-h urine specimen). Eclampsia is defined as seizures that cannot be attributable to other causes in a woman with preeclampsia Superimposed preeclampsia (on chronic hypertension) New onset proteinuria (>300 mg/24 h) in a woman with hypertension but no proteinuria before 20 weeks' gestation A sudden increase in proteinuria or blood pressure, or platelet count less than 100,000 in women with hypertension and proteinuria before 20 weeks' gestation Mild preeclampsia is defined as the presence of hypertension (BP >140/90 mm Hg) on 2 occasions, at least 6 hours apart. Proteinuria is defined as the presence of greater than or equal to 1+ protein on random dipstick or at least 300 mg of protein in a 24-hour urine collection. Some investigators and clinicians have accepted a urine protein-creatinine ratio of at least 0.3 as a criterion for proteinuria, but the American College of Obstetricians and Gynecologists (ACOG) has not yet incorporated this in their definition.28 Edema and hyperreflexia are no longer considered to be diagnostic criteria. In addition, the relative rise of systolic pressure by 30 mm Hg and/or diastolic by 15 mm Hg has been dropped from the criteria for hypertension. Severe preeclampsia is defined as the presence of one of the following symptoms or signs in the presence of preeclampsia: Systolic BP of 160 mm Hg or higher or diastolic BP of 110 mm Hg or higher on 2 occasions at least 6 hours apart Proteinuria of more than 5 g in 24-hour period Pulmonary edema Oliguria (<400 mL in 24 h) Persistent headaches Epigastric pain and/or impaired liver function Thrombocytopenia Intrauterine growth restriction HELLP syndrome (hemolysis, elevated liver enzyme, low platelets) is a form of severe preeclampsia that has been associated with particularly high maternal and perinatal morbidity and mortality and may be present without hypertension or, in some occasions, without proteinuria. Diagnosis of Preeclampsia Preeclampsia is diagnosed when new-onset hypertension and proteinuria are present in a pregnant woman according to the criteria described in Classifications. However, because the clinical manifestation of preeclampsia can be heterogeneous, diagnosing preeclampsia may not be straightforward. In particular, since the final diagnosis of gestational hypertension can only be made in retrospect, a clinician may be forced to treat some women with gestational hypertension as if she has preeclampsia. In addition, if a woman has underlying renal or cardiovascular disease, the diagnosis of preeclampsia may not become clear until the disease becomes severe. Hypertension is diagnosed when 2 blood pressure readings of 140/90 mm Hg or greater are noted 6 hours apart within a one-week period. Measuring BP with an appropriate sized cuff placed on the right arm at the same level as the heart is important. The patient must be sitting and, ideally, have had a chance to rest for at least 10 minutes prior to the BP measurement. She should not be lying down in a lateral decubitus position, since the arm often used to measure the pressure in this position will be above the right atrium. The Korotkoff V sound should be used for the diastolic pressure. In cases where the Korotkoff V sound is not present, the Korotkoff IV sound may be used, but should be noted as such. The difference between the Korotkoff IV and V sound may be as much as 10 mm Hg. When using an automated cuff, it must be able to record the Korotkoff V sound. When serial readings are obtained during an observational period, the higher values should be used to make the diagnosis. To diagnose proteinuria, a 24-hour urine collection for protein and creatinine should be obtained whenever possible. Up to 30% of women with gestational hypertension who have trace protein noted on random urine samples may have 300 mg of protein in a 24-hour urine collection.30 Thus, 24-hour urine protein analysis remains the criterion standard. Alternatively, greater than 1+ protein on a dipstick analysis on a random sample is sufficient to make the diagnosis of proteinuria. Random urine samples can be used to calculate the protein-creatinine ratio. Thresholds of 0.14-0.3 have been proposed for diagnosing proteinuria.31 However, the best threshold for identifying pregnant women with significant proteinuria has not been agreed upon. Up to 10% of patients with preeclampsia and 20% of patients with eclampsia may not have proteinuria.32, 33 Furthermore, HELLP syndrome has been known to occur without hypertension or proteinuria. Because the underlying pathophysiology of preeclampsia is a diffuse endothelial cell disorder influencing multiple organs, hypertension does not need to necessarily precede other symptoms or laboratory abnormalities (see Pathophysiology). Presenting symptoms other than hypertension may include edema, visual disturbances, headache, and epigastric or right upper quadrant tenderness. All women who present with