Psychological Disorder
... (iii) Irrationality – unable to communicate in a reasonable manner with others. (iv) Unpredictability – acting in ways which are entirely unexpected. (v) Vividness and intensity– experience sensations which are far more vivid and intense than those of other people. (vi) Observer discomfort – acting ...
... (iii) Irrationality – unable to communicate in a reasonable manner with others. (iv) Unpredictability – acting in ways which are entirely unexpected. (v) Vividness and intensity– experience sensations which are far more vivid and intense than those of other people. (vi) Observer discomfort – acting ...
Spotting Trouble and Fixing it
... When it’s something – Symptoms in kids are the same as in adults: loss of appetite and energy, irritability, difficulty sleeping, feelings of worthlessness, inability to feel enjoyment. Thoughts of suicide are also a sign. Treatment – Cognitive therapy can help kids reframe feelings and change persp ...
... When it’s something – Symptoms in kids are the same as in adults: loss of appetite and energy, irritability, difficulty sleeping, feelings of worthlessness, inability to feel enjoyment. Thoughts of suicide are also a sign. Treatment – Cognitive therapy can help kids reframe feelings and change persp ...
Disorders Usually First Diagnosed in Infancy, Childhood
... Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence Mental Retardation; Learning Disorders Communication Disorders Autistic Spectrum Disorders Attention-Deficit and Disruptive Behavior Disorders Feeding and Eating Disorders of Infancy or Early Childhood Tic Disorders Other Disor ...
... Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence Mental Retardation; Learning Disorders Communication Disorders Autistic Spectrum Disorders Attention-Deficit and Disruptive Behavior Disorders Feeding and Eating Disorders of Infancy or Early Childhood Tic Disorders Other Disor ...
Obsessive Compulsive Disorder ( OCD )
... people with OCD often have abnormalities within the brain, particularly in the orbital cortex (the part of the brain above the eyes) Infection: • A streptococcal infection of the throat is known to occasionally result in the body confusing healthy cells with the infection and causing cellular damage ...
... people with OCD often have abnormalities within the brain, particularly in the orbital cortex (the part of the brain above the eyes) Infection: • A streptococcal infection of the throat is known to occasionally result in the body confusing healthy cells with the infection and causing cellular damage ...
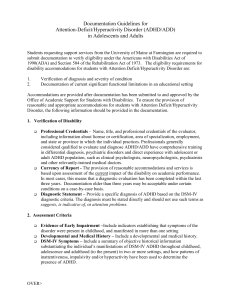
Word - University of Maine Farmington
... and state or province in which the individual practices. Professionals generally considered qualified to evaluate and diagnose ADHD/ADD have comprehensive training in differential diagnosis, psychiatric disorders and direct experience with adolescent or adult ADHD population, such as clinical psycho ...
... and state or province in which the individual practices. Professionals generally considered qualified to evaluate and diagnose ADHD/ADD have comprehensive training in differential diagnosis, psychiatric disorders and direct experience with adolescent or adult ADHD population, such as clinical psycho ...
TorontoRecovery08-JCullberg1
... • When you hear constant inner voices and know they don’t come ”from outside” - you don’t suffer from a psychosis but from a disorder of perception – a minor disturbance of the brain ...
... • When you hear constant inner voices and know they don’t come ”from outside” - you don’t suffer from a psychosis but from a disorder of perception – a minor disturbance of the brain ...
Step Up To: Psychology
... 5. Which of the following is not a misconception about psychological disorders that is dispelled by the chapter in your textbook? • A) “Crazy” behavior is very different than “normal” behavior • B) There is a strong social stigma attached to having a psychological disorder • C) Any behavior that is ...
... 5. Which of the following is not a misconception about psychological disorders that is dispelled by the chapter in your textbook? • A) “Crazy” behavior is very different than “normal” behavior • B) There is a strong social stigma attached to having a psychological disorder • C) Any behavior that is ...
PowerPoint Presentation - Psychological Disorders
... – parental communication that is disorganized, hard-to-follow, or highly emotional – expressed emotion • highly critical, over-enmeshed families ...
... – parental communication that is disorganized, hard-to-follow, or highly emotional – expressed emotion • highly critical, over-enmeshed families ...
