Cardiomyopathy
... Heart muscle’s ability to act as a pump (the engine of the body) becomes poor >>>>>heart failure ...
... Heart muscle’s ability to act as a pump (the engine of the body) becomes poor >>>>>heart failure ...
Effects of Exercise on the Heart
... Reduction in resting heart rate as a result of training Below 60 beats per minute ...
... Reduction in resting heart rate as a result of training Below 60 beats per minute ...
Lecture Note 3 - Heart Failure
... blood or pump blood sufficiently through the body. • Thus, there will be inadequate supply of oxygen to peripheral tissues and organs. • Under perfusion of organs leads to reduced exercise capacity, fatigue, and shortness of breath. It can also lead to organ dysfunction (e.g., renal failure) in some ...
... blood or pump blood sufficiently through the body. • Thus, there will be inadequate supply of oxygen to peripheral tissues and organs. • Under perfusion of organs leads to reduced exercise capacity, fatigue, and shortness of breath. It can also lead to organ dysfunction (e.g., renal failure) in some ...
Congestive Heart Failure: From Basics to Recent Advances
... function and neurohormonal regulation, which are accompanied by effort intolerance, fluid retention, and reduced longevity” ...
... function and neurohormonal regulation, which are accompanied by effort intolerance, fluid retention, and reduced longevity” ...
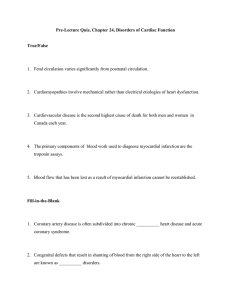
Pre-Lecture Quiz
... 3. Cardiovascular disease is the second highest cause of death for both men and women in Canada each year. ...
... 3. Cardiovascular disease is the second highest cause of death for both men and women in Canada each year. ...
Complications of Heart Disease Case Study Answers
... to a backup of blood into the pulmonary system. Clinical manifestations include dyspnea, cough, pulmonary crackles, low oxygen saturation, and, ultimately, decreased cardiac output. How do his medications treat his congestive heart failure? The Digoxin increases force of myocardial contractility and ...
... to a backup of blood into the pulmonary system. Clinical manifestations include dyspnea, cough, pulmonary crackles, low oxygen saturation, and, ultimately, decreased cardiac output. How do his medications treat his congestive heart failure? The Digoxin increases force of myocardial contractility and ...
ZLYHANIE SRDCA - TOP Recommended Websites
... the metabolizing tissue, or to do so only from an elevated filling pressure. • Clinical syndrome due to different structural and functional disease of the heart leading to abnormality in filling or emptying of the left ventricle. ...
... the metabolizing tissue, or to do so only from an elevated filling pressure. • Clinical syndrome due to different structural and functional disease of the heart leading to abnormality in filling or emptying of the left ventricle. ...
Atrial Fibrillation as A Complication of Congestive Heart Failure in
... Introduction Heart failure (HF) is a clinical syndrome that present when the heart is unable to pump blood forward at a sufficient rate to meet the metabolic demands of the body. HF results in a clinical syndrome of dyspnea, fatigue, peripheral edema and rales. In CHF patient often occurs ventricula ...
... Introduction Heart failure (HF) is a clinical syndrome that present when the heart is unable to pump blood forward at a sufficient rate to meet the metabolic demands of the body. HF results in a clinical syndrome of dyspnea, fatigue, peripheral edema and rales. In CHF patient often occurs ventricula ...
Slide ()
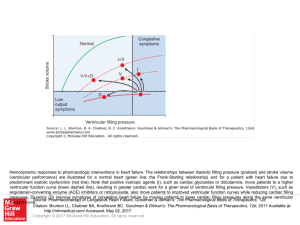
... Hemodynamic responses to pharmacologic interventions in heart failure. The relationships between diastolic filling pressure (preload) and stroke volume (ventricular performance) are illustrated for a normal heart (green line; the Frank-Starling relationship) and for a patient with heart failure due ...
... Hemodynamic responses to pharmacologic interventions in heart failure. The relationships between diastolic filling pressure (preload) and stroke volume (ventricular performance) are illustrated for a normal heart (green line; the Frank-Starling relationship) and for a patient with heart failure due ...
Pre-Lecture Quiz
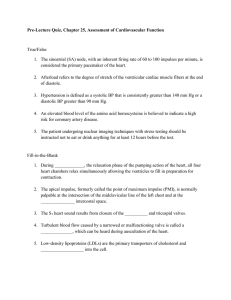
... considered the primary pacemaker of the heart. 2. Afterload refers to the degree of stretch of the ventricular cardiac muscle fibers at the end of diastole. 3. Hypertension is defined as a systolic BP that is consistently greater than 140 mm Hg or a diastolic BP greater than 90 mm Hg. 4. An elevated ...
... considered the primary pacemaker of the heart. 2. Afterload refers to the degree of stretch of the ventricular cardiac muscle fibers at the end of diastole. 3. Hypertension is defined as a systolic BP that is consistently greater than 140 mm Hg or a diastolic BP greater than 90 mm Hg. 4. An elevated ...
description
... Similar to paroxysmal nocturnal dyspnea, however this symptom occurs imminently when the patient lies down; measured by number of pillows the patient needs to breathe normally - symptom is assumed to be directly caused by the increasing amounts of fluid entering the lung during sleep and filling the ...
... Similar to paroxysmal nocturnal dyspnea, however this symptom occurs imminently when the patient lies down; measured by number of pillows the patient needs to breathe normally - symptom is assumed to be directly caused by the increasing amounts of fluid entering the lung during sleep and filling the ...
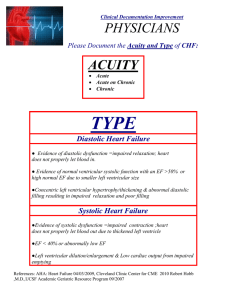
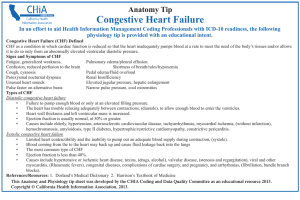
Congestive Heart Failure - California Health Information Association
... Causes include elderly, hypertension, arteriosclerotic cardiovascular disease, tachyarrhythmias, myocardial ischemia, (without infarction), hemochromatosis, amyloidosis, type II diabetes, hypertrophic/restrictive cardiomyopathy, constrictive pericarditis. Systolic congestive heart failure ...
... Causes include elderly, hypertension, arteriosclerotic cardiovascular disease, tachyarrhythmias, myocardial ischemia, (without infarction), hemochromatosis, amyloidosis, type II diabetes, hypertrophic/restrictive cardiomyopathy, constrictive pericarditis. Systolic congestive heart failure ...
Is Your Patient HuFfing and PuEFing? (HFPEF)
... Dr Matthew Best, Cardiologist, Perth Cardiovascular Institute ...
... Dr Matthew Best, Cardiologist, Perth Cardiovascular Institute ...
Pre-Lecture Quiz
... 1. The most common type of heart failure is an alteration in ventricular contraction called diastolic heart failure, which is characterized by a weakened heart muscle. 2. A decreased amount of blood is ejected from the ventricle in systolic heart failure. 3. Right-sided heart failure, failure of the ...
... 1. The most common type of heart failure is an alteration in ventricular contraction called diastolic heart failure, which is characterized by a weakened heart muscle. 2. A decreased amount of blood is ejected from the ventricle in systolic heart failure. 3. Right-sided heart failure, failure of the ...
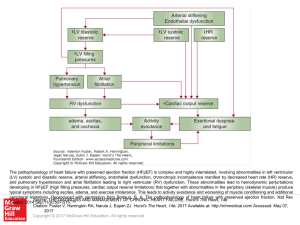
Slide 1 - AccessCardiology
... The pathophysiology of heart failure with preserved ejection fraction (HFpEF) is complex and highly interrelated, involving abnormalities in left ventricular (LV) systolic and diastolic reserve, arterial stiffening, endothelial dysfunction, chronotropic incompetence manifest by decreased heart rate ...
... The pathophysiology of heart failure with preserved ejection fraction (HFpEF) is complex and highly interrelated, involving abnormalities in left ventricular (LV) systolic and diastolic reserve, arterial stiffening, endothelial dysfunction, chronotropic incompetence manifest by decreased heart rate ...
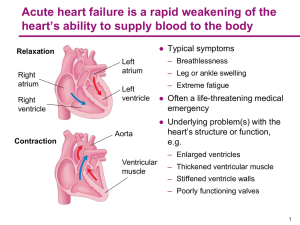
Heart failure

Heart failure (HF), often referred to as congestive heart failure (CHF), occurs when the heart is unable to pump sufficiently to maintain blood flow to meet the body's needs. The terms chronic heart failure (CHF) or congestive cardiac failure (CCF) are often used interchangeably with congestive heart failure. Signs and symptoms commonly include shortness of breath, excessive tiredness, and leg swelling. The shortness of breath is usually worse with exercise, while lying down, and may wake the person at night. A limited ability to exercise is also a common feature.Common causes of heart failure include coronary artery disease including a previous myocardial infarction (heart attack), high blood pressure, atrial fibrillation, valvular heart disease, excess alcohol use, infection, and cardiomyopathy of an unknown cause. These cause heart failure by changing either the structure or the functioning of the heart. There are two main types of heart failure: heart failure due to left ventricular dysfunction and heart failure with normal ejection fraction depending on if the ability of the left ventricle to contract is affected, or the heart's ability to relax. The severity of disease is usually graded by the degree of problems with exercise. Heart failure is not the same as myocardial infarction (in which part of the heart muscle dies) or cardiac arrest (in which blood flow stops altogether). Other diseases that may have symptoms similar to heart failure include obesity, kidney failure, liver problems, anemia and thyroid disease.The condition is diagnosed based on the history of the symptoms and a physical examination with confirmation by echocardiography. Blood tests, electrocardiography, and chest radiography may be useful to determine the underlying cause. Treatment depends on the severity and cause of the disease. In people with chronic stable mild heart failure, treatment commonly consists of lifestyle modifications such as stopping smoking, physical exercise, and dietary changes, as well as medications. In those with heart failure due to left ventricular dysfunction, angiotensin converting enzyme inhibitors or angiotensin receptor blockers along with beta blockers are recommended. For those with severe disease, aldosterone antagonists, or hydralazine plus a nitrate may be used. Diuretics are useful for preventing fluid retention. Sometimes, depending on the cause, an implanted device such as a pacemaker or an implantable cardiac defibrillator may be recommended. In some moderate or severe cases cardiac resynchronization therapy (CRT) may be suggested or cardiac contractility modulation may be of benefit. A ventricular assist device or occasionally a heart transplant may be recommended in those with severe disease despite all other measures.Heart failure is a common, costly, and potentially fatal condition. In developed countries, around 2% of adults have heart failure and in those over the age of 65, this increases to 6–10%. In the year after diagnosis the risk of death is about 35% after which it decreases to below 10% each year. This is similar to the risks with a number of types of cancer. In the United Kingdom the disease is the reason for 5% of emergency hospital admissions. Heart failure has been known since ancient times with the Ebers papyrus commenting on it around 1550 BCE.