new-onset hypertension should have the following laboratory tests: complete blood count (CBC), serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, serum creatinine, and uric acid. In addition, a peripheral smear, serum lactate dehydrogenase (LDH) levels measured, and indirect bilirubin should be done if HELLP syndrome is suspected. While a coagulation profile (PT, aPTT, and fibrinogen) should also be evaluated, the clinical use of routine evaluation is unclear when the platelet count is 100,000 or more with no evidence of bleeding.34 While controversy exists over the threshold for elevated liver enzyme, the values proposed by Sibai et al (AST of >70 U/L and LDH of >600 U/L) appear to be the most widely accepted. Alternatively, values that are 3 standard deviations away from the mean for each laboratory value may be used for AST.35 The presence of schistocytes, burr cells, or echinocytes on peripheral smears, or elevated indirect bilirubin and low serum heptoglobin levels, may be used as evidence of hemolysis in diagnosing HELLP syndrome. The differential diagnosis for HELLP syndrome must include various causes for thrombocytopenia and liver failure such as acute fatty liver of pregnancy, hemolytic uremic syndrome, acute pancreatitis, fulminant hepatitis, systemic lupus erythematosus, cholecystitis, and thrombotic thrombocytopenic purpura. Other laboratory values suggestive of preeclampsia include elevation in hematocrit and a rise in serum creatinine and/or uric acid. While these laboratory abnormalities increase the suspicion for preeclampsia, none of these laboratory tests should be used to diagnose preeclampsia. Laboratory values for preeclampsia and HELLP syndrome 29, 35 Renal Proteinuria of >300 mg/24 h Urine dipstick >1+ Protein/creatinine ratio >0.3* Serum uric acid >5.6 mg/dL* Serum creatinine >1.2 mg/dL Low platelets/coagulopathy Platelet count <100,000/mm3 Elevated PT or aPTT* Decreased fibrinogen* Increased d-dimer* Hemolysis Abnormal peripheral smear* Indirect bilirubin >1.2 mg/dL* Lactate dehydrogenase >600 U/L* Elevated liver enzymes Serum AST >70 U/L8 Eclampsia, defined as new-onset tonic-clonic seizure in an otherwise healthy woman with hypertensive disorder of pregnancy, is a significant complication of preeclampsia and is associated with high maternal and neonatal morbidity and mortality. Multiple studies have described various abnormalities noted on CNS imaging studies. Both CT and MRI scans have revealed numerous abnormalities such as cerebral edema, focal infarction, intracranial hemorrhage, and posterior leukoencephalopathy.36 Unfortunately, at this time, there is no pathognomonic CT or MRI finding for eclampsia. Furthermore, cerebral imaging is not necessary for diagnosis and management. Cerebral imaging should be obtained in women with focal neurologic deficits, prolonged coma, or atypical presentation for eclampsia. Differential diagnosis for eclampsia includes cerebrovascular accidents, seizure disorders, brain tumors, metabolic diseases, metastatic gestational trophoblastic disease, and thrombotic thrombocytopenic purpura, among others. Management of Preeclampsia The optimal management of a woman with preeclampsia depends on gestational age and severity of the disease. Since delivery is the only cure for preeclampsia, clinicians must try to minimize maternal risk while maximizing fetal maturity. The primary objective is the safety of the mother and then the delivery of a healthy newborn. Preeclampsia A pregnancy complicated by mild preeclampsia at or beyond 37 weeks should be delivered. While the pregnancy outcome is similar in these women as those with a normotensive pregnancy, the risk of placental abruption and progression to severe disease is slightly increased.37, 38 Thus, regardless of cervical status, induction of labor should be recommended. Cesarean section may be performed based on standard obstetric criteria. Prior to 37 weeks, expectant management is appropriate. In most cases, patients should be hospitalized and monitored carefully for the development of worsening preeclampsia or complications of preeclampsia. While randomized trials in women with gestational hypertension and mild preeclampsia demonstrate the safety of outpatient management with frequent maternal and fetal evaluations, most of the patients in these studies had mild gestational hypertension.39 Therefore, the safety of managing a woman with mild preeclampsia as an outpatient still needs to be investigated. While bedrest has been recommended in women with preeclampsia, little evidence supports its benefit. In fact, prolonged bed rest during pregnancy increases the risk of thromboembolism. Antepartum testing is generally indicated during expectant management of these patients. However, the types of tests to be used and the frequency of testing have little consensus. Most clinicians offer a nonstress test (NST) and a biophysical profile (BPP) at