Post-Traumatic Stress Disorders, Dissociative and Somatoform
... Alterations of function and structure of the amygdale and hippocampus associated with increased fear reactivity and intrusive memories following a traumatic event. Increased levels of general arousal such as a higher resting heart rate and increased levels of NEsuggest the sensitization of the symp ...
... Alterations of function and structure of the amygdale and hippocampus associated with increased fear reactivity and intrusive memories following a traumatic event. Increased levels of general arousal such as a higher resting heart rate and increased levels of NEsuggest the sensitization of the symp ...
Module 69 - Personality Disorders
... 1. Childhood maltreatment 2. A gene that altered neurotransmitter balance ...
... 1. Childhood maltreatment 2. A gene that altered neurotransmitter balance ...
When clinical psychosis accompanies depression
... associated psychotic symptoms, often mood-congruent delusions and hallucinations.1 Psychosis is defined as a loss of contact with reality, often exhibited by hallucinations, delusional beliefs, disorganised thinking or bizarre behaviour. Mood disorders can be accompanied by psychosis, including Schn ...
... associated psychotic symptoms, often mood-congruent delusions and hallucinations.1 Psychosis is defined as a loss of contact with reality, often exhibited by hallucinations, delusional beliefs, disorganised thinking or bizarre behaviour. Mood disorders can be accompanied by psychosis, including Schn ...
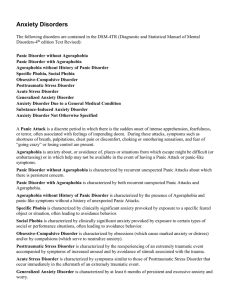
Anxiety Disorders - Joseph Berger MD, R. Ph.
... Agoraphobia without History of Panic Disorder is characterized by the presence of Agoraphobia and panic-like symptoms without a history of unexpected Panic Attacks. Specific Phobia is characterized by clinically significant anxiety provoked by exposure to a specific feared object or situation, often ...
... Agoraphobia without History of Panic Disorder is characterized by the presence of Agoraphobia and panic-like symptoms without a history of unexpected Panic Attacks. Specific Phobia is characterized by clinically significant anxiety provoked by exposure to a specific feared object or situation, often ...
Psychological Disorders
... Savanti repeatedly told her daughter that she was incompetent, and any mishaps that happened to her were her own fault.......When Mr. Savanti deserted the family, Angela’s first response was that somehow she was responsible. From her mother’s past behavior, Angela had learned to expect that in some ...
... Savanti repeatedly told her daughter that she was incompetent, and any mishaps that happened to her were her own fault.......When Mr. Savanti deserted the family, Angela’s first response was that somehow she was responsible. From her mother’s past behavior, Angela had learned to expect that in some ...
Disorder Patients - Journal of Rawalpindi Medical College
... Foundation Hospital, Rawalpindi a tertiary care facility. One hundred consecutive patients of both sexes, between ages of 13-60 years and diagnosed as dissociative (conversion) disorder from December 2009 to May 2010 were included in the study. The diagnosis ...
... Foundation Hospital, Rawalpindi a tertiary care facility. One hundred consecutive patients of both sexes, between ages of 13-60 years and diagnosed as dissociative (conversion) disorder from December 2009 to May 2010 were included in the study. The diagnosis ...
Unit Goal:
... • “Do not rush the person or crowd his personal space. Any attempt to force an issue may quickly backfire in the form of violence.” • “He may be waving his fists, or a knife, or yelling. If the situation is secure, and if no one can be accidentally harmed by the individual, you should adopt a *nonco ...
... • “Do not rush the person or crowd his personal space. Any attempt to force an issue may quickly backfire in the form of violence.” • “He may be waving his fists, or a knife, or yelling. If the situation is secure, and if no one can be accidentally harmed by the individual, you should adopt a *nonco ...
Document
... Premenstrual dysphoric disorder (PMDD) is: • a diagnosis used to indicate serious premenstrual distress with associated deterioration in functioning • a severely distressing and disabling condition that requires treatment. • characterized by depressed or labile mood, anxiety, irritability, anger, an ...
... Premenstrual dysphoric disorder (PMDD) is: • a diagnosis used to indicate serious premenstrual distress with associated deterioration in functioning • a severely distressing and disabling condition that requires treatment. • characterized by depressed or labile mood, anxiety, irritability, anger, an ...
