* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download LECTURE OUTLINE DISEASE MECHANISMS OF GN Complement
Survey
Document related concepts
Transcript
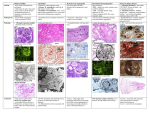
LECTURE OUTLINE DISEASE MECHANISMS OF GN Complement-leukocyte-mediated mechanism: 1. Complement activation 2. C5a (chemotactic) attracts neutrophils & monocytes 3. Damage caused by – Proteases – degrade GBM Oxidants – gen. cell damage Eicosanoids (arachidonic acid metabolite) C5b-9 (MAC) - epithelial cell detachment Platelets – aggregate in glom – prostaglandins Epith, mes. & endoth. Secrete interleukin-1 Circulating complexes vs. In situ complexes Pre-formed complexes – Post streptococcal Deposited antigens – Heymann’s Nephritis Glomerular antigens – Goodpasture’s syndrome Localisation of complexes Smallest molecules reach sub epithelial positions Larger molecules remain subendothelially or Migrate to the mesangial matrix Benign Hypertension NB renal disease ↔ hypertension a vicious circle Afferent arterioles Thickening, hyalinization of vessel wall Fibrin & BM matrix deposition Interlobular arteries Early = medial hypertrophy Later = fibrosis of media ≈ GLOMERULAR ISCHAEMIA = COAGULATIVE NECROSIS OF RENAL TUFT WITH LATER FIBROSIS & COMPLETE SCLEROSIS Macroscopy Small Granular surface with dark red depressed scars Microscopy Fibrous tissue infiltrated by lymphocytes & plasma cells Malignant Hypertension RAPID RISE IN BP FIBRINOID NECROSIS in afferent arterioles also Haemorrage Crescent formation Thrombosis Interlobular arteries Onion skin lesion of intima Medial hypertrophy Macroscopy “flea-bitten” kidney i.e. cortical haem. Smooth surface Occasional small infarcts CHRONIC RENAL FAILURE (CRF) All progressive renal diseases end in CRF - know all the diseases Severity = monitor [serum urea] [creatinine] GFR Surviving nephrons compensate – HYPERTROPHY INCREASED ACTIVITY (CONSTANT) Sclerosis – increased filtration pressure Efferent arteriole constriction Increased “wear & tear” on glom. EFFECTS OF CHRONIC RENAL FAILURE 1. Water & Electrolyte Balance – arrythmias & hypertesnion 2. Disturbance of acid-base balance – Metabolic acidosis 3. Uraemia – lethargy, anorexia, nausea, vomiting 4. Hormonal abnormalities – anaemia , renal osteodystrophy 5. Hypertension & its consequences – cardiac failure & stroke 6. Fibrinous exudates – heart, lung, colon 7. Haemorrhagic ulcers – in G.I.T 8. Immune depression – infections INFECTIONS OF THE KIDNEY Tubulointerstitial Nephritis (TIN) = group of inflammatory diseases that primarily involve the tubules & interstitium. Glom. Are spared or affected late TIN of bactrerial eatiology commonly has prominent involvement of renal pelvis hence the term PYELONIPHRITIS Pyelo- =pelvis Pyo- = pus production Interstitial nephritis (IN) is used to describe noninfectious cases e.g.: Drug damage to tubules Hypokalaemia (metabolic disorders) Irradiation Immune reactions Acute & Chronic categories are based on the clinical features & character of the inflammatory exudates reagardless of the etiology Ascending infection associated with lower UTI Or Haematogenous spread by pyogenic organisms (less common) Acute Pyelonephritis Clinical features: Pyrexia Nausea Vomiting Headaches Rigors Locally: Frequency Dysuria Loin pain Haematuria Macroscopy Streaks & wedges of suppuration in cortex Pale streaks with surrounding congestion in medullary rays Acute congestion & swelling of pelvis & parenchyma Microscopy Tubular destruction by abscess formation Mainly interstitial inflammation In tact tubules filled with pus cells Glom. In tact Urine Microscopy – pus cells / bacteria / red cells / pus cell casts Chemical – proteinuria / haematuria Bacteriology Principle causative org. = enteric gram neg. rods E.coli (most common) Proteus Klebsiella Enterobacter Pseudomonas Aetiology Women – cystitis / vesici-ureteric reflux during micturition / pregnancy / urethral instrumentation i.e. catheterisation & cystoscopy introduce bacteria into bladder Men – prostatic enlargement / urethral instrumentation i.e. catheterisation & cystoscopy introduce bacteria into bladder Both Sexes – calculi / tumours in renal pelvis / pressure effects of tumours on ureters / calculi in ureters & tumours of bladder Protective mechanisms: Antimicrobial action of bladder wall Flushing action during micturition Consequently urine is sterile IN outflow obstruction or bladder dysfunction: Defense protective mechanisms are overwhelmed Consequently stage is set for UTI Obstruction at level of urinary bladder = Incomplete emptying & increased residual vol. of urine= In the presence of stasis any bacteria introduced into the bladder for e.g. by catheterization can multiply undisturbed without being flushed or destroyed by bladder wall Incompetence of the vesicoureteral orifice allows bacteria to ascend the ureter into the pelvis i.e. VUR vesicoureteral reflux Intrarenal reflux = movement of urine from the renal pelvis through small ducts into the renal palillae and parenchyma Influence of urinary tract obstruction 1. stagnation of urine 2. vesico-ureteric reflux 3. catherterisationis carried out = mixed infection Progress Perinephric abscess Papillary necrosis – in kidney poles – associated with Obstruction Diabetes Analgesic nephropathy Sickle cell anaemia Severe hypotension Healing Recurrence CP CHRONIC PYELONEPHRITIS Due to REPEATED ATTACKS of INFLAMMATION & HEALING REFLUX CONGENITAL ANOMALIES Pathogenesis: Hypertension exacerbates pathology MACROSOPY MICROSCOPY 1. interstitial fibrosis 2. acute suppurative lesions (recent infection) 3. foci of dilatedw tubules in cortex – collecting tubules destroyed – upper tubules dilate – develop colloid casts – patchy atrophy & fibrosis CLINICAL EFFECTS LOSS OF RENAL CONCETRATING POWER ACIDOSIS URAEMIA (not in unilateral obstruction) HYPERTENSION NB Patient can still be passing large quantities of dilute urine CP CAUSES END STAGE RENAL FAILURE RENAL FUNCTION & PREGNANCY 1. 2. 3. 4. ACUTE PYELONEPHRITIS PRE-ECLAMPSIA & ECLAMPSIA ATN BILATERAL CORTICAL NECROSIS ACUTE TUBULAR NECROSIS AETIOLOGY Shock – haemorrhage / burns / trauma / acute intestinal / incompatible transfusion / acute pacnreatitis Poisoning – carbonCl4 / cis-platinum / lithium / mercury / antibiotics MACROSCOPY Cortex broad & pale Markings absent Enlarged Kidney Grossly congested pyramids Cut surfaces bulge due to oedema LIST OF TUBULO-INTERSTITIAL DISEASES 1. ATN 2. Pyelonephritis (infective aetiology) 3. IN (interstitial nephritis) Acute – 10-14 d post drug exposure Drugs = methicillin / NSAIDs (mefenamic acid) Symptoms = febrile / haematuria / prtoeinuria / arthralgia NB cause of ACUTE RENAL FAILURE Chronic – idiopathic / interstitial fibrosis is key feature / Inflammation with continual tubular damage with tubular loss and atrophy Many pnts present with CRF 4. Metabolic conditions e.g. gout / nephrocalcinosis / hypokalaemia Basic pathogenesis 5. Myeloma cast nephropathy 6. Renal Tubular Abnormalities AETIOLOGY OF HAEMOLYTIC URAEMIC SYNDROME 1. Children with E.coli 0157 alimentary infection (verocytotoxin) 2. Shock conditions e.g. abruptio placentae / endotoxic shock 3. Malignant hypertension 4. Drugs e.g. contraception / immunosuppressive drugs COMPLICATIONS OF END STAGE THERAPIES