* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Kawasaki Disease
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Henipavirus wikipedia , lookup
Neonatal infection wikipedia , lookup
Brucellosis wikipedia , lookup
Lyme disease wikipedia , lookup
Trichinosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Chagas disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Yellow fever wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hepatitis B wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Orthohantavirus wikipedia , lookup
Typhoid fever wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
West Nile fever wikipedia , lookup
Marburg virus disease wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Schistosomiasis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Leptospirosis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
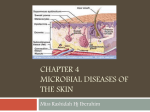
FEVER AND RASH IN A 5 MONTH OLD INFANT David H. Rubin, MD Department of Pediatrics St Barnabas Hospital Professor of Clinical Pediatrics Albert Einstein College of Medicine CASE HISTORY 5 month old immunized female T98.6°F, P 127, RR 32 Diffuse macular eruption on face, arms and trunk Decreased intake and urine output Diarrhea (blood tinged), vomiting, cough CASE HISTORY Seen 2d prior to ED visit and Rx Amoxicillin due to otitis media (also did stool culture negative) Developed petechial rash on arms after 2-3 hours in ED WBC 11.6, 74% lymph, no bands CSF: glucose 62, protein 38, WBC 4 RBC 170 Rx: ceftriaxone FEVER AND RASH – DIFFERENTIAL DIAGNOSIS I Rubeola (measles virus) Rubella (rubella virus) Erythema infectiosum (5th disease; human parvovirus B19) Roseola (human herpesvirus 6) Lyme disease (borrelia burgdorferi) Erythema multiforme (idiopathic) Secondary syphillis (treponema pallidum) Meningococcemia (neisseria meningitidis) FEVER AND RASH – DIFFERENTIAL DIAGNOSIS II Rocky Mountain Spotted Fever (rickettsia rickettsii) Scarlet Fever (beta-hemolytic streptococcus) Toxic shock syndrome (staphylococcus aureus) Kawasaki disease Varicella (varicella-zoster virus) Herpes zoster (varicella-zoster virus) Rickettsialpox (rickettsia akari) Erythema nodosum (various causes) Enteroviral infection INFECTIOUS GASTROENTERITIS ETIOLOGY Viruses – rotavirus, Norwalk Shigella Salmonella Campylobacter Entamoeba histolytica E coli 0157:H7 Cryptosporidium C. difficile Giardia lamblia Vibrio Cholera Cyclospora RECTAL BLEEDING AND DIARRHEA (Boyle, PIR, 2008) Infectious colitis (salmonella, shigella, yersinia, campylobacter, e coli 0157, aeromonas hydrophilia, klebsiella, c. difficile, n. gonorrhea, cmv, e histolytica, trichuris trichura) Hemolytic uremic syndrome Necrotizing enterocolitis Eosinophilic proctocolitis IBD – ulcerative colitis, Crohn disease DEHYDRATION AND SYMPTOMS RUBEOLA Etiology: measles virus – single stranded RNA paramyxovirus Affects upper respiratory tract and regional lymph nodes during brief viremia Secondary viremia spreads 5-7 days later as virus infected monocytes spread virus to respiratory tract, skin, and other organs RUBEOLA Rash: macular/papular may become confluent; begins face, neck spreads out and inferior, rash secondary to vasculitis Most common 5-9 year olds Exposure from large respiratory droplets; requires close contact Infected people contagious 1-2 days prior to symptoms and 4 days after the rash RUBEOLA “Modified measles” • Cases of mild measles in people with partial protection • Usually children vaccinated prior to age 12 months (with or without coadministered immune serum globulin or • Persons receiving immunoglobulin RUBEOLA Symptoms: •Stage 1 (invasion): coryza, cough, conjunctivitis, Koplik spots •Stage 2 (eruption): fever, high temperature, maculopapular (morbilliform) rash (blanches on pressure), abdominal pain, pneumonia •Stage 3 (convalescence): rash fades, low grade temperature RUBEOLA Basis for diagnosis: serology – test for IgM antibodies Confirmation of