the time of the diagnosis and usually twice per week until delivery.27, 28 If a patient is at 34 weeks' gestation or more and has ruptured membranes, abnormal fetal testing, progressive labor, or fetal growth restriction in the setting of mild preeclampsia, delivery is recommended. Severe preeclampsia When severe preeclampsia is diagnosed after 34 weeks' gestation, delivery is most appropriate. The mode of delivery should depend on severity of the disease and the likelihood of a successful induction. However, whenever possible, vaginal delivery should be attempted and cesarean section should be reserved for routine obstetric indications. In addition, women with severe preeclampsia who have nonreassuring fetal status, ruptured membranes, labor, or maternal distress should be delivered regardless of gestational age. If a woman with severe preeclampsia is at 32 weeks' gestation or more and has received a course of steroid, she should be delivered as well. Patients presenting with severe, unremitting headache, visual disturbance, and right upper quadrant tenderness in the presence of hypertension and/or proteinuria should be treated with utmost caution. Expectant management of severe preeclampsia If a patient presents with severe preeclampsia before 34 weeks' gestation, but appears stable and fetal condition is reassuring, expectant management may be considered provided they meet the strict criteria set by Sibai et al (see Laboratory values for preeclampsia and HELLP syndrome).40 This type of management should be considered only in a tertiary center. In addition, because delivery is always appropriate for the mother, some authorities consider delivery as the definitive treatment regardless of gestational age. However, delivery may not be optimal for a fetus that is extremely premature. Therefore, in a carefully chosen population, expectant management may benefit the fetus without greatly compromising maternal health. All of these patients must be evaluated on a Labor and Delivery unit for 24 hours before a decision for expectant management can be made. During this period, maternal and fetal evaluation must show that the fetus does not have severegrowthrestriction or fetal distress. In addition, maternal urine output must be adequate. The woman must have essentially normal laboratory values (with the exclusive exception of mildly elevated liver function test results less than 2 times the normal value) and hypertension that can be controlled. Fetal monitoring should include daily nonstress test and ultrasonography performed to monitor for the development of oligohydramnios and decreased fetal movement. In addition, fetal growth determination at 2-week intervals must be performed to document adequate fetal growth. In addition, a 24-hour urine collection for protein may be repeated. Corticosteroids for fetal lung maturity should be administered prior to 34 weeks. Daily blood tests should be performed for LFTs, CBC, uric acid, and LDH. Patients should be instructed to report any headache, visual changes, epigastric pain, or decreased fetal movement. Women with severe preeclampsia who are managed expectantly, must be delivered under the following circumstances: Nonreassuring fetal heart status Uncontrollable blood pressure Oligohydramnios with AFI of less than 5 cm Severe intrauterine growth restriction where estimated fetal weight is less than 5% Oliguria (<500 mL/24 h) Serum creatinine level of at least 1.5 mg/dL Pulmonary edema Shortness of breath or chest pain with pulse oximetry of <94% on room air Headache that is persistent and severe Right upper quadrant tenderness Development of HELLP syndrome Seizure prophylaxis Magnesium sulfate is the drug of choice for seizure prophylaxis in women with preeclampsia. Although the precise mechanism of its antiseizure activity is unknown, several randomized studies showed that magnesium sulfate is better than benzodiazepam or phenytoin in preventing the onset of initial eclamptic seizures and recurring seizures. Therapy is started at the beginning of labor or prior to cesarean section and continued 24 hours postpartum in most cases. The duration of postpartum therapy may be modified depending on the severity of the disease. Treatment is started by administering an intravenous (IV) loading dose of 4-6 g magnesium sulfate, followed by a maintenance dose of 1-3 g/h. Proposed mechanisms of action of magnesium sulfate therapy are prevention of calcium ion transport, cerebral blood vessel dilatation, and prevention of platelet aggregations (28 in up-to-date management of preeclampsia). Patients receiving magnesium sulfate should be monitored carefully for signs and symptoms of magnesium toxicity. Magnesium toxicity manifests initially as loss of patellar reflexes and shortness of breath. Therefore, the patellar reflexes must be checked every 4 hours and oxygen saturation and respiratory rate must be monitored. As magnesium