PSY 150 Common Exam
... 46. According to Maslow, the psychological need that arises after all other needs have been met is the need for: a. unconditional positive regard. b. self-esteem. c. personal control. d.self-actualization. 47. Personality is defined as: a. the set of personal biases, stereotypes and prejudices b. th ...
... 46. According to Maslow, the psychological need that arises after all other needs have been met is the need for: a. unconditional positive regard. b. self-esteem. c. personal control. d.self-actualization. 47. Personality is defined as: a. the set of personal biases, stereotypes and prejudices b. th ...
12MoodDisorders
... expansive or irritable mood, lasting at least 1 week (or any duration if hospitalization is necessary) B. During the period of mood disturbance, 3 or more of the following symptoms have persisted (4 if mood is irritable) and have been present to a significant degree: 1) inflated self esteem or grand ...
... expansive or irritable mood, lasting at least 1 week (or any duration if hospitalization is necessary) B. During the period of mood disturbance, 3 or more of the following symptoms have persisted (4 if mood is irritable) and have been present to a significant degree: 1) inflated self esteem or grand ...
Dual Diagnoses
... (3) continuous treatment relationship in which (4) integrated treatment and (5) coordination of care can take place through multiple treatment episodes. Within this context, (6) case management / care and (7) empathic detachment / ...
... (3) continuous treatment relationship in which (4) integrated treatment and (5) coordination of care can take place through multiple treatment episodes. Within this context, (6) case management / care and (7) empathic detachment / ...
Dual Diagnoses - Integrated Recovery
... (3) continuous treatment relationship in which (4) integrated treatment and (5) coordination of care can take place through multiple treatment episodes. Within this context, (6) case management / care and (7) empathic detachment / ...
... (3) continuous treatment relationship in which (4) integrated treatment and (5) coordination of care can take place through multiple treatment episodes. Within this context, (6) case management / care and (7) empathic detachment / ...
studentship advert - University Of Worcester
... symptoms and signs. Despite these similarities the two disorders have very different aetiologies and prognoses (Paris & Black 2015). However, the two disorders are commonly diagnosed comorbidly. Estimates of the degree of comorbidity vary from as low as 4% (George et al. 2003) to as high as 50% (Wil ...
... symptoms and signs. Despite these similarities the two disorders have very different aetiologies and prognoses (Paris & Black 2015). However, the two disorders are commonly diagnosed comorbidly. Estimates of the degree of comorbidity vary from as low as 4% (George et al. 2003) to as high as 50% (Wil ...
Mental Illness_Care and Understanding of Schizoaffective Disorder
... schizoaffective disorder, and bipolar or other mood disorders (Frazier and Dryzmkowski, 2009). Not knowing what truly is behind a mental disorder can be frustrating but learning about an illness leads to a better understanding of what can be done to move forward. This disorder can make it difficult ...
... schizoaffective disorder, and bipolar or other mood disorders (Frazier and Dryzmkowski, 2009). Not knowing what truly is behind a mental disorder can be frustrating but learning about an illness leads to a better understanding of what can be done to move forward. This disorder can make it difficult ...
Anxiety Disorders - Austin Community College
... Anxiety is relieved by developing physical symptoms for which no known organic cause or physiologic mechanism can be identified Somatization Disorder Conversion Disorder Pain Disorder Hypochondriasis ...
... Anxiety is relieved by developing physical symptoms for which no known organic cause or physiologic mechanism can be identified Somatization Disorder Conversion Disorder Pain Disorder Hypochondriasis ...
Abnormal Psychology - West Morris Mendham High School
... – 4. Frequent negative thoughts, faulty attribution of blame, low self-esteem (cognitive) – 5. Loss of energy, restlessness (physical) – 6. May last six or more months • 12% of adult population will be affected by this • Can turn into a major depressive episode – Thoughts of suicide, death ...
... – 4. Frequent negative thoughts, faulty attribution of blame, low self-esteem (cognitive) – 5. Loss of energy, restlessness (physical) – 6. May last six or more months • 12% of adult population will be affected by this • Can turn into a major depressive episode – Thoughts of suicide, death ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.