* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gram-positive Spore Forming Bacilli
Survey
Document related concepts
Bacterial morphological plasticity wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neonatal infection wikipedia , lookup
Triclocarban wikipedia , lookup
Germ theory of disease wikipedia , lookup
Gastroenteritis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Infection control wikipedia , lookup
Sarcocystis wikipedia , lookup
Globalization and disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Transcript
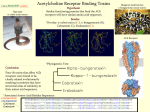
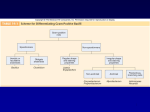
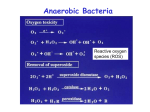
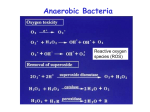
Gram-positive Spore Forming Bacilli. Divided into two groups according to their oxygen requirement. 1. Genus: Bacillus (aerobic). Two species. B.anthracis and B.cereus. 2. Genus: Clostridium. (anerobic). Four species. C.tetani, C.perfringens, C.botulinium and C.difficile. Bacillus anthracis Morphology & Characteristics. Gram-positive. Large Rectangular Bacilli (in chains). Central & Oval Spores. In older cultures not in clinical samples. Resistant to chemicals & heat. Killed by autoclave. Aerobic. Growth at 37°C. Non-motile. Large, waxy (dry) colonies, irregular shape, not haemolytic. On nutrient agar produce filamentous structures called “Medusa” head colonies. Capsualted in clinical animals & some laboratory media (conditions). Unique capsule of D-Glutamic acid. Require thymine and amino acids for growth. Ferment: Glucose, Sucrose, Maltose & Trehalose. Koch’s postulates first applied to B.anthracis. B.anthracis produces ZOONOTIC infection. Habitat: Soil or contaminated vegetative material. Antigens & Virulence Factors. Capsule. Important virulence factor. Inhibits phagocytosis. Found in clinical specimens but not always on laboratory media. Exotoxin. Protein complex. Composed of: 1. Protective antigen. 2. Oedema factors. 3. Lethal factors. • Increase vascular permeability & lead to shock. • Virulence dependent on presence of two Plasmids. One codes for the capsule & the other the toxin. Must be present in virulent strains. SporeForming/ mednotes/razina 1 Epidemiology Anthrax primarily disease of herbivores. Humans infections by contact with infected animals or contaminated animal products. Occurs in countries where animals are not vaccinated. Developed countries disease rare. Recent interest because of possible use as biological weapon. Human anthrax acquired by: 1. Inoculation. 2. Ingestion. 3. Inhalation. Clinical Infections. Cutaneous anthrax /Malignant pustule. Inoculation most common mode (manifestation). From contaminated soil or infected animal products (hides, goat hair & wool) Spores enter through the skin. Infections mainly on exposed areas of the skin. Initially painless papule at the site of scratch. Papule progresses to ulcer surrounded by vesicles & then to a necrotic “escar”. Necrosis due to effect of the toxin. Described as BLACK ESCAR. Clinical signs: lymphadenopathy & massive oedema. Mortality rate without treatment about 20%. Untreated the bacteria can invade regional lymph nodes & the blood stream this is usually lethal. Pulmonary anthrax. Woolsorter’s disease. Transmission by inhalation (uncommon mode nature). Most likely route for biological weapons. Patients may remain asymptomatic for prolonged period (2 months) different from other forms of disease. Spores transmitted from dust, wool fibers or brushes made from animal hair. Symptoms: Fever, dyspnoea, cough, headache, vomiting, chills, chest & abdominal pain. Bacteria multiply in bronchi then spread to lungs, lymphatics & blood stream. Produce intense inflamation, haemorrhage & septicemia as bacteria multiply. High mortality rate. (Requires very rapid treatment). SporeForming/ mednotes/razina 2 Gastrointestinal anthrax. Rare mode of transmission. Outbreaks follow ingestion of spores from contaminated meat. Clinical symptoms depend on site of infection. Invasion of upper intestinal tract results in formation of ulcers in mouth or oesophagus lead to regional lymphadenopathy, oedema & sepsis. Bacteria in the caecum or terminal ileum result in symptoms of nausea, vomiting and malaise which progress to systemic disease. Haemorrhagic diarrhoea and death. Mortality rate as high as 100%. Laboratory diagnosis. 1. Specimens: Skin or Fluid from vesicles, sputum, faeces or blood. 2. Microscopy: Gram-positive, large rectangular bacilli. Stains from cultures show long chains with spores. • Fluorescent Staining: Rapid detection. 