sulfate is excreted by the kidney, urine output should be monitored closely and should be at least 30 mL/h. If magnesium toxicity is suspected, a blood test for magnesium level should be performed. Most practitioners feel comfortable with a level below 9.0 mg/dL. However, patients have been reported to show signs of toxicity below 6.0 mg/dL. Therefore, clinical evaluation of the patient should continue even if the serum magnesium level is below 9.0 mg/dL. Side effects of IV magnesium administration include flushing, chest heaviness, blurred vision, and minor headache. While these are not symptoms of toxicity, it may be reasonable to consider lowering the doseorwithholding therapy if they become severe. Rarely, magnesium can be administered intramuscularly (IM) if a patient does not have an IV access. The standard dose is to inject 5 grams IM in each buttock for a total of 10 g. The entire amount should not be injected in one site. If IV access is not established, a 5-g injection can be given every 4 hours until IV administration becomes possible. Magnesium sulfate therapy is contraindicated in patients with myasthenia gravis. Magnesium sulfate therapy for seizure prophylaxis should be administered to all women with severe preeclampsia during induction or labor. However, prophylaxis for mild preeclampsia is controversial. ACOG recommends magnesium sulfate in severe preeclampsia. However, ACOG has not recommended magnesium sulfate therapy in all cases of mild preeclampsia. Some practitioners withhold magnesium sulfate if blood pressure is stable and/or mildly elevated and if the laboratory values for liver function tests and platelets are mildly abnormal and/or stable. Others feel that even patients with gestational hypertension should receive magnesium, since a small percentage of these patients may either have or develop preeclampsia. The ultimate decision should depend on the comfort level of the labor and delivery staff in administering IV magnesium sulfate. An estimated 100 patients need to be treated with magnesium sulfate therapy to prevent one case of eclampsia.41, 42, 43 Acute treatment of severe hypertension in pregnancy Systolic blood pressure of 160 mm Hg or greater and/or diastolic pressure of 110 mm Hg or greater must be treated right away. The goal is to maintain the blood pressure around 140/90 mm Hg. Hydralazine is a direct peripheral arteriolar vasodilator and, in the past, was widely used as the first-line treatment for acute hypertension in pregnancy.44, 45 Hydralazine has a slow onset of action (10–20 min) and peaks approximately 20 minutes after administration. Hydralazine should be given as an IV bolus at a dose of 5–10 mg, depending on the severity of hypertension. It may be administered every 20 minutes up to a maximum dose of 30 mg. The side effects of hydralazine are headache, nausea, and vomiting. Importantly, hydralazine may result in maternal hypotension, which may subsequently result in a nonreassuring fetal heart rate tracing in the fetus.29 In a recent meta-analysis, Magee et al pointed out that hydralazine was associated with worse maternal andperinataloutcomes than labetalol and nifedipine. Furthermore, hydralazine was associated with more maternal side effects than labetalol and nifedipine.44 Labetalol is a selective alpha-blocker and nonselective beta-blocker that produces vasodilatation and results in a decrease in systemic vascular resistance. The dosage for labetalol is 20 mg IV with repeat doses (40, 80, 80, and 80 mg) every 10 minutes up to a maximum dose of 300 mg. Decreases in blood pressure are observed after 5 minutes (in contrast to the slower onset of action of hydralazine) and results in less overshoot hypertension than hydralazine. Labetalol decreases supraventricular rhythm and slows the heart rate, reducing myocardial oxygen consumption. No change in afterload is observed after treatment with labetalol. The side effects of labetalol are dizziness, nausea, and headaches. After achieving satisfactory control with IV administration, an oral maintenance dose can begin.29, 44 Calcium channel blockers act on arteriolar smooth muscle and induce vasodilatation by blocking calcium entry into the cells. Nifedipine is the oral calcium channel blocker that is used in the management of hypertension in pregnancy. The dosage of nifedipine is 10 mg PO every 15-30 minutes with a maximum of 3 doses. The side effects of calcium channel blockers include tachycardia, palpitations, and headaches. Concomitant use of calcium channel blockers and magnesium sulfate is to be avoided. Nifedipine is commonly used postpartum in patients with preeclampsia for blood pressure control.29, 44 In a severe hypertensive emergency, when above mentioned medications have failed to lower blood pressure, sodium nitroprusside may be given. Nitroprusside results in the release of nitric oxide, which subsequently results in significant