* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical
Polysubstance dependence wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Drug design wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmacognosy wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Prescription costs wikipedia , lookup
Toxicodynamics wikipedia , lookup
Norepinephrine wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Theralizumab wikipedia , lookup
Drug interaction wikipedia , lookup
Chlorpromazine wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Antipsychotic wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
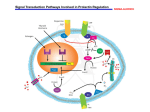
Review 1. Introduction 2. Physiological function and control of prolactin secretion 3. Prolactin receptors, mechanisms of activation and Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. consequences 4. Hyperprolactinemia 5. Pharmacokinetic and pharmacodynamic particularities of antipsychotics and consequences on prolactin secretion 6. Expert opinion Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences Victor Voicu†, Andrei Medvedovici, Aurelian Emil Ranetti & Flavian Ştefan Rădulescu † University of Medicine and Pharmacy Carol Davila, Faculty of Medicine, Department of Clinical Pharmacology, Toxicology and Psychopharmacology, Bucharest, Romania Introduction: The altered profiles of prolactin secretion in the anterior hypophysis, generated by pathological, pharmacological or toxicological causes, have special consequences on multiple functions in both genders. Areas covered: This selective review presents the main mechanisms controlling prolactin secretion, focusing on the interplay of various neurotransmitters or xenobiotics, but also on the role of psychic or posttraumatic stress. A detailed analysis of several pharmacotherapeutic groups with hyperprolactinemic effects emphasize on the relevance of the pharmacokinetic/pharmacodynamic mechanisms and the clinical significance of the long term administration. Expert opinion: Accurate monitoring and evaluation of the hyperprolactinemia induced by xenobiotics is strongly recommended. The typical antipsychotics and some of the atypical agents (amisulpride, risperidone, paliperidone), as well as some antidepressants, antihypertensives and prokinetics, are the most important groups inducing hyperprolactinemia. The hyperprolactinemic effects are correlated with their affinity for dopamine D2 receptors, their blood--brain barrier penetration and, implicitly, the requested dose for adequate occupancy of cerebral D2 receptors. Consequently, integration of available pharmacokinetic and pharmacodynamic data supports the idea of therapeutic switch to non-hyperprolactinemic agents (especially aripiprazole) or their association, for an optimal management of antipsychotic-induced hyperprolactinemia. Possible alternative strategies for counteracting the xenobiotics-induced hyperprolactinemia are also mentioned. Keywords: anterior hypophysis, antidepressants, antipsychotics, blood--brain barrier, dopamine D2 receptors, hyperprolactinemia, logBB, therapeutic switching Expert Opin. Drug Metab. Toxicol. [Early Online] 1. Introduction Prolactin, a polypeptide hormone, is secreted in the anterior hypophysis by the specialized lactotroph cells. Most of the prolactin existing in the hypophysis has a molecular weight of 23 kDa, but there are also molecular variants generated by proteolytic cleavage, posttranslational changes, etc. Prolactin circulates under various molecular forms, with different molecular weights, the usual one being composed of 199 amino acids. Approximately 80 -- 90% of the circulant prolactin is monomeric, but dimeric or polymeric forms, with high molecular weights, could also be observed [1]. Macroprolactin, the high molecular weight circulating form, has a reduced biological activity, a low clearance and can be identified by analytical tests; 10.1517/17425255.2013.791283 © 2013 Informa UK, Ltd. ISSN 1742-5255, e-ISSN 1744-7607 All rights reserved: reproduction in whole or in part not permitted 1 V. Voicu et al. Article highlights. . . Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. . . . Prolactin is secreted by the anterior hypophysis, passes in the systemic circulation and acts on the target structures by the specialized receptors, further generating effects on growth factors, neurotransmission and immunomodulation. Hyperprolactinemia is described as a consequence of specific physiological (pregnancy, lactation) or pathological states (tumors of the lactotroph cells, prolactinomas) or as consequence of action of various exogenous factors, including antidopaminergic drugs and other xenobiotics. The affinity for dopamine D2 receptors, the occupancy half-life and the values of molecular descriptors which are determinants for BBB penetration could be used as predictors of xenobiotics potential to induce hyperprolactinemia. For antipsychotics, switching or association of non-hyperprolactinemic agents could be the optimal approach, in case of clinical significant hyperprolactinemia. The use of hypoprolactinemiant dopaminergic drugs is mainly reserved for hyperprolactinemia associated with prolactinomas and essential hyperprolactinemia. This box summarizes key points contained in the article. therefore it could generate errors in the clinical diagnostic. The use of laboratory methods that specifically identify the various forms of circulating prolactin has been suggested [1]. The posttranslational changes of prolactin alter its biological activity [2,3]. For example, glycosylation decreases the biological activity of prolactin; phosphorylation generates antagonists of prolactin in some species, while the cleavage of the 16K molecule cancels its binding capacity [2]. It is admitted that prolactin has almost 300 functions in different organs and species, but their relevance in humans still needs to be established [4]. Prolactin is also produced in the central nervous system (CNS), being identified in cortex, hypothalamus, amygdala, septum, bulbus, cerebellum, spinal cord, choroid plexus and circumventricular organs. In hypothalamus, the secretion of prolactin is independent from the one in the hypophysis, although the exact function of prolactin produced at this level or elsewhere has not been identified. It must be noted that, for delivery at the CNS level, the circulant prolactin must penetrate the blood--brain barrier (BBB) at the level of the choroid plexus, where an increased density of prolactin receptors has been described [5]. Prolactin or prolactin-like molecules have been identified in placenta, amnion, uterus, mammary glands and milk, with more or less identified functions, subject to numerous studies. A series of other cells, including lymphocytes and immunocompetent thymic cells, contain prolactin. Extensive evaluations have been dedicated to the assessment of the physiological control of prolactin secretion, at the level of the 2 hypophysis lactotroph cells, and to the consequences of