* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Microbiology bio 123
Germ theory of disease wikipedia , lookup
Gastroenteritis wikipedia , lookup
Epidemiology of syphilis wikipedia , lookup
Globalization and disease wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Infection control wikipedia , lookup
Hepatitis C wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Herpes simplex wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Neonatal infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
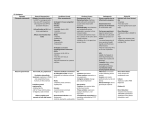
Module C-13 Urinary and Reproductive Tract Urinary: Structure: a. Kidneys b. Ureters (have smooth muscles in their wall, use peristalsis to move the urine) c. Bladder d. Urethra Normal Flora: a. The last 1/2 inch of the urethra is the only portion of the urinary structure to have normal flora. b. Urethra: 1. Lactobacilli 2. Staphylococci 3. Streptococci 4. Hemophilus Infections / inflammation 1. Cystitis - bladder infection 1. 2. 3. 4. 5. 6. 7. 8. Females have a 70-80% chance of having a bladder infection during their life time E. coli is the most common cause Most are biofilms Most often it is an endogenous infection Is typically called autoinoculation Males have a 50% chance of getting an infection Most common cause in males is from not washing hands Symptoms: 1. Frequent and painful urination 2. Blood or pus in the urine 9. If untreated, likely it will subside, but possible chance of infection of the kidneys causing pyelonephritis 10. Anyone that is catheterized will have a higher chance of a bladder infection (these are always biofilms) 1. Catheterization bacteria is normally Proteus (loves to move/swim) 2. Long term catheterization will typically caused by Pseudomonas 11. Treatments (generally rapidly cleared from body): 1. Tetracycline (broad spectrum – can cause yeast infections) 2. Ampicillin 3. Sulfonamide 2. Prostatitis a. Inflammation of the prostate gland b. c. d. e. f. Urethra passes though the prostate Usual cause is because urine is contaminated Increases chances of bladder infection 80% of the time, most common organism is E. coli, and is by autoinoculation Symptoms: 1. frequent and painful urination 2. Blood and pus in urine or semen g. Infections can be chronic h. Treatments include sulfonamide or trimethoprim sulfa 3. BPH a. b. c. d. e. f. Benign prostatic hypertrophy Non-infectious prostatitis Same symptoms as prostatitis Must be differentiated from prostate cancer Also need a PSA test (prostatic antigen test, needs to be less than 4) and digital exam Cancer can be treated with radiation and prostatectomy (removal of the prostate) Reproductive Tract: Male: a. b. c. d. Penis Testes Epididymis (sperm cells mature here) Vas deferens Female: e. Bladder f. Uterus g. Vagina h. Fallopian tube (uterine tube) i. Fimbriae j. Cervix Sexually Transmitted Diseases: Organisms tend to be very sensitive to cooling and drying Gonorrhea a. #2 STD b. Neisseria gonorrhea (Gram negative diplococcus [two] “the gonococcus” - typically kidney shaped. Most cocci are gram positive so this is rare.) c. Usually see them inside phagocytes d. Incubation a. 1-3 days after direct contact e. Male a. Presents as urethritis b. Painful urination c. Foul smelling pussy exudate d. Itching f. Female a. May be inflammation of the cervix and uterine tubes b. More than 80% of females are asymptomatic g. Untreated in females can lead to PID (Pelvic Inflammatory Disease) a. Effects the uterus, ovaries, and fallopian tubes b. Can develop scar tissue in the fallopian tubes, causing sterility h. Can also progress to gonococcal arthritis, gonococcal meningitis, or gonococcal endocarditis i. Treatments a. Penicillin - Worked until development of PPNG (penicillinase producing N. gonorrhea) in 1950’s b. Treated now with ceftriaxone c. Erythromycin for babies eyes (used to be silver nitrate) Syphilis a. b. c. d. e. Treponema palladium (spirochete) Very sensitive to drying and chilling. Cannot be grown in the lab. Must be grown in rabbit testes. Incubation period of 3 weeks There are three clinical stages (not everyone goes through all three) Primary syphilis: 1. Development of chancre (chancre is specific to syphilis) Can be anywhere. Very contagious. 