vasodilation. Preload and afterload are then greatly decreased. The onset of action is rapid, and severe rebound hypertension may result. Cyanide poisoning may occur subsequent to its use in the fetus. Therefore, its use should be reserved for postpartum care or just before the delivery of the fetus.29 Eclampsia When eclamptic seizures occur, maternal injury must be prevented. The airway must be protected and oxygenation assured, including placement of a supportive airway, if necessary, to prevent aspiration. Management may include placement of a padded tongue blade and suctioning of the oral cavity. Pulse oximetry should be performed to monitor oxygenation and oxygen by facemask should be provided.36 Fetal monitoring may be instituted when the maternal airway and seizures are under control, since intervention for the fetus should not be considered until the mother’s condition is stabilized. Magnesium sulfate must be administered to prevent further seizure activity. A loading dose of 4-6 g followed by a maintenance dose of 2 g/h is given. Of women with eclampsia, 10% will have a second convulsion after receiving magnesium sulfate.36, 43 Occasionally, convulsions may recur even though a patient receives adequate doses of magnesium sulfate. In these patients, sodium amobarbital, 250 mg IV over 3–5 minutes, may be administered.36 Alternatively, benzodiazepine may be administered along with magnesium sulfate, since patients may have other underlying CNS causes for their seizure. Blood pressure must be controlled after initiation of magnesium sulfate therapy. This is accomplished by the administration of parental hydralazine and/or labetalol, as described previously. Hypoxemia, which may occur during maternal convulsive episodes, may lead to nonreassuring fetal heart rate status. Emergency cesarean section should be avoided until maternal status has been stabilized. Furthermore, most cases of nonreassuring fetal heart rate tracing will respond to in-utero resuscitation. Both maternal and fetal resuscitation can be performed concurrently. However, if bradycardia and/or recurrent late decelerations persist beyond 10–15 minutes despite all resuscitative efforts, and if the mother is stable, cesarean delivery may be considered. The utmost priority in managing eclampsia is maternal safety. Only when the mother is safe enough to undergo surgery may cesarean delivery be considered. If a cesarean delivery is not indicated, a vaginal delivery should be attempted. In terms of anesthesia for cesarean section or for pain control during labor, spinal and epidural anesthesia are contraindicated if the patient has severe thrombocytopenia (platelet count <50,000/mm3). If general anesthesia is necessary in case of an emergency cesarean or secondary to severe thrombocytopenia, a significant increase in blood pressure may be encountered during intubation, therefore elevating the risk of stroke. In this situation, blood pressure must be controlled in close collaboration with the anesthesiology team. Transfusion of blood products must be anticipated. Postpartum Management Preeclampsia resolves after delivery. However, patients may still have elevated blood pressure postpartum. Liver function tests and platelet counts must be performed to document decreasing values prior to hospital discharge. In addition, one third of seizures occur in the postpartum period, most within 24 hours of delivery, and almost all within 48 hours.46 Therefore, magnesium sulfate seizure prophylaxis is continued for 24 hours postpartum. Rarely, a patient may have elevated liver enzymes, thrombocytopenia, and renal insufficiency beyond 72 hours after delivery. In these cases, the possibility of hemolytic uremic syndrome (HUS) or thrombotic thrombocytopenic purpura (TTP) must be considered. In these situations, plasmapheresis along with corticosteroid therapy may be of some benefit and must be discussed with renal and hematology consultants. In addition, use of dexamethasone (10 mg IV q6-12h for 2 doses followed by 5 mg IV q6-12h for 2 doses) has been proposed in the postpartum period to restore platelet count to normal range in those with persistent thrombocytopenia.47, 48 The effectiveness of this therapy in preventing severe hemorrhage or ameliorating the disease course needs to be investigated further. Elevated blood pressure may be controlled with nifedipine or labetalol postpartum. If a patient is discharged with blood pressure medication, reassessment and a blood pressure check should be performed at the latest one week after discharge. Unless a woman has undiagnosed chronic hypertension, in most cases of preeclampsia, the blood pressure returns to baseline by 12 weeks' postpartum. Prevention and Prediction of Preeclampsia Efforts to prevent preeclampsia have been disappointing.49 To date, a systematic review of 14 trials using low-dose aspirin (60-150 mg/d) in women with risk factors for preeclampsia