diagnosis • Multinucleated giant cells in nasal mucosa smears • Virus isolation of culture • Antibody increase between acute and convalescent serum RUBEOLA - COMPLICATIONS Otitis media (most common); mastoiditis Abdominal pain – watch for appendicitis due to swelling of Peyer’s patches, obstruction Pneumonia from secondary bacterial infection Myocarditis Encephalitis (most serious) Late onset: subacute sclerosing pan encephalitis (autoimmune phenomenon) RUBEOLA - TREATMENT No specific treatment Hydration, antipyretics Avoid intense light (for photophobia) IV ribavirin ??? High dose vitamin A improves outcome for • Populations at risk for severe infections – infants 6 • • months - 2 years of age HIV infected infants Children in endemic areas in developing countries RUBEOLA - TREATMENT Prevention: live virus vaccine at 12-15 months and 4-6 years • Contraindications: severe HIV disease, immunocompromised children with congenital immunodeficiency, cancer chemotherapy, immunosuppressive dose of steroids Susceptible household contacts with a chronic disease or immunocompromised exposed to measles need to receive post exposure prophylaxis with measles vaccine within 72 hours of exposure or immunoglobulin within 6 days of exposure MACULOPAPULAR ERUPTION KOPLIK SPOTS TYPICAL MEASLES EXANTHEM: ERYTHEMATOUS MACULOPAPULAR RASH Zenel, J. A. Pediatrics in Review 2000;21:105-107 Copyright ©2000 American Academy of Pediatrics RUBELLA (German or 3 days measles) Invades respiratory tract and disseminates by a primary viremia Low grade temperature Rash usually starts on face and spreads outward; maculopapular but not confluent Most contagious 2 days prior to rash and 5-7 days after rash Arthralgias, postauricular lymph node swelling Complications: Encephalitis (rare), ITP from vaccine RUBELLA 20% of patients – Forschheimer spots – rose spots on soft palate Mild pharyngitis, conjunctivitis, anorexia, headache, low grade fever Polyarthritis of the hands common in older women Paresthesias Tendinitis Treatment – supportive; maintain hydration and give antipyretics RUBELLA Infection in utero: congenital rubella syndrome (crs) • If infection in 1st trimester – 90% of fetuses infected • Cataracts, deafness, PDA Infects with CRS may shed virus in nasopharyngeal secretions and urine for more than 1 year – can easily transmit virus RUBELLA MMR at 12-15 months; rubella shed after vaccination from nasopharynx but not communicable Pregnant women should be immunized after delivery Avoid pregnancy for 28 days after receiving vaccine After vaccination, post pubertal females may experience arthralgias in 25% of cases • May occur 1-3 weeks after vaccination RUBELLA Contraindications to vaccination – similar to rubeola Susceptible non-pregnant persons exposed to rubella should receive rubella vaccination Immunoglobulin should be administered when pregnant women are exposed to rubella and elective abortion is not an option RUBELLA VARICELLA Chickenpox and zoster - caused by varicella-zoster virus Chickenpox is the primary infection; zoster is a reactivation infection VZV infects susceptible persons via conjunctivae or respiratory tract VARICELLA Disseminates by primary viremia and infects regional lymph nodes, liver, spleen and other organs Secondary viremia follows resulting in a cutaneous infection/rash • After resolution of the rash, virus persists in latent infection in dorsal root ganglia cells • Zoster (shingles) is a reactivated of latent infection of endogenous VZV VARICELLA Exposure – respiratory droplets; incubation 9-28 days (mean=13) after contact Period of communicability is 2 days before and 7 days after lesions crusted over Symptoms: low grade fever, lesions of various sizes/shapes Treatment: symptomatic, avoid aspirin, antiviral in selected cases VARICELLA Pre-eruption phase of zoster includes intense pain and tenderness along dermatome with malaise and fever Papules appear which vesiculate ; group of