2. Hard ridge around the edge, and is painless 3. Will reside without treatment 4. Chancre is contagious and can be found anywhere on the body where the organism made entry 5. About 6-8 wks later, begins secondary syphilis f. Secondary syphilis: 1. Organism has invaded bloodstream and moved through body 2. Headache, sore throat, aches/pains 3. Fever 4. Body rash that disappears without treatment; rash is very contagious. 5. Once rash disappears, enters latent phase and is not contagious. Can last up to 30 yrs. g. Latent phase – can last up to 30 years and never progress to tertiary stage. h. Tertiary syphilis: 1. Symptoms are not caused by the organism, but are caused by an immune (hypersensitivity) response. Can affect any tissue. 2. Caused by lesions called gumma - Can be found on skin, bone, and nervous tissue (external or internal) 3. Other symptoms are cardiovascular, erosion of the aorta, heart failure, blindness, paralysis, and dementia/insanity. - This dementia has been written about a lot in history i. Congenital syphilis: 1. After the sixteenth week of pregnancy, the organism can cross the placenta and be transferred to the fetus 2. The effect of the organism depends on what stage the mother is in. - If in primary or secondary syphilis, results in stillbirth - If in latent phase, the baby is often born with a latent syphilis infection and birth defects such as mental retardation and bone deformities. The bone deformities tend to smash in the nose, bow the legs, etc. May have other malformed organs, liver and kidney disease, and deafness. “Hutchinson’s Teeth” = notched teeth characteristic of hereditary syphilis. j. Treatments: 1. Penicillin - For primary, secondary, and congenital - Is not used for tertiary. Tertiary cannot be treated because it’s an immune response. - Treatments do not restore deformities in congenital syphilis 2. Before penicillin, small periods of arsenic were administered over long periods of time. 3. No vaccine. k. Testing for the organism is by antibodies (agglutinins) - The test is called Treponema Immobilization Test. When agglutinins are combined w/ treponema, treponema will become immobile. - Used to use the VDRL (Venereal Disease Research Laboratory Slide Test) Non-Gonococcal Urethritis and Vulvovaginitis Group of disorders that are not gonorrhea. Symptoms are inflamed urethra in men and inflamed vulva & vagina in women. 1. Chlamydia trachomatis a. Gram negative coccobacillus b. Is the most common STD, and is the most frequently reported STD c. Incubation period of 7-14 days d. Often co-infects with Gonorrhea e. Symptoms and very similar to Gonorrhea 1. Scant watery discharge in both male and female, most of the time in the morning 2. Sometimes painful urination in females but is often asymptomatic 3. Female may have abnormal vaginal bleeding 4. If untreated in female may result in pelvic inflammatory disorder and sterility 5. May cause contamination of the eyes of newborns – treated with erythromycin f. Treatments 1. Erythromycin 2. Tetracycline g. There are different strains of this organism 1. Some prefer the eyes – trachoma (eye infection with Chlamydia) h. About 600,000,000 people are thought to be infected, is thought to be the cause in half of the cases of blindness worldwide 2. Ureaplasma urealyticum a. Is also a gram negative coccobacillus b. Belongs to the Mycoplasma family (no cell walls, cold agglutinins) c. Responsible for half of all fertility that is caused by infection d. Causes low sperm count and decreases sperm motility e. Is a major cause of fetal death and recurrent miscarriages f. Treatment is with tetracycline – usually both partners are treated 3. Tricamonas vaginalis a. Is a flagellated protozoan – same family as Giardia b. Is the third most common cause of vaginal symptoms c. Can see the flagella very clearly on the protozoa d. Asymptomatic men and the carriers of these protozoa e. Symptoms 1. Itching and burning 2. Yellow frothy discharge (caused by the production of hydrogen gas by the protozoa) 3. Pain during urination 4. Walls of the vagina and vulva and red and swollen f. Is transmitted sexually, but can be transmitted by fomites if they are damp 1. Sharing towels, underwear, blankets g. Can be passed congenitally; babies can