the action on these mechanisms during therapy with different drugs and other xenobiotics (Figure 1). Physiological function and control of prolactin secretion 2. Prolactin has a circadian rhythm of secretion, similar to other hormones with major functions, for example, corticosteroids. Its secretion is increased during the sleeping period and decreases in the wakeful state. In the case of corticosteroids, the pattern is reversed, increasing from the first hours in the morning. Extensive proofs emphasize that the dopaminergic tonus controlled by the hypothalamus exerts inhibitory effects on prolactin secretion, correlated with different periods of the day, under the control of the dopaminergic tonus of the tuberoinfundibular neurons. If the first, fundamental aspect of the control of the prolactin secretion refers to its dependence on the prevalent inhibitory tonus of the hypothalamus, the second aspect focuses on dopamine, as the main inhibitory factor of prolactin secretion. Dopamine D2 receptors are located in the membrane of the lactotroph cells. The tuberoinfundibular neurons release dopamine through the portal system in the sinusoidal capillaries of the anterior lobe of hypophysis, being considered as the major physiological regulator of prolactin secretion. The anatomical support of the dopamine system controlling the prolactin release is the tuberoinfundibular and tuberohypophiseal dopaminergic tract. The first dopaminergic projections, the tuberoinfundibular ones, represent the main dopaminergic control of the anterior hypophysis [6]. An important particularity results from the fact that the released dopamine does not interact with the postsynaptic receptors, but reaches the perivascular space, is uptaken by the port circulation and transported to the anterior hypophysis. This generates the neuroselective function characteristic for such neurons [6]. However, it is a rough simplification to consider that the dopamine pathways control the prolactin release, including the dopamine--prolactin interaction. The interference of other multiple factors with positive or negative effects on the control of prolactin release should be considered, as it results from the further succinct presentation. It is admitted that the lactotroph cells have as unique characteristic an intense basal secretory activity of prolactin. The inhibitory tonus of dopamine on this process implicitly requests increased secretion and release of dopamine, induced among other factors, by the high activity of hypothalamic tyrosine hydroxylase (conversion of tyrosine to DOPA and furthermore, to dopamine), which is constitutive active, as an adaptive consequence to the increased request of dopamine. Moreover, the consensus with the phenomenon described previously, the maintenance of a high concentration of dopamine, is achieved also by the absence of dopaminergic auto-receptors at the level of tuberoinfundibular projections, Expert Opin. Drug Metab. Toxicol. [Early Online] Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences Endobiotics Endobiotics Inhibitors of dopamine activity Stimulators of dopamine activity - Serotonin; - Acetylcholine; - Noradrenalin; - TRH (tirotropin releasing hormone); - Histamine; - Oxytocin; Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. - Endogenous opioids; - Angiotensin II; - Somatostatin; - Natriuretic atrial peptide; Xenobiotics Xenobiotics Stimulators of prolactin secretion Inhibitors of prolactin secretion - Antidopaminergic (antipsychotics, digestive prokinetics); - Dopamine agonists; TIDA - Cholinergics; - Serotonin antagonists. - Selective serotonin reuptake inhibitors and other antidepressants; - Opioids, cocaine; DA - Amphetamine-like compounds; - Calcium channels blockers (verapamil); - Simpatholytics (reserpine, α-methyl-dopa). PRL Figure 1. Direct effects of various endobiotics (neurotransmitters, neuromodulators, hormones) and xenobiotics on tuberoinfundibular dopaminergic system (TIDA) and consequently, on prolactin secretion [1,5,37,48,105,106]. therefore removing the negative feedback on the tyrosine hydroxylase activity [6]. The description of dopamine effects on lactotroph cells and of their time dependence is relevant for illustration of their consequences on prolactin secretion. Consecutive to the interaction with D2 receptors at the level of the membrane of lactotroph cells, it determines in few seconds the increase of conductance in potassium channels, inactivating the voltage-sensitive calcium channels. Consequently, a hyperpolarization of the membrane arises, followed by a decrease of intracellular calcium concentration below the threshold of activation of the secretion processes and a consecutive inhibition of prolactin secretion. In the following sequences, after minutes or hours, dopamine generates the inhibition of the adenylylcyclase activity, of the metabolism of inositol phosphate and of the release of arachidonic acid, processes followed by down-regulation of the prolactin gene [7]. The secretion of prolactin acts as a feedback mechanism on the dopamine endocrine neurons, the increase in hormone secretion leading to the increase of hypothalamic synthesis of dopamine. The action of dopamine at the level of specific receptors ends after the neuronal reuptake, by active transport in the dopaminergic nerve endings. The pharmacodynamic (PD) interference to this transport mechanism has, implicitly, consequences on the dopaminergic tonus and, consequently, on prolactin secretion. Other segments of the transduction pathways of the signal at the level of dopamine D2 receptors Expert Opin. Drug Metab. Toxicol. [Early Online] 3 Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. V. Voicu et al. from the membrane of the lactotroph cells which might be influenced pharmacodynamically are the activity of adenylate cyclase, the metabolism of inositol-phosphate, the ionic channels for potassium and voltage-sensitive calcium channels. For example, the net secretion of prolactin can be altered by inhibition of calcium channels and stimulation of potassium channels. There are proofs of the stimulatory action of a component of the serotoninergic center for the secretion of prolactin. The central adrenergic system is involved in the regulation of the prolactin secretion, by modulation of the activity of the tuberoinfundibular neurons. This action is relevant especially in the stress-induced prolactin secretion. Histamine, through H2 receptors, has a stimulatory effect on the prolactin secretion, the process being blocked by the H2 receptors antagonists. The endogenous opioid system of CNS produces the increase of prolactin secretion by inhibiting the dopaminergic neurons in hypothalamus, in various physiological conditions, most probably by activation of µ and k receptors. Their antagonists, for example, naloxone, reduce the stress-induced secretion of prolactin. It is considered that this type of effect of the endogenous opioids is integrated into the neurohumoral adaptive