lesions appear for 1-7 days Any branch of cranial nerve V may be affected – which may result in corneal and/or intraoral lesions If cranial nerve VII involved facial paralysis and ear canal vesicles (Ramsey Hunt syndrome) VARICELLA - TREATMENT Non aspirin antipyretics Cool baths Hygiene Immunocompromised? • Early therapy with antivirals (eg acyclovir) may prevent pneumonia, encephalitis, death • For nonpregnant persons ≥ 13 yrs and children ≥ 12 months with chronic cutaneous or pulmonary disease receiving steroids or long term salicylates VARICELLA - COMPLICATIONS Secondary infections (staph/strep) most common; may be life threatening with toxic shock syndrome/necrotizing fasciitis Varicella gangrenosa – thrombocytopenia with hemorrhagic lesions Pneumonia Myocarditis/pericarditis Hepatitis VARICELLA - COMPLICATIONS Glomerulonephritis Orchitis Arthritis Ulcerative gastritis Encephalitis (cerebellar ataxia may occur without encephalitis) Reyes syndrome VARICELLA - OTHER ISSUES Primary varicella in pregnant woman fetal varicella infection • Low birthweight, cortical atrophy, seizures, mental retardation, chorioretinitis, cataracts, intracranial calcifications Children exposed in utero to VZV may develop zoster without varicella VARICELLA - OTHER ISSUES Severe neonatal varicella • Occurs in newborns of mothers with varicella (not shingles) 5 days before or 2 days after delivery • Child born prior to maternal antibody response develops • Treat infants ASAP with varicella zoster immunoglobulin VARICELLA Children with varicella- no return to school until all lesions crust over Live viral vaccine at 12-18 months and 19 months – 13th birthday Passive immunity with VZIG given within 96 hours of exposure for high risk persons • Immunocompromised • Neonates of mothers with neonatal varicella VARICELLA ERYTHEMA INFECTIOSUM – 5TH DISEASE Human parvovirus B19 Slapped cheek syndrome Spread is respiratory Initial viremia at 7-10 days; mild flu-like illness Rash at 10-17 days represents immune response; patients are only contagious up to presence of rash ERYTHEMA INFECTIOSUM – 5TH DISEASE Mild systemic symptoms (fever, malaise, sore throat) in 50% of children Complications • Arthritis: F>M, older>younger • Aplastic crisis: usually not noticed in patients with normal erythrocyte half-life BUT results in severe anemia in those with any chronic hemolytic anemia (rash follows hemolysis) • Pregnancy: early miscarriage, late hydrops fetalis ERYTHEMA INFECTIOSUM – 5TH DISEASE ERYTHEMA INFECTIOSUM – 5TH DISEASE ROSEOLA Cause: human herpes virus 6 and 7 Seen in children 6 mo-3 yrs Clinical findings: • Sudden onset of fever – common to see >40C which may last up to 8 days (mean 4 days), followed by diffuse maculopapular eruption • Fatigue, irritability, URI symptoms (but no conjunctivitis or exudative pharyngitis), diarrhea and vomiting (30% of pts), swollen eyelids may precede fever ROSEOLA - COMPLICATIONS Febrile seizure (10% of pts) HHV-6 can cause meningoencephalitis or aseptic meningitis Multiorgan disease can occur in immunocompromised patients • Pneumonia • Hepatitis • Bone marrow suppression • Encephalitis ROSEOLA ROSEOLA LYME DISEASE Subacute or chronic spirochetal infection caused by Borrelia burgdorferi transmitted by the bite of a deer tick Erythema chronicum migrans develops in 6080% of patients (most characteristic feature) • Occurs between 3-30 days; may reach diameter of 20 cm Arthritis – seen in 50% of patients weeks to months after bite • Recurrent attacks of migratory, monoarticular or • pauciarticular involving knees and other large joints Chronic arthritis develops in 10% of patients LYME DISEASE Neurological symptoms in 20% of patients; untreated symptoms may become chronic or permanent • Bell’s palsy, aseptic meningitis, peripheral neuritis, GuillainBarre syndrome, encephalitis, ataxia, chorea Cardiac disease in 5% of patients Serologic diagnosis based on • Heart block or myocardial