3. Culture: Blood Agar shows large, waxy, irregular, grey colonies. Nutrient agar show “Medusa” head colonies. 4. Confirmatory Tests: Non-motile, Gelatin liquification. 5. Serological tests: ELISA. Retrospective value, NOT useful for rapid diagnosis. 6. Animal virulence tests: Used previously. 7. Toxin production tests: 8. PCR. Rapid detection. Treatment. 1. First choice: Ciprofloxacin. 2. Alternative drugs: Penicillin, Erythromycin, tetracyclines or chloramphenicol after suitable anti-microbial testing. Control & Prevention. 1. 2. Control in animals. Isolation & incineration of infected animals. Living attenuated vaccine (First vaccine by Pasteur). Live spore vaccine, new & effective. Control in humans. Prevent transmission from infected animals. Prevent transmission from infected cases by isolation of patients & use protective clothing. Chemoprophylaxis using ciprofloxacin for those at risk. Alum precipitated toxoid effective for at risk individuals. ****** SporeForming/ mednotes/razina 3 B.cereus : Food poisoning. Morphology & characteristics like B.anthracis. Differs, is motile & lacks glutamic acid capsule. Saprohyte: In vegetation, soil & water. Spores are heat resistant & most strains produce toxins. Associated with foods such as cereals and specially rice. Produces food-borne intoxication. Frequently associated with “Chinese food”. Clinical symptoms. 1. • • • • • • One organism produces two distinct diseases. Emetic Disease: Vomiting 1- 6 h after ingestion. Action of preformed toxin (intoxication). Low M.W. Stable to heat, acid & enzymatic activity. Associated with cereals & rice. Symptoms: Nausea, vomiting & abdominal cramps. Fever and diarrhoea usually absent. 2. • • • • Diarrhoeal Disease: Diarrhoea about 8-24 h after ingestion. Action of enterotoxins. Heat labile. Formed in intestine following ingestion. These toxins are similar to toxins produced by Salmonella and E.coli. Foods involved are; contaminated meat, vegetables and sauces. Symptoms: Diarrhoea, nausea and abdominal cramps. • • Laboratory Diagnosis. 1. Specimen: Food if available. Faeces not useful because colonisation common. Faecal isolation in cluster of cases may be useful. 2. Microscopy: Gram-positive bacilli with spores. 3. Culture: Blood agar. Show large numbers of organisms present per gram of food >108. SporeForming/ mednotes/razina 4 Treatment & control. Treatment. Self-limiting disease. Treatment - Fluid & electrolyte replacement. Antibiotics not required. Control. Disease prevented by proper cooling and storage of food. Ideally use fresh food. Adequate heating when using previously prepared foods. Characteristics of B.anthracis & “anthracoids” Characteristic B.anthracis Pathogen “Anthracoids” Non-Pathogenic Motile No Yes Haemolysis (Blood agar) No Yes Medusa head Yes No Capsule (Glutamic acid) Yes No Penicillin Sensitive Resistant Laboratory animals Virulent Not virulent ****** SporeForming/ mednotes/razina 5 Clostridium species. Characteristics. Large, Gram-positive, Straight or slightly curved with rounded ends. Pleomorphic. Produce spores. Anaerobic. Habitat; Soil & intestinal tract of humans & animals. Two types: 1. Saachrolytic species ferment carbohydrates to produce acid. 2. Proteolytic species metabolise proteins yielding foul smelling amines. Most species produce disease by action of enzymes & toxins (not invasive) but gas gangrene is invasive. Four important members to the group. C.tetani produces tetanus “lock jaw” syndrome. Drum stick appearance (terminal spores). Highly motile (peritrichious flagella). Spores enter through wound. Superficial abrasions, Puncture, Gunshots, burns or animal bite. Post-operative wounds & in babies umbilical stump infection “Tetanus neonatarum”. Not invasive disease. Remains in localised area of tissue. Require anaerobic environment to germinate and grow. Antigens: Many serotypes all produce same exotoxin. Immunity directed against exotoxin. Toxin producing strains have large plasmid. Loss of plasmid converts to a non-virulent strain. Pathogenesis. C.tetani produces tetanus “lock jaw” syndrome. Drum stick appearance (terminal spores). Highly motile (peritrichious flagella). Spores enter through wound. Superficial abrasions, Puncture, Gunshots, burns or animal bite. Post-operative wounds & in babies umbilical stump infection “Tetanus neonatarum”. Not invasive disease. Remains in localised area of tissue. Require anaerobic environment to germinate and grow. Antigens: Many serotypes all produce same exotoxin. Immunity directed against exotoxin. Toxin producing strains have large plasmid. Loss of plasmid converts to a non-virulent strain. SporeForming/ mednotes/razina 6 Virulence Factors. Two toxins: Tetanospasmin & Tetanolysin Tetanospasmin: 1. Binds to cells at neuromuscular junctions. 