mechanisms [5]. Angiotensin II as principal effector of the renin--angiotensin-aldosterone system, based on its tissue distribution, at the level of CNS, cardiovascular and renal system, has connections and control/regulation functions on the prolactin secretion, in hypothalamus and hypophysis [5]. It seems like the endogenous angiotensin system produces a decrease of the hypothalamus-hypophysis response on increasing prolactin secretion, consecutive to the action of several endogenous and exogenous factors. Calcitonin, a polypeptide secreted by the thyroid, with effects of reduction of the plasma calcium concentration, generates a decrease of prolactin secretion, according to some authors, by activation of the tuberoinfundibular dopaminergic system [8]. A series of experimental proofs emphasize that endothelin and endothelin-like compounds are involved in the control of prolactin secretion, correlated with environmental factors, having variable consequences [9]. These proofs, beside the distribution of endothelin and of its precursors, implicitly of its specific receptors at the level of hypothalamus and hypophysis, suggest that they act as neurotransmitters and neuromodulators of prolactin secretion [5]. The system of amino acids and their specific receptors in the CNS, with important functions in the excitatory (glutamatergic) or inhibitory (GABA-ergic) neurotransmission, is involved also in the control and regulation of prolactin secretion. Essentially, the excitatory amino acids produce effects on prolactin secretion by acting on the hypothalamic receptors, modulating the prolactin releasing or inhibitory factors. The inhibitory amino acids display also either stimulatory or inhibitory activity on prolactin secretion. It is admitted that the main function of the GABA-ergic system is the negative feedback regulation of the prolactin secretion under the influence of several physiological factors [5,10]. 4 Prolactin itself exists in an interrelationship of feedback control with its own secretion/concentration in the biophase. The inhibition of secretion is triggered by activation of hypothalamic dopamine neurons or directly, by acting on the lactotroph cells [5]. The cholinergic system in the hypophysis, by activation of the muscarinic receptors, exerts a tonic inhibitory action on the prolactin secretion [5,11]. Atropine, the competitive antagonist of muscarinic receptors, induces a dose-dependent increase of the prolactin secretion [12]. In a broad review, Freeman et al. [5] pointed out that prolactin secretion and its complex control, correlated with the reproduction and survival of individuals, is a complex, homeostatic process. The control and regulation of prolactin secretion by various endogenous factors is achieved by acting at the level of different effector structures involved in this process, that is, hypothalamus or hypophysis. The impact is variable, according to the physiological status of the organism. Finally, the prolactin reaching the biophase interacts with the prolactin receptors of lactotroph cells, launching the activation of a cascade of events leading to the activation of effector structures. The receptors, having specific membrane disposition, belong to the superfamily of cytokine receptors. The prolactin receptors are present in almost all tissues, with a net expression in liver, mammary glands, suprarenal glands and choroid plexus [13]. These receptors have a single membrane crossing, generating an extracellular domain on which the ligand binds and an intracellular one, coupling the receptors with the signaling molecules [13]. Noteworthy, the prolactin receptors interact with three types of ligands: prolactin, placental lactogen (PL) and growth hormone (GH), resulting in the difficulty in understanding the biological effects [2] and potentially pathological consequences, correlated with the prolactin variations. The first stage of interaction, the binding of prolactin to the receptors, initiates the activation and dimerization, triggering the cascade of intracellular signaling by means of associated kinases which activate the subsequent effectors [2]. This concise summary of the complex functional interrelationships of various systems involved in the homeostasis of prolactin secretion should be considered as a background, the functional basis and potential links and targets, on which various groups of biologically active substances, either drugs or toxicants act and determine changes of the prolactin levels. The complexity of the control and regulation of secretion, beside the considerable number of functions and targets assigned to prolactin (approximately 300) suggest the need to accurately evaluate the relevance and impact of the changes induced by the exposure of human organism to various xenobiotics [4]. Prolactin receptors, mechanisms of activation and consequences 3. Prolactin acts as a hormone. It is secreted by the anterior hypophysis, passes in the systemic circulation and acts on the target structures by the specialized receptors, further Expert Opin. Drug Metab. Toxicol. [Early Online] Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences generating effects such as growth factors, neurotransmission and immunomodulation. The prolactin receptors are produced in various types of cells, with several isoforms and transported at the level of the cell membrane. The interaction with prolactin determines a series of structural changes of the extracellular domain of the receptor, changes transmitted to the intracellular domain which, by its activity controls different signaling pathways [14]. The life cycle of the receptor ends by its removal from the plasma membrane. The critical analysis of the literature reports in the field emphasizes, on one hand, on the protein system by which human prolactin induces its effects on several cellular systems, but also the scarce data explaining their mechanism of action [14]. Obviously, the physiological agonists of the receptor are the lactotroph hormones (GHs, placental lactotroph and prolactin), with prolactin having the central role. Noteworthy, it is considered that prolactin binds and activates the prolactin receptors by a unique mechanism, completely different compared with other lactogens [14]. It is interesting that prolactin receptors are largely distributed in highly different tissues. The 85 identified functions have been standardized into five categories: reproduction, osmoregulation, growth, integument and synergism with corticosteroids [15]. Bole-Feysot et al. added water and electrolytes balance, growth and development, endocrinology and metabolism, brain and behavior, immunoregulation and protection [16]. 