dysfunction • ELISA • Immunoblot to confirm ELISA (if positive or questionable) • Causative organism difficult to culture LYME DISEASE - TREATMENT Based on ISDA 2006 http://www.journals.uchicago.edu/doi/full/10.1 086/508667 Routine use of antibiotics after tick bite not supported Treatment with docycycline (> 8 yrs of age), amoxicillin, or cefuroxime is recommended for early or late LD associated with ECM Neurologic symptoms – ceftriaxone Cardiac symptoms – ceftriaxone, ?pacemaker LYME DISEASE LYME DISEASE KAWASAKI DISEASE Vasculitis of unknown etiology Multisystem involvement and inflammation of small and medium sized arteries with aneurysm formation More common among children of Asian decent Usually children <5 years; peak 2-3 years KAWASAKI DISEASE In children < 3 months of age • Usually see atypical course leading to rapid and severe coronary artery damage (CAD) • ECHO mandatory if considered in this age group; diagnosis very difficult Age is independent risk factor for CAD CAD develops in 5% of timely treated patients Incomplete/atypical definition • Fever, at least 2 of the clinical criteria for KD, and laboratory data showing systemic inflammation; 2D echos should be performed KAWASAKI DISEASE Prolonged fever is hallmark of the disease Lymphadenopathy is least common finding (seen in 75% of cases compared with 90% for other signs) Coronary lesions are usually not present until 10 days; therefore decision to treat made prior to knowledge of cardiac outcome Other useful signs • Extreme irritability • Inflammation of BCG scar KAWASAKI DISEASE – CLINICAL PRESENTATION Acute phase (1-2 weeks) • Sudden onset of high fever followed by conjunctival erythema, mucosal changes, cervical adenopathy, swelling of hands and feet • Irritability • Abdominal pain, hydrops of gall bladder • Arthritis • Carditis – tachycardia, CHF, giant coronary artery aneurysms KAWASAKI DISEASE – CLINICAL PRESENTATION Subacute phase Convalescent phase • Lasts up to 4th week • Resolution of fever and other symptoms • Desquamation of fingers and toes • Elevation of platelet count • Coronary artery aneurysms • Disappearance of clinical symptoms • 6-8 weeks after initial symptoms CLINICAL DIAGNOSIS KAWASAKI DISEASE Still difficult to diagnosis – especially in incomplete or atypical form Atypical Kawasaki Disease: 3 clinical criteria + identification of coronary aneurysms Despite timely treatment, 15% of patients have persistent fever which require steroids, additional immunoglobulins, and immunosuppressant medication Children apparently normal during initial exam may develop cardiac findings later in life KAWASAKI DISEASE COMPLICATIONS Coronary artery thrombosis and coronary and peripheral artery aneurysm Myocardial infarction Myopericarditis Congestive heart failure Hydrops of gall bladder Aseptic meningitis Arthritis Sterile pyuria (urethritis) Thrombocytosis Diarrhea Pancreatitis Peripheral gangrene KAWASAKI DISEASE - TREATMENT IV Immunoglobulin (mechanism unknown) • Single dose of 2 g/kg over 12 hours • Rapid defervescence and symptom resolution • Reduces incidence of coronary artery aneurysm Aspirin 80-100 mg/kg/day divided q 6 hours for 48 hours then reduce by ½ • Continue for 6-8 weeks until cardiac ECHO shows no evidence of cardiac pathology ERYTHEMATOUS MACULAR ERUPTION - KAWASAKI SYNDROME DESQUAMATION OF THE SKIN ANGULAR CHELITIS STRAWBERRY TONGUE CONJUNCTIVAL INJECTION SCARLET FEVER Erythrogenic toxin produced by strains of Group A beta hemolytic streptococci - usually seen 24-48 hrs after pharyngitis May also be seen following infection of wounds, burns, streptococcal skin infection, impetigo, cellulitis Punctate erythema starts on trunk and spreads to extremities, becoming confluent; rash fades in 4-5 days; desquamation may occur Treatment: penicillin or erythromycin SCARLET FEVER SCARLET FEVER – STRAWBERRY TONGUE MENINGOCOCCEMIA Etiology: Neisseria meningitidis; Gram negative organism with endotoxin in