2. Crosses nerve cell membrane & is transported to inhibitory interneurons. 3. Blocks release of inhibitory transmitters (e.g.γ-amino-butyric acid GABA, glycine) 4. Toxin transmitted by motor nerves & nerve fibres. Also delivered by blood to the CNS. Clinical symptoms. 1.Generalised tetanus most common. Incubation period: Variable (Distance of wound from CNS). Involves masseter muscles “lockjaw”. Typical sardonic smile results from sustained contraction. Other signs; drooling, sweating, irritability & back spasms. Spasms involve neck & jaws. Disease called “lockjaw” syndrome. Death occurs by muscular spasms affecting the respiratory system. 2.Localised tetanus. Confined to musculature at primary site. 3.Cephalic tetanus: Primary site is head. Prognosis very poor. 4.Neonatal tetanus: “Tetanus neonatarum”. Umbilical stump infection can lead to generalised tetanus. Mortality rate more than 90%. Laboratory diagnosis. Clinical presentation important. Specimen: From site of primary infection. Microscopy: Gram-positive, “drum stick”. Fluorescent Staining: More sensitive. Culture: Blood agar anaerobic incubation. Difficult for few bacteria in lesions & killed in air. Inoculate Cooked Meat Broth. Confirmatory test: After isolation confirm by detection of toxin using anti-toxin neutralisation test. Virulence in animals: Used to test the toxin. SporeForming/ mednotes/razina 7 Treatment. 1. Debridement of wound. 2. Metronidazole eliminate vegetative bacteria. 3. Passive immunisation with tetanus immunoglobulin (anti-toxic serum). Specially in un-vaccinated individuals or those with out boosters. 4. Active immunisation: Vaccination with tetanus toxoid (DPT). Prevention. Diphtheria Pertussis Tetanus “DPT” Vaccine. 3 doses of formalin inactivated tetanus toxoid. At 2,4 and 6 months of age. Boosters at 18 months and then followed by boosters every 5-10 years. Important for military personnel, ladies prior to pregnancy and children at school age. **** C.perfringens - Gas gangrene Characteristics C.perfringens causative agent of gas gangrene. Other species sometimes involved are; C.novyi, C.histolyticum & C.septicum. Large, rectangular, Gram-positive bacilli. Spores subterminal, not bulging, spores rarely in-vivo or in-vitro isolation. Non-motile. Culture: Haemolytic colonies on blood agar. Ferments carbohydrates and produces gas. Produces at least 12 different toxins and numerous enzymes as virulence factors. Diseases: (1).Severe necrotising wound infection (2).Self-limiting gastroenteritis. (3).Severe haemorrhagic diarrhoea. SporeForming/ mednotes/razina 8 Virulence factors 12 different toxins & enzymes named using Greek letters; α,β …. α-toxin or lecithinase most important. Produces cell membrane hydrolysis & cell destruction. Other enzymes include; collagenase, hyaluronidase, fibrinolysin, DNase & neuraminidase. C.perfringens sub-divided into five serotypes. A,B,C,D and E. Type A most common, (also for gas gangrene) . Type C produces severe life threatening diarrhoea. Type A produces a heat labile “enterotoxin”. Affects ion transport in the intestine & membrane permeability. Gas Gangrene (Wound infection): Pathogenesis. 1. Infection follows contamination of wounds with spores (invasive infection in damaged tissue). 2. Wounds could be result of; military casualties, automobile or farm equipment accidents. 3. Bacteria & spores found in human & animal excreta. 4. Spores indirectly derived from; dirty clothing, street dust or air in hospital operating theatres from poorly designed ventilation system. 5. Bacteria germinate then secrete exotoxins & enzymes cause tissue destruction. Disease spreads rapidly in a necrotic environment. 