4. Hyperprolactinemia Hyperprolactinemia, due to increased secretion of the hormone at the level of the lactotroph cells of the hypophysis, with a plasma concentration above the physiological level, is described as a consequence of specific physiological (pregnancy, lactation) or pathological states (tumors of the lactotroph cells, prolactinomas) or as consequence of action of various exogenous factors, including antidopaminergic drugs and other xenobiotics. Currently, one can state that the single characterized pathological state correlated with prolactin is hyperprolactinemia [2], generated by different mechanisms described briefly herein. It is considered that hyperprolactinemia is involved in approximately 25% of the menstrual disturbances in women [2]. It is to be pointed out that there are proofs linking the high levels of circulating prolactin with the increased risk of mammary cancer in pre- or postmenopausal women [4], without identification of a clear mechanism. A study performed on human mammary cancer cell cultures emphasized that prolactin acts as a potent survival factor for tumor cells, preventing their entry into apoptosis [17]. Moreover, prolactin might contribute to the increased viability of tumor cells, to their resistance to chemotherapy and metastatic processes [18]. Table 1 presents the consequences of hyperprolactinemia in males and females. In female subjects, hyperprolactinemia can induce a series of neuroendocrine disorders, notably breast augmentation, galactorrhea, ovarian dysfunction, decrease of libido, atrophy of urethra and vaginal mucosa, dyspareunia. In addition, hostility, anxiety and depression have been reported [19]. A series of data correlate hyperprolactinemia with breast cancer in male subjects. The experimental proofs, although not clearly confirmed in humans, underline the role of prolactin as initiator and promoter of cancer [20]. On the other hand, available data are contradictory. Moreover, there are concerns regarding the relationship between schizophrenia and various types of cancer. The screening of female schizophrenia patients for breast cancer has been recommended [21]. Moreover, hyperprolactinemia induced by several antipsychotics is not clearly correlated with an increased risk of breast cancer [22]. Therefore, it is rather difficult to clearly state if antipsychotic-induced hyperprolactinemia or schizophrenia determines a high risk of breast cancer. It is beyond doubt that typical antipsychotic (phenothiazine, haloperidol and thioxanthens) produce side effects on the sexual function in 30 -- 60% of schizophrenic patients [23]. In male subjects, hyperprolactinemia induces effects such as reduced libido, erectile and ejaculatory dysfunction, gynecomastia, galactorrhea, reduction of semen volume, priapism. In females, the effects are more intense and of high risk: reduced libido, amenorrhea, dysmenorrhea, gynecomastia, galactorrhea, painful breasts, obesity, risk of osteoporosis, risk of breast cancer. On the whole, it can be concluded that female subjects are more susceptible to drug hyperprolactinemic effects as compared with males [24]. However, the role of prolactin in regulating metabolism or body weight is not clear. Insulin resistance has been correlated with hyperprolactinemia and prolactin inhibits the secretion of adiponectin [25,26]. Effects of psychic and posttraumatic stress on prolactin secretion 4.1. It is admitted that prolactin, its secretion and control, represent a complex process, correlated with the functional status of the organism (adaptative, pathological status, psychic stress, posttraumatic stress) [27-29]. The hormonal response to psychic stress is correlated with the individual particularities, but can generate an effect on prolactin or cortisol secretion. There is a negative correlation between peak secretion of prolactin and cortisol, resulting that the two hormonal components are two distinct and alternative strategies to stress [29]. Posttraumatic stress disorder (PTSD) is associated with disturbances of the hypothalamus--pituitary--adrenal (HPA) axis, but also of hypothalamus--pituitary--thyroid pathway [28]. The studies conducted in PTSD patients indicate that a series of plasmatic hormones, including cortisol, prolactin, thyrotropin and free thyrotoxin have significantly decreased levels, compared with healthy subjects [28]. Recently, another group of researchers has evaluated the predictive factors resulting from the reactivity of HPA axis in PTSD patients and healthy subjects. The results of dexamethasone test demonstrated a hypersuppression of cortisol concentration and a significant decrease of plasma prolactin in patients [27]. Expert Opin. Drug Metab. Toxicol. [Early Online] 5 V. Voicu et al. Table 1. Clinical consequences of hyperprolactinemia. Gender Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. General characteristics Consequences Male Female Hypogonadism Erectile dysfunction Diminished ejaculate volume Oligospermia Delayed puberty Decreased libido Decreased bone mineral density [107] Rarely: gynecomastia, galactorrhea (approx. 20%) Possible increased incidence of breast cancer Hypogonadism Breast volume increase Galactorrhea Increased risk of breast cancer Ovarian dysfunction Infertility Decreased libido Atrophy of the urethral and vaginal mucosa Decreased bone mineral density [107] Decreased vaginal lubrication and dyspareunia Acne and possible hirsutism Possible consequences: hostility, anxiety, depression, all of medium intensity [19] In subjects with a diagnostic of first episode of psychoses (bipolar or depressive), the pituitary volume is increased, according to the MRI scans [30]. The increase was obvious in the case of first episode of schizophrenia. The explanation resides on the hyperactivity of the HPA axis, as the answer of the main neurohormonal system to stress. The authors mentioned that the subjects without antipsychotic treatment or under treatment with atypical antipsychotics have a similar increase of the pituitary volume, whereas typical antipsychotics seem to induce a more pronounced increase. They concluded that, on one hand, this increase of pituitary volume is independent on the antipsychotic effect; on the other hand, the typical antipsychotics induce an adjacent increase, consecutive to the activation of lactotroph cells. Hyperprolactinemic effects of drugs The analysis of the effects of some drugs and/or xenobiotics on prolactin secretion needs a description of their pattern, pharmacokinetic (PK) and PD mechanism and consequences on the therapeutic strategy for selected drugs used in the treatment of chronic diseases, for example, schizophrenia or depressive syndrome. Tables 2 and 3 illustrate a synthesis of the available data, classifying the compounds generating hypo- and hyperprolactinemia according to their pharmacotherapeutic class, mechanism of action and therapeutic indication. Some general characteristics correlated with clinical and therapeutic consequences must be emphasized. Thus, the hyperprolactinemic domain is obviously important and relevant for the clinical consequences and, implicitly, the measures for prevention of major effects of hyperprolactinemia, especially since long-term administration is needed in several instances (antipsychotics, antidepressants, antihypertensives, prokinetics). It results that the main therapeutic group producing hyperprolactinemia is represented by the typical (first-generation) antipsychotics, but also by some atypical antipsychotics (especially risperidone, paliperidone and amisulpride). Olanzapine can generate hyperprolactinemia at high doses. The firstgeneration antidepressants are considered hyperprolactinemic 4.2. 