* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical approach to determination of the need for prophylaxis in
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
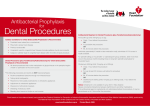
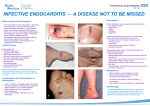
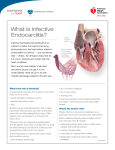
When do you give prophylactic treatment in MVP? Clinical approach to determination of the need for prophylaxis in patients with suspected MVP Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association • A reasonable approach for endocarditis prophylaxis should consider the following: – the degree to which the patient’s underlying condition creates a risk of endocarditis – the apparent risk of bacteremia with the procedure – the potential adverse reactions of the prophylactic antimicrobial agent to be used; and the cost-benefit aspects of the recommended prophylactic regimen Failure to consider all of these factors may lead to overuse of antimicrobial agents, excessive cost, and risk of adverse drug reactions Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association • Prophylaxis is recommended in individuals who have a higher risk for developing endocarditis than the general population and is particularly important for individuals in whom endocardial infection is associated with high morbidity and mortality Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Endocarditis prophylaxis recommended High-risk category • Prosthetic cardiac valves • Previous bacterial endocarditis • Complex cyanotic congenital heart disease Eg. Single ventricle states, Transposition of the great arteries, Tetralogy of Fallot • Surgically constructed systemic pulmonary shunts or conduits Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Moderate-risk category • Acquired valvular dysfunction (eg, rheumatic heart disease) • Hypertrophic cardiomyopathy • Mitral valve prolapse with valvular regurgitation and/or thickened leaflets Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Endocarditis prophylaxis NOT recommended Negligible-risk category • Isolated secundum atrial septal defect • Surgical repair of ASD, VSD or PDA • Previous coronary artery bypass graft surgery • Mitral valve prolapse without valvular regurgitation • Physiologic, functional, or innocent heart murmurs • Previous Kawasaki disease without valvular dysfunction • Previous rheumatic fever without valvular dysfunction • Cardiac pacemakers and implanted defibrillators Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Prophylaxis • Prophylaxis at the time of cardiac surgery should be directed primarily against staphylococci and should be of short duration • First-generation cephalosporins are most often used • Prophylaxis is most effective when given perioperatively in doses that are sufficient to assure adequate antibiotic concentrations during and after the procedure • Antibiotics should be used only during the perioperative period - initiated shortly before a procedure and should not be continued no more than 6 to 8 hours • In the case of delayed healing, or of a procedure that involves infected tissue, it may be necessary to provide additional doses of antibiotics Prophylaxis Antimicrobial prophylaxis administered within 2 hours following the procedure will provide effective prophylaxis Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Streptococcus viridans is the most common cause of endocarditis following: – dental or oral procedures – certain upper respiratory tract procedures – bronchoscopy with a rigid bronchoscope – surgical procedures that involve the respiratory mucosa – esophageal procedures Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association • The recommended standard prophylactic regimen for all these procedures is a single dose of oral amoxicillin to be administered 1 hour before the anticipated procedure – Adult dose is 2.0 g – Pediatric dose is 50 mg/kg (not to exceed adult dose) • For individuals who are unable to take or unable to absorb oral medications, parenteral Ampicillin sodium is recommended Durack DT. Prevention of infective endocarditis. N Engl J Med. 1995 • Individuals who are allergic to penicillin – Clindamycin hydrochloride – Azithromycin or clarithromycin • When parenteral administration is needed in an individual who is allergic to penicillin, clindamycin phosphate is recommended Durack DT. Prevention of infective endocarditis. N Engl J Med. 1995 Prophylaxis • Enterococcus faecalis is the most common cause of bacterial endocarditis that occurs following genitourinary and gastrointestinal tract surgery or instrumentation • Antibiotic prophylaxis should be directed primarily against Enterococci Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association • High-risk patients – Ampicillin plus gentamicin • High-risk patients allergic to ampicillin/amoxicillin – Vancomycin plus gentamicin • Moderate-risk patients – Amoxicillin or ampicillin • Moderate-risk patients allergic to ampicillin/amoxicillin – Vancomycin Prevention of Bacterial Endocarditis: Recommendations by the American Heart Association