concluded that aspirin reduced the risk of preeclampsia (OR 0.86, 95% CI, 0.76-0.96) along with perinatal death, but did not significantly affect birth weight or the risk of abruption.50 Low-dose aspirin in unselected nulliparous women seems to reduce the incidence only slightly (RR 0.7, 95% CI 0.6-1.0).51 For women with risk factors for preeclampsia, starting low-dose aspirin (commonly, one tablet of baby aspirin per day), beginning at 12-14 weeks' gestation is reasonable. The safety of low-dose aspirin use in the second and third trimesters is well established.50, 52 The use of calcium and vitamin C and E supplementations in low-risk populations did not reduce the incidence of preeclampsia.53, 54, 55 Use of low molecular weight heparin in women with thrombophilia who have a history of adverse outcome has been investigated. However, to date, no data suggest that the use of heparin prophylaxis lowers the incidence of preeclampsia. Numerous screening tests for preeclampsia have been proposed over the past few decades. A screening test should be safe, valid, reliable, acceptable to the population, reproducible, appropriate for the population, and economical. Preeclampsia is an appropriate disease to screen, as it is common, important, and increases both maternal mortality and perinatal mortality. However, to date, no test has been shown to appropriately screen for preeclampsia.56 Although measurement of urinary kallikrein has been shown to have high predictive value, it was not reproducible.57, 58 While recent works on sFlt-1, PlGF, and VEGF are promising, their positive predictive values in predicting preeclampsia are yet to be evaluated in a prospective fashion. Currently, the clinical value of an accurate predictive test for preeclampsia is not clear since we lack effective prevention. Intensive monitoring in women who are at increased risk of developing preeclampsia, when identified by a predictive test, may lower the incidence of adverse outcome for both mother and the neonate. However, the effectiveness of such a strategy must be rigorously investigated. Recurrence In general, the recurrence risk of preeclampsia in a woman whose previous pregnancy was complicated by preeclampsia near term is approximately 10%.59 If a woman had severe preeclampsia (including HELLP syndrome and/or eclampsia), she has 20% risk of developing preeclampsia sometime in her subsequent pregnancy.60, 61, 62, 63, 64, 65 If a woman had HELLP syndrome or eclampsia, the recurrence risk of HELLP syndrome and eclampsia are 5%61 and 2%,63, 64, 65 respectively. The recurrence rate rises the earlier the disease manifested during the index pregnancy. If preeclampsia presents clinically before 30 weeks' gestation, the recurrence rate may be as high as 40%.66 Future cardiovascular disease Preeclampsia is a syndrome characterized by endothelial dysfunction in the mother. Therefore, the possibility exists that preeclampsia may be a contributor to future cardiovascular disease. In a recent metaanalysis, several associations were observed between an increased risk of cardiovascular disease and a pregnancy complicated by preeclampsia. These associations included an approximate fourfold increase in risk of subsequent development of hypertension and an approximate 2 times risk of ischemic heart disease, venous thromboembolism, and stroke.67 Moreover, women who had recurrent preeclampsia were more likely to suffer from hypertension later in life.67 In another review, Harskamp and Zeeman noted that population-based studies relate preeclampsia to an increased risk of later chronic hypertension (RR, 2.00-8.00) and cardiovascular morbidity/mortality (RR, 1.3-3.07), compared with normotensive pregnancy. Moreover, women who develop preeclampsia before 36 weeks' gestation or have multiple hypertensive pregnancies are at highest risk (RR, 3.4-8.12).68 Harskamp and Zeeman note that the underlying mechanism for the remote effects of preeclampsia is complex and probably multifactorial. The risk factors that are shared by cardiovascular disease and preeclampsia are endothelial dysfunction, obesity, hypertension, hyperglycemia, insulin resistance, and dyslipidemia. Metabolic syndrome, they note, may be a possible underlying mechanism common to cardiovascular disease and preeclampsia. Keywords preeclampsia, eclampsia, hypertension, proteinuria, placental hypoperfusion, diffuse endothelial cell injury, liver failure, renal failure, disseminated intravascular coagulopathy, seizures, chronic hypertension, preeclampsia superimposed on chronic hypertension, gestational hypertension, HELLP syndrome, thrombocytopenia, intrauterine growth restriction, Korotkoff sound, new-onset tonic-clonic seizure References Acknowledgments The authors and editors of eMedicine greatly acknowledge the contributions of previous authors MatthewWarden, MD and Brian Euerle, MD, FACEP to the development and writing of this article