6 agents of short duration. All selective serotonin reuptake inhibitor (SSRI) antidepressant drugs have been associated with hyperprolactinemic effects [31]. Beside the risk of breast cancer, the long-term complication of hyperprolactinemia is the decrease of bone density, reported especially in women, but also in men. Noteworthy, even after correction of hyperprolactinemia or transitory hyperprolactinemia, the osteopenia persists [32]. The drug-induced hyperprolactinemia and its consequences impose both clinical and laboratory diagnostic, especially in schizophrenic patients under treatment with antipsychotics. In this context, either the decrease of the dose, the therapy switching to aripiprazole (as an example, due to its partial antagonist effect on dopamine D2 receptors) or adjuvant therapy for correction of sexual dysfunction (phosphodiesterase inhibitors) should be initiated [33]. Although several authors suggest that hyperprolactinemia is an important adverse effect of the antipsychotic treatment, this is generally neglected [34]. Recent data indicate that hyperprolactinemia represents a risk factor not only for the breast cancer, but also for prostate cancer [35]. Experimental, clinical and epidemiological studies suggest that hyperprolactinemia is associated with breast cancer [35]. Emerging proofs also support a relationship between hyperprolactinemia and prostate carcinogenesis. Currently, there are recommendations for evaluation of these aspects, as part of both regulatory and clinical toxicology, in high-risk patients under treatment with hyperprolactinemic drugs [35]. The increase of prolactin secretion induced by SSRI drugs is correlated with the serotoninergic mechanisms involved in the generation of specific antidepressant effects. These drugs have as common mechanism the inhibition of serotonin reuptake, therefore increasing the availability of the neurotransmitter at the level of the corresponding synapses (Figure 1 and Table 3) [31]. Antipsychotic-induced hyperprolactinemia A series of clinical data suggest that the hyperprolactinemic effects in patients treated with antipsychotic drugs could be at least underestimated, if not neglected, for several reasons 4.3. Expert Opin. Drug Metab. Toxicol. [Early Online] Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences Table 2. Drugs with inhibitory activity on the prolactin secretion. PD class Dopamine antagonists Bromocriptine Pergolide Cabergoline Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. L-DOPA Effect on prolactin Mechanism of action Intense decrease, short duration Intense decrease, medium duration Intense decrease, long duration Decrease, short duration D2 R agonist Therapeutic use D2 R agonist Antiparkinsonian, treatment of hyperprolactinemia Antiparkinsonian, off-label treatment of hyperprolactinemia Treatment of hyperprolactinemia Dopamine precursor Antiparkinsonian D1 R and D2 R agonist Parasympathomimetics Pilocarpine Physostigmine Cocaine Increase Stimulation of muscarinic R Obsolete Decrease Release of catechol amines, blocking of reuptake Local anesthetic Serotonin antagonists Cyproheptadine Decrease 5-HT2A R antagonist, H1 R antagonist, antimuscarinic Antihistamine, serotonin syndrome, etc. Opioid antagonists Naloxone Decrease PD: Pharmacodynamic. Data from [84,105,106,108]. linked to patient, physician, associated medication, psychopathological aspects or environmental factors [36]. The atypical antipsychotics generate much reduced or no effects, excepting risperidone and amisulpride. In a recent review, the authors have emphasized on the similar profile of the 9-hydroxy metabolite of risperidone (paliperidone) [37,38]. Among other secondgeneration antipsychotics, amisulpride, risperidone and paliperidone have hyperprolactinemic effects comparable with those reported for the first generation [39]. It is estimated that risperidone, paliperidone and amisulpride have superior hyperprolactinemic effects compared with haloperidol [40-42]. By contrast, quetiapine and clozapine do not induce hyperprolactinemic effects, whereas aripiprazole can induce a decrease of prolactin levels, also at high doses [43]. The hyperprolactinemic effects of risperidone are dose-dependent [42,44,45]. In case of amisulpride administered in doses of 630 -- 910 mg [46], the decline of initially high prolactin levels during a long-term treatment, was explained by an up-regulation of dopamine D2 receptors, following a prolonged blockade. The decreasing levels of prolactin on the time course of treatment and their normalization after discontinuation has been considered a proof of lack of persistent modification of neuroendocrine mechanisms, but additional, adaptive changes could also be involved [46]. Pharmacokinetic and pharmacodynamic particularities of antipsychotics and consequences on prolactin secretion 5. A recent analysis of the consequences of antidopaminergic activity in case of antipsychotics on the prolactin secretion underlines, beside the differences between the two types (typical and atypical), a series of other determinants of antipsychotics and other drugs with antidopaminergic action on the considered hormone [47]. The affinity ratio for serotonin (5-HT2) and dopamine (D2) receptors is discussed. Another determinant factor, focusing on the distinct effects within the atypical antipsychotic drugs, is correlated with differences in the transport (permeability) through the BBB. Obviously, the entities not penetrating BBB or not reaching a sufficient concentration at the level of target structures in the CNS do not generate effects on the cerebral function. The relative low penetration by some compounds requests high doses in order to generate an occupancy of central D2 receptors, therefore leading to an increased occupancy in periphery (anterior hypophysis) and an increase in prolactin secretion [37,48,47]. The biotransformation of several neuropsychotropic generates more hydrophilic metabolites with decreased BBB penetration and, in some instances, distinct PD properties [37], which can be better evaluated by PK--PD correlations, including both parent drugs and active metabolites. In this direction, it is relevant, for example, that the ratio of affinities for serotonin 5-HT2 and dopamine D2 receptors is highly different for active metabolites, compared with the parent drug [37,49]. It is the case of 9-hydroxy risperidone which, as a new pharmacologically active entity, has been subject to extensive analysis of molecular descriptors defining the ‘physico-chemical properties space’ [37,50,51]. It results that the mentioned active metabolite is characterized by a decreased lipophilicity (as estimated by the partition coefficient in n-octanol/ water binary systems, logKow), implicitly increased hydrophilicity, decreased DlogP (difference in logP evaluated in n-octanol and cyclohexane/water binary systems), increased hydrogen bonding ability (HBD), increased polar surface area (PSA), decreased membrane permeability. Expert Opin. Drug Metab. Toxicol. [Early Online] 7 V. Voicu et al. Table 3. Drugs with stimulatory activity on the prolactin secretion. Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. PD class Antipsychotics (typical and atypical) phenothiazines butyrophenones (haloperidol) risperidone, paliperidone amisulpride molindone zotepine Antidepressants imipramine desimipramine amitriptyline clomipramine paroxetine, fluoxetine, citalopram, fluvoxamine (SSRI) MAO inhibitors (pergoline, tranylcypromine) Digestive prokinetics metoclopramide domperidone Opiates and opioids morphine spiradoline methadone Amphetamines (amphetamine-like) fenfluramine Antihypertensive calcium channel blockers (verapamil) methyldopa neurosympatholytic (reserpine) Effect on prolactin Mechanism of action Therapeutic use Chronic increase D2 R antagonist D2 R and 5-HT2 R antagonist Treatment of schizophrenia Increase, short duration Increased availability of serotonin, by blocking the reuptake Treatment of depressive syndrome Stimulation, short duration moderate stimulation D2 R antagonist D2 R peripheral antagonist Antiemetic, prokinetic prokinetic Stimulation, short duration moderate stimulation chronic moderate stimulation µ R agonist k R agonist µ R agonist Central anesthetic and treatment of substitution Intense, short stimulation Increased release and inhibition of serotonin reuptake Recreational drugs, drugs of abuse Chronic stimulation chronic, moderate stimulation Calcium channel blockers decrease of sympathetic tonus by false mediator (a-methyldopa) catecholamine depletion Antihypertensive, antiarrhythmic antihypertensive antihypertensive (obsolete) PD: Pharmacodynamic; SSRI: Selective serotonin reuptake inhibitor. Data from [105,106,108,84]. The brain/plasma ratio for 9-hydroxy risperidone drops five times compared with the parent drug, generating a logBB value (logarithm of the brain/plasma ratio) of - 0.67 and - 0.02, respectively [52-54]. The comparison with domperidone, unanimously considered to act outside CNS, could be suggestive, since logBB is - 0.78, static and dynamic PSA are 68 and 57 Å2, respectively [55]. Noteworthy, the logP for domperidone is 3.9, indicating an optimal value for BBB penetration [56]. Domperidone is a dopamine antagonist of peripheral D2 receptors, having digestive prokinetic effects (acceleration of gastric emptying, increase of the motor activity of esophagus, increase of antral-duodenal contractions). It is assumed that, although in very small concentrations, domperidone penetrates BBB. The antiemetic effects, generated by acting at the level of the chemoreceptor trigger zone in the IV ventricle, although manifested on some cerebral mechanisms, are placed outside BBB. Most probably, the antiemetic and prokinetic effects contribute synergistically to the central one (at the level of the trigger zone) in generating the specific 8 effect [57-59]. On the other hand, risperidone has dynamic and static PSA of 57 and 74 Å2, respectively, while the 9-hydroxy metabolite, 45 and 62 Å2. The optimal interval of PSA for CNS activity is 60 -- 70 Å2. The drop in PSA is reflected by the decreased logBB value for the metabolite. An important aspect which must be considered is the unbound fraction of the considered compound. The binding profile to plasma protein is correlated with the lipophilicity, which is decreased for the metabolite, if considering risperidone and its 9-hydroxy-derivative. Finally, as a consequence of hydroxylation, the 9-hydroxy metabolite has a lower affinity for both serotonin 5-HT2 and dopamine D2 receptors, compared with the parent drug [60,61]. On human cloned D2 receptors, the dissociation half-life for 9-hydroxy risperidone is 1 min, while for risperidone is 27 min. The hyperprolactinemic effects of the antipsychotic drugs become relevant approximately 10 h after the initiation of treatment, with levels of prolactin almost 10 times higher, compared with the basal level [19]. After intravenous Expert Opin. Drug Metab. Toxicol. [Early Online] Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences administration of amisulpride of two dose strengths, 20 and 100 mg, respectively, comparable maximum concentrations of prolactin were reached in 15 -- 30 min, detectable levels being maintained for 7 h [62]. Two aspects are essential. On one hand, the hyperprolactinemia induced by several antipsychotics is correlated with their concentration. For risperidone, this correlation is valid in adults, since age-specific patterns have been described for children and adolescents, as a result of difference in neurotransmitter systems, number of lactotroph cells or sensitivity to hyperprolactinemiants [63]. On the other hand, the concentration level is determined by the dose necessary to induce the central antipsychotic effect. The plasma concentration generates a gradient controlling the BBB penetration (if only the passive diffusion processes are considered) and achievement of the active concentration at the level of cerebral receptors (dopaminergic D2, serotoninergic 5-HT2, cholinergic, etc.). The relationship between the mentioned determinants and BBB permeability is characterized by the ratio of the concentrations in brain and blood, that is, logBB. Finally, the necessary concentration of the antipsychotic in the biophase of the cerebral receptors is determined by its affinity. For amisulpride, the hydrophilic character and low fraction unbound to plasma protein were mentioned as the main determinants for preferential distribution outside BBB [64]. Therefore, this specific PK profile, combined with the high affinity for dopamine D2 receptors, could account for the marked hyperprolactinemic effect. In fact, the mean efficient dose and the occupancy half-life for each antipsychotic and receptor reveal the affinity for the considered type of receptor. It is a very well-known fact that, beside partition coefficient (logP), a series of molecular descriptors, that is, PSA, molecular volume, plasma protein binding or distribution coefficient (logD), determine the penetration of BBB (logBB), but implicitly, the resulting hyperprolactinemic effects. Although molecular determinants mentioned above have been correlated with passive diffusion processes, the interplay of P-glycoprotein (P-gp) alters considerably ratio of brain to blood concentration, some reports suggesting a possible influence on the rate of non-responders to antipsychotic therapy [65]. Noteworthy, lipophilicity, the presence of at least one nitrogen atom ionized at the physiological pH and a rather narrow interval of variation for the molecular weight seems to describe the modulators of P-gp [66]. Several antipsychotic drugs, for example, haloperidol, quetiapine, olanzapine and clozapine are weak or no substrate for P-gp, but display inhibitory activity on this efflux transporters [66,67]. Of particular importance is the fact that, while several antipsychotics are inhibitors of P-gp (risperidone, clozapine), their active metabolites generated in vivo by different biotransformation pathways are substrates of P-gp, that is, paliperidone [37,68] and N-desmethyl-clozapine [67]. It concerns the switching to prolactin-sparing antipsychotics, it should be mentioned that both aripiprazole and its active metabolite dehydro metabolite are substrates of P-gp [69]. Potential clinically relevant drug--drug interaction should be considered in case of hyperprolactinemic agents such as haloperidol, risperidone or amisulpride, the later one being both inhibitor and substrate of P-gp [70]. In the authors’ opinion, a useful approach should consider three distinct parameters that, according to available data, are correlated with the hyperprolactinemic effect of antipsychotic drugs: the affinity for dopamine D2 receptors, the half-life of occupancy and the distribution through BBB, estimated by logBB. Decreased affinities and shorter occupancy (1/ED50) are correlated with a lower incidence of hyperprolactinemic effects (decreasing from risperidone to aripiprazole) [71-73]. As mentioned previously, amisulpride and risperidone induce the most intense effects. Based on estimated or experimental data, a reverse correlation has been suggested between logBB of some antipsychotics and their induced hyperprolactinemic effect. The affinity of antipsychotics for dopamine D2 receptors, compared with the affinity for dopamine, is relevant for the incidence of hyperprolactinemic effects, but also of the extrapyramidal effects, although generated in another cerebral area [74]. Moreover, there is a continuous search of the psychiatrists and psychopharmacologists for criteria that distinguish between the ability to induce not only the specific clinical efficacy, but also the presence or absence of some adverse effects, including the extrapyramidal or hyperprolactinemic effects [75]. Notable hyperprolactinemic effects with significant clinical consequences impose the switch to another antipsychotic therapy which reduces or exhibits no hyperprolactinemic effects. Another key aspect should be discussed, which correlates well with the previously presented facts, the tardive dyskinesia. It is assumed that tardive dyskinesia is just an indicator of an ample dysfunction, the dopaminergic neurotransmission, a pandopaminergic dysfunctional state which may appear in patients with or without antipsychotic treatment [76]. Nevertheless, it seems like there is a correlation between tardive dyskinesia and deviation of the neuroendocrine answer to hyperprolactinemia. The minority at risk to develop tardive dyskinesia has also a high risk to develop sexual dysfunctions correlated with the hypersecretion of prolactin (prolactinrelated sexual disturbances). Notably, the hyperprolactinemic effects are consecutive to the interaction of antipsychotics with dopamine D2 receptors at the level of the lactotroph cells, outside BBB, while tardive dyskinesia is a consequence of the interaction at the central level. Possibly, tardive dyskinesia and sexual disturbances are two distinct manifestations, with a common support, that is the pandopaminergic dysfunction characteristic of schizophrenia [76-78]. In the past, the secondary motor effects of antipsychotics were correlated with the hyperprolactinemic effects, both being generated by the interaction with dopamine D2 receptors. The significant difference resides on the fact that the extrapyramidal effects are consequences of blocking of striatal dopamine D2 receptors, whereas hyperprolactinemia is consecutive to the blockage in the anterior hypophysis [49]. Expert Opin. Drug Metab. Toxicol. [Early Online] 9 Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. V. Voicu et al. The ratio of brain to plasma concentrations of antipsychotics is a determinant for hyperprolactinemia. There is a reverse dependence, the highest the ratio, the lowest the level of prolactin, in relation with the targeted antipsychotic effect. The authors have demonstrated a reverse dependence between the hyperprolactinemic effect of some antipsychotics and logBB value [37,79]. In order to obtain a specific effect for a compound with low BBB permeability, an increased plasma level is required, generating an increased incidence of the hyperprolactinemic effects, correlated with the occupancy of dopamine D2 receptors in the anterior hypophysis (1/ED50) and with the affinity (1/Ki) and the dissociation rate (t1/2). The analysis of the model for agonist--antagonist interaction and release of prolactin after the administration of risperidone and paliperidone emphasize a similar potency for the two antipsychotics for the release of prolactin [38]. It is interesting to note that the metabolite has a distinct profile of affinities for serotonin 5-HT2 versus dopamine D2 receptors [49], but also distinct half-life of dissociation. 6. Expert opinion As it results from the analysis of the clinical consequences of hyperprolactinemia in humans, a key aspect is the accurate monitoring of the treatment with hyperprolactinemic drugs. Depending on the causal agent (pharmacological, toxicological or pathological), a strategy of hyperprolactinemia management is to be defined. In the case of an antipsychotic treatment, with relevant hyperprolactinemic effects on plasma levels (higher than 100 ng/ml) and symptoms, several issues must be discussed. The most important aspect is the switching between the hyperprolactinemic agent (amisulpride, risperidone) and olanzapine, quetiapine, clozapine or aripiprazole. Apparently, the switching is a simple procedure. In reality, this is not easy to be accomplished if an adequate antipsychotic outcome has been obtained. The switching to another antipsychotic can generate an unsatisfactory outcome or another type of adverse effects [80]. It is considered that matching a specific antipsychotic medication for a specific patient is a substantial challenge [81,82]. In this context, adjunctive treatment with aripiprazole for antipsychotic-induced hyperprolactinemia represents an adequate therapeutic solution, with restoration of normal values for prolactin and reversal of consequent clinical symptoms [83]. There were some attempts to associate risperidone and aripiprazole, with significant results on the hyperprolactinemia generated by the first antipsychotic [84,85]. Reversal of paliperidone-induced hyperprolactinemia was also reported [86]. The PK particularities of amisulpride, especially the hydrophilicity-driven distribution outside BBB, administered in high doses (1000 mg) could explain why addition of aripiprazole, a highly lipophilic, high affinity agonist/antagonist of dopamine D2 receptors doesn’t seem to lower the prolactin levels [64]. The dose of hyperprolactinemic agent could be the 10 key factor, since there is a report of association between 200 -- 300 mg amisulpride and 10 -- 15 mg aripiprazole leading to decreased prolactin concentration [87]. In the case of hyperprolactinemia in patients with antidepressant treatment, the switch with another agent is recommended. The treatment with other hypoprolactinemiant (dopaminergic) drugs, for example, cabergoline, bromocriptine, etc. is generally not recommended, the outcome being controversial. The main reason is the worsening of psychotic symptoms [88]. The single, partial agonist of dopamine with significant results in both switching of the hyperprolactinemic antipsychotic or temporary association is aripiprazole [34,89]. In the previously mentioned context or for normalization of prolactin levels, one could admit that the effects of the association of the hyperprolactinemic antipsychotic and aripiprazole are consequences of their PD antagonism at the level of dopamine D2 receptors [81], but this approach requests a broader discussion. The above-mentioned dopaminergic compounds preserve the therapeutic significance in prolactinomas and idiopathic hyperprolactinemia, that is, they normalize the plasma prolactin level, improve the clinical symptomatology and reduce the volume of prolactinomas [90,91]. In this context, cabergoline is preferred to bromocriptine, based on the higher rate of success and on the reduced incidence of adverse effects [90,91]. The hyperprolactinemia induced by different classes of drugs, particularly those administered chronically, has clinically significant consequences, such as sexual dysfunction in both genders, breast or prostate cancer and low bone mineral density. Therefore, accurate monitoring and evaluation of the hyperprolactinemia induced by some drugs appears as a necessity, imposing a strategy for the management of this type of disturbance. The typical antipsychotics and some of the atypical agents (amisulpride, risperidone, paliperidone), but also some antidepressants, antihypertensives and prokinetics, are the most important classes of drugs that generate hyperprolactinemia. Based on available recommendation [92,93], regular assessment of possible sexual dysfunction must be performed. Whenever available, prolactin levels should be determined at baseline. The level and duration of hyperprolactinemic effects are of particular importance. Mild elevation, persisting for > 3 months should determine either a dose reduction of incriminated hyperprolactinemc agent or switching to a prolactin-spearing one. The switching is usually recommended by persistent prolactin levels above the threshold of 50 ng/ml [92]. Particularly for men experiencing sexual dysfunction induced by hyperprolactinemia, levels higher than 17 ng/ml has been proposed for identification of patients benefiting from switching to prolactin-spearing antipsychotics [94]. In case of prolactin levels above 200 ng/ml or if lateral visual deficits are concluded [92], screening of prolactinoma should be performed [95]. Evaluation of bone mineral density must be implemented if hypogonadism associated with hyperprolactinemia was identified. Specifically for the procedures involving the switching to aripiprazole, there are several case reports of worsening Expert Opin. Drug Metab. Toxicol. [Early Online] Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences psychosis [96-99]. It has been suggested that this particular feature may be related to the previously described, unique receptor binding profile of aripiprazole, that is, partial agonist of dopamine D2/D3 receptors, partial agonist of serotonin 5-HT1A receptors [100]. The agonistic/antagonistic profile of aripiprazole is receptor reserve-dependent [101]. An up-regulation of dopamine receptors in the areas of intense and prolonged blockage has been correlated with increased sensitivity to dopamine, phenomenon described as the ‘neuroleptic-induced supersensitivity psychosis’ [102,103]. The hyperprolactinemic effects of antipsychotics and other drugs are correlated with their affinity for dopamine D2 receptors, their BBB penetration and, implicitly, the necessary dose for an adequate occupancy of cerebral D2 receptors. The penetrability is a complex resultant of several molecular descriptors (partition or distribution coefficient, PSA, molecular Bibliography Papers of special note have been highlighted as either of interest () or of considerable interest () to readers. 1. Holt RI. Medical causes and consequences of hyperprolactinaemia. A context for psychiatrists. J Psychopharmacol 2008;22:28-37 2. Goffin V, Binart N, Touraine P, et al. Prolactin: the new biology of an old hormone. Annu Rev Physiol 2002;64:47-67 3. 4. 5. .. 6. .. 7. 8. Sinha YN. Structural variants of prolactin: occurrence and physiological significance. Endocr Rev 1995;16(3):354-69 Bernichtein S, Touraine P, Goffin V. New concepts in prolactin biology. J Endocrinol 2010;206:1-11 Ben-Jonathan N, LaPensee CR. Prolactin and its neuroendocrine control. In: Larry RS, editors. Encyclopedia of Neuroscience. Academic Press, Oxford; 2009. 1125-31 Clementi G, Nicoletti F, Patacchioli F, et al. Hypoprolactinemic action of calcitonin and the tuberoinfundibular Declaration of Interest The authors declare no conflict of interest and have received no payment in the preparation of their manuscript. dopaminergic system. J Neurochem 1983;40:885-6 9. Kanyicska B, Lerant A, Freeman ME. Endothelin is an autocrine regulator of prolactin secretion. Endocrinology 1998;139:5164-73 10. Apud JA, Cocchi D, Locatelli V, et al. Biochemical and functional aspects on the control of prolactin release by the hypothalamo-pituitary GABAergic system. Psychoneuroendocrinology 1989;14:3-17 11. 12. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev 2000;80:1523-631 Comprehensive review of functions and control of prolactin secretion. Ben-Jonathan N, Hnasko R. Dopamine as a prolactin (PRL) inhibitor. Endocr Rev 2001;22:724-63 Review of the role of dopamine and of the interplay of several endobiotics on prolactin secretion. weight, HBD, etc.), accurately defined by logBB [37,61,104]. For some antipsychotics and domperidone, a reverse correlation can be concluded between logBB and the hyperprolactinemic effects. The comparative analysis of the hyperprolactinemic effects of several antipsychotics, typical or atypical, in close relation with their affinity for dopamine D2 receptors, their occupancy half-life and the values of the molecular descriptors, determinant for logBB, allows, in the authors’ opinion, a good prediction of their potential to induce hyperprolactinemia and exhibits increased potential in the screening for new molecular entities [37,104]. 13. 14. .. 15. Mukherjee A, Snyder G, McCann SM. Characterization of muscarinic cholinergic receptors on intact rat anterior pituitary cells. Life Sci 1980;27:475-82 