6. Bacteria ferment carbohydrates & produce gas in tissues. Pressure from gas causes restriction of blood supply & necrosis. In absence of surgical and anti-toxic treatment severe toxaemia and death frequently occur. C.perfringens can also cause diffuse spreading cellulitis accompanied by toxemia. Abdominal infections may originate from the large intestine either from a bowel perforation or contaminated injection site. Perineal infections from intestinal organisms more common in hospitalised patients. C.perfringens in female genital tract as normal flora. Can induce abortions & uterine gas gangrene. Myonecrosis or gas gangarene is life threatening. Symptoms; intense pain about one week after infection. Followed by extensive muscle necrosis, shock, renal failure and death often within 48 h of onset. SporeForming/ mednotes/razina 9 Examination reveals necrotic tissue and presence of gas due to metabolic activity of rapidly dividing bacteria. Toxins cause extensive haemolysis and bleeding. Other Soft tissue Infections include: Cellulitis, Fascitis or supparative myositis. Food Poisoning: (Common disease). Produced by C.perfringens type A. Incubation period 8-24 h. Symptoms: Abdominal cramps & watery diarrhoea, but no fever, nausea or vomiting. Lasts about 24 h. Associated with; meat products containing spores of C.perfringens type A. Prevention: Refrigerate prepared food to prevent production of enterotoxin. Adequate heating of food can destroy the toxin. Necrotising Enteritis: (Rare, acute necrotising process in intestine.) Symptoms: Abdominal pain, bloody diarrhoea, shock and peritonitis. Mortality rate 50%. Produced by type C. Risk factors include exposure to large numbers of bacteria and malnutrition. Septicaemia: Serious infection. Must consider significance of isolate (may be contaminant from skin). Laboratory Diagnosis. • • • • • 1. Specimens : Exudate or biopsy material. Microscopy : Gram-positive bacilli in specimens. Culture : Anaerobic culture on blood agar. Inoculate cooked meat broth & sub-culture. Confirmatory tests: Nagler reaction: α-toxin “lecithinase” breaks down lecithin in egg yolk media shown by an “opaque” area around the colony. Presence of anti-toxin on the media stops the action of the toxin. 2. Stormy fermentation in milk. Coagulated milk “blown apart” by gas produced due to lactose fermentation. 3. Biochemical tests can be used to identify individual species. SporeForming/ mednotes/razina 10 Treatment & Control. Surgical cleansing of wounds most important. Anti-toxin may be used when complete surgical debridement not possible. Penicillin useful in tissue which still have blood supply. Hyperbaric oxygen chambers: Infected tissue placed in chamber containing oxygen under pressure have some success in stopping growth of these organisms. Prognosis poor. Mortality rate from 40-100% in severe infections. Control difficult because of the ubiquitous distribution of this organism. Clostridium botulinium. ****** Characteristics C.botulinium found in soil & water globally. Causative agent of “botulinium” food poisoning with canned or preserved food. Heterogenous group. Fastidious,spore forming, anaerobic bacilli. Motile with peritrichious flagella. Spores are oval, bulging & sub-terminal. Grows best 35–37°C. Some strains grow & produce toxin at low temperatures. Spores survive boiling for hours. Killed by autoclaving. Seven antigenically distinct toxins A – G. Human disease caused by A, B, E and F. Pathogenesis Botulism neurotoxin toxin the most poisonous natural substances. 1ml of culture fluid lethal for 2 million mice and 1µg lethal for humans. Preformed neurotoxin is absorbed from GIT. NOT destroyed by intestinal enzymes. After absorbtion into blood stream it binds irreversibly to presynaptic nerve endings of peripheral nervous system and cranial nerves where it inhibits (neurotransmitter) acetylcholine release. Also produces a binary toxin with two components that affect vascular permeability. SporeForming/ mednotes/razina 11 1. Foodborne botulism. Neurotoxin present in food. From preserved foods (often canned). Insufficient heating important cause in home canning. Types A & B in home-canned foods & type E in preserved fish. Smoked, salted or spiced meat also involved. Food does not look spoiled but small taste causes symptoms. Incubation period 1-2 days (or longer). Oculomotor muscles affected. Initial symptoms; blurred vision, diplopia, drooping eye lids, dilated pupils, dry mouth, nausea, vomiting, constipation & abdominal pain. Problems in speech & swallowing. Signs of “bulbar” paralysis are progressive with weakness & sleepiness. Death is due to respiratory or cardiac failure. Mortality rate was as high as 70% now reduced to 10%. 