cell walls causing capillary vascular leak and DIC May be carried asymptomatically for months in upper respiratory tract; 1% of carriers develop disease Classified serologically by groups based on capsular polysaccharide; systemic disease usually caused by: A, B (1/3 of cases), C (25%), Y (25%), W-135 (15%) May produce isolated infection to septic shock and: meningitis, sepsis, septic arthritis, pericarditis, pneumonia, chronic meningococcemia, otitis media, conjunctivitis, and vaginitis MENINGOCOCCEMIA Since 1982, vaccine available (menomune) against groups A, C, Y, W135; recent release of conjugated vaccine menactra for superior coverage • No coverage of Group B – responsible for cases in infants < 1 year of age and large number of cases in US and UK MENINGOCOCCEMIA Prodrome of URI followed by rapid onset of high fever, headache, nausea, toxicity, hypotension Purpura usually seen on extremities May be followed by signs/symptoms of meningitis • Neck stiffness, vomiting, stupor Complications: permanent CNS damage, deafness, seizures, paralysis, cognitive deficits Treatment: vancomycin and cefotaxime to start; after isolation of N. meningitidis, may use penicillin MENINGOCOCCEMIA MENINGOCOCCEMIA ROCKY MOUNTAIN SPOTTED FEVER Cause is R. rickettsii, gram negative coccobaccillus, which invades endothelial walls of blood vessels producing vasculitis and eventually increased permeability and organ failure Most common rickettsial disease in USA 40% of patients unable to recall history of tick bite ROCKY MOUNTAIN SPOTTED FEVER Nonspecific fever within 5-10 days after tick bite Classic presentation rarely seen: fever, rash, tick bite • More likely: fever, severe headache, vomiting, muscle pain, lost appetite Early small flat, pink, macules on wrists, ankles, blanch with pressure Late rash (petechial), abdominal pain, joint pain, diarrhea ROCKY MOUNTAIN SPOTTED FEVER Laboratory: hypoNa, increased LFTs, thrombocytopenia Multisystem involvement: respiratory, CNS, renal, GI G6PD deficient patients have high risk for early death Indirect immunofluorescence assay (IFA) - reference standard in Rocky Mountain spotted fever serology May also use ELISA, latex agglutination, and dot immunoassays ROCKY MOUNTAIN SPOTTED FEVER Therapy should not be postponed pending laboratory confirmation Rx: Docycycline or chloramphenicol Complications • Noncardiogenic pulmonary edema (ARDS) • DIC • Circulatory collapse • Multiple organ failure (myocarditis, encephalitis, hepatitis and renal failure) ROCKY MOUNTAIN SPOTTED FEVER ROCKY MOUNTAIN SPOTTED FEVER TOXIC SHOCK SYNDROME Severe prolonged shock caused by a toxin produced by S. aureus or streptococcal pyogenes (group A strep) Approximately 400 cases/year in USA May be seen in • Abscesses, animal bite, barrier contraception (cervical • cap, diaphragm, sponge), breast augmentation surgery, burns Wounds, bursitis, croup, deep and superficial soft tissue infections TOXIC SHOCK SYNDROME May also be seen in: • Dermatological surgery, empyema, endometritis, influenza, insect bite, lymphadenitis • Nasal packing, postoperative complication, postpartum period • Septic abortion, sinusitis, tampon use • Tracheitis, varicella zoster TOXIC SHOCK SYNDROME TOXIC SHOCK SYNDROME ENTREROVIRAL INFECTIONS ENTREROVIRAL INFECTIONS Named due to their replication in GI tract Over 70 different serotypes – originally named as echovirus, coxsackievirus – now named by number Transmission by fecal oral route Clinical: viral paralysis, acute hemorrhagic conjunctivitis, herpangina Watch for myocarditis or pericarditis ENTEROVIRAL INFECTIONS •Symptoms variable -Nonspecific URI symptoms, or enteric symptoms (vomiting and diarrhea), fever, irritability •Rash variable (occurring on 2-4th day of fever) -Usually erythematous maculopapules or morbilliform; vesicular, urticarial, or petechial •Transmission is fecal-oral or from upper respiratory secretions •Summer - fall outbreaks •Treatment supportive