contract it during birth h. Treatments: 1. Flagyl 4. Candida albicans a. Candida b. Dimorphic fungus (yeast) c. Endogenous, opportunistic infection d. 2nd most common cause of vaginal symptoms e. Symptoms 1. Scanty white curd like discharge f. Cause is from disruption of normal flora 1. Typically the lack of Lactobacilli 2. Can occur with pH of vagina rises above 5 g. Late pregnancy may cause the fungus to propagate due to hormone shifts altering environment in vagina h. Taking oral contraceptive and diabetes may increase the chance of infection i. Treatment is with Nystatin (-azoles) and may give a suppository to lower pH or adjust hormone levels Viral STDs 1. Herpes simplex II a. b. c. d. e. f. g. h. i. j. k. l. m. Is a latent virus (causes intermittent symptoms) This is one of the family of Herpes viruses; inserts its own DNA into host’s nerve cells Genital herpes is the fourth or fifth most common STD Lesions start out as small red bumps that develop into blisters, which break which become ulcers. When they heal, they become dry and crusty. Typically found on vaginal, cervical, or urethral linings and on the shaft of the penis They disappear and then will recur sometimes later on They itch, burn and are painful Can be transmitted during inactive periods They can be transferred at birth, and a female with herpes will have an automatic C-Section at birth, even without symptoms If the infant does catch the herpes during birth, it will either die or be permanently be disabled Herpes patients have a 5x greater risk of cervical cancer Simplex I can cause simplex II and vice-versa Treatments include Acyclovir, an antiviral medication (doesn’t cure, only shortens symptoms) 2. Genital Warts a. Caused by Human Papilloma Virus (HPV) b. 12 viruses are transmitted – about 8 of them are associated with cervical cancer. Four of these are strongly associated and of those four, two are definitely known to be linked with cancer. c. Incubation of 1-3 months or longer d. May have no symptoms e. Warts may appear on head or shaft of penis, vulva, vagina, or anus, may block the urethra or vagina f. May be removed by freezing with liquid nitrogen or acid application g. May have complete remission, but does not mean that you are not infectious. Most times virus clears body but 10% of the time the virus inserts its DNA into host’s cells and becomes a persistent infection. h. Has a very high rate of cervical cancer i. Vaccine for HPV called Gardasil – contains top four viruses 3. HIV a. Is an example of a reverse transcriptase virus (retrovirus) b. Virus attacks helper T-cells and effects both B and T-cell immune responses c. Treated with AZT 4. Vaginosis a. Is an endogenous infection of the vagina (not STD) due to change in vaginal environment b. Usually due to a rise in vaginal pH and decrease in Lactobacilli c. Organism is typically Gardnerella vaginalis (gram negative bacillus) d. pH needs to be at about 5 or 6 (normal pH is about 4) e. Lactobacilli die off at about 5 pH f. Vaginal smear will reveal “clue” cells (epithelial cells that are covered in bacteria) g. Symptoms: 1. Frothy, fish smelling discharge diagnosed by “whiff test” h. Treatment is with Flagyl or recolonizing with a Lactobacilli Fetal infections 1. Cytomegalovirus a. CMV – causes cells to enlarge (recall square cube cell law – smaller cells are more efficient.) b. Belongs to the Herpes family c. About 75% of people have the virus d. Most of us have been exposed to the virus in childhood e. Problems are caused when you are exposed when very young infants, fetus and newborn f. Transmitted by body secretions (saliva, milk, urine, feces, vaginal secretions, mucus, semen, etc.) blood transfusions, vaginal birth g. Can cross the placenta h. About 10% of newborns show Congenital Cytomegalic Disease - can cause brain damage, hearing loss, impaired vision, jaundice (enlarged liver), anemia, and blindness i. Treatments – none 2. Toxoplasmosis a. Toxoplasma gondii b. Protozoan c. Can cross the placenta d. Rare meat and kitty litter e. Most harmful in the first trimester of pregnancy f. May cause severe birth defects – cardiac problems, blindness, mental retardation g. Treatments is with Flagyl h. Birth defects cannot be repaired with treatment.