2. Infant botulism Bacteria from environment or food. Honey sometimes associated with this disease. Colonises GIT of babies. Absence of normal flora helps colonisation. Adults also exposed to C.botulinium but it cannot proliferate because of normal flora. Neurotoxin produced in GIT of infants (different from foodborne disease). Disease affects children less than 1 yr (usually 1-6 m). Clinical symptoms non-specific. Include; constipation, weak cry and “failure to thrive”. Progressive disease with flaccid paralysis and respiratory arrest. “Floppy child syndrome” Some infant deaths previously attributed to other syndromes such as “sudden infant death syndrome” may be a result of botulism. 3. Wound Botulism Wound botulism not always in serious wounds. Even with minor wounds needs to considered in patients with typical symptoms. Symptoms: Blurred vision, weakness and difficulty in swallowing. Abdominal symptoms less pronounced than in food borne infections. SporeForming/ mednotes/razina 12 Laboratory Diagnosis. Specimen: Food sample, faeces or vomit. Isolation from faeces improved by heating. Wound exudate or serum. Detect bacteria or toxin. Microscopy: Typical appearance. Culture: Anaerobic culture on blood agar. Confirmatory tests: Lipase production, Hydrolyse Gelatin, Ferment Glucose and digest milk products. Toxin detection: Toxin –antitoxin neutralisation test. Detect toxin in food or in patient’s blood. Administered to mice with and without anti-toxin. Small amounts of toxin are lethal for mice. Care should be taken in carrying out tests because of virulence of toxin. Treatment. 1. Remove unabsorbed toxin from stomach and intestines. 2. Neutralise unfixed toxin. Suspected cases administered anti-toxin ( polyvalent / types A,B & E). Does not neutralise fixed toxin but free residual toxin. Infants not administered anti-toxin because horse derived and may produce hypersensitivity. 3. Administer metronidazole & penicillin. 4. Administer relevant intensive care (ventilation) and support. Control. Avoid home canning. Home canned vegetables should be boiled for 10 min. Sterilised home canned (pressure cooker) vegetables should be maintained at the high temperature for 15 min. Outbreaks from variety of foods reported specially when food precooked & stored at ambient temperature for 1-2 days. Prophylactic dose of anti-toxin to be given to suspected cases. Active immunization: Administer toxoid preparation in 3 doses, 2 months. Produces solid immunity but routine usage not warranted. Recommended for laboratory workers. ******* SporeForming/ mednotes/razina 13 C.difficile Characteristics & Epidemiology Motile, Gram-positive, oval, sub-terminal spores. Found in faeces of neonates & babies until weaning. Not usually a commensal in adults. Evidence suggests organisms from exogenous source may enter patients whose intestinal colonisation resistance has been affected by antibiotic usage. C.difficile normal flora (endogenous) in some adults (10%) & when other antibiotic sensitive organisms are eliminated from intestine these grow in large numbers to produce disease. Pathogenesis C.difficile produces antibiotic associated gastrointestinal diseases ranging from mild self limiting diarrhoea to severe life threatening ‘pseudomembranous colitis’. Diarrhea may be watery or bloody with abdominal cramps, leukocytosis & fever. Antibiotics particularly associated are clindamycin & ampicillin. Some cephalosporins also implicated and there is virtually no antibiotic which is blame free. Produces two toxins; 1. Toxin A: Potent Enterotoxin produces diarrhea & has cytotoxic activity binds to brush border membranes of the gut at receptor sites. 2. Toxin B: Potent Cytoxin. Has lethal effects. Laboratory diagnosis Specimen collection, microscopy and culture on selective media. Confirmatory test: Demonstrate the presence of toxin. Both toxins can be detected in faecal samples. Cytoxin (toxin B) shown in tissue culture cells. Enterotoxin (toxin A) detected by immuno-assays. Commercial kits using latex agglutination or ELISA tests available for detecting both toxins. SporeForming/ mednotes/razina 14 Treatment. 1. Discontinue use of implicated antibiotic. Most patients recover spontaneously. 2. Suppress growth & toxin production by; oral vancomycin & metronidazole. 3. Relapses are frequent in 20 – 30% cases. Only vegetative forms of bacteria killed by antibiotic. Spores are resistant. Second course of treatment with same antibiotic often successful. Control. 1. Difficult as bacteria commonly exists in hospitals specially in areas near infected patients. 2. Spores difficult to destroy hence bacteria may survive in environment for months and is a major cause of nosocomial outbreaks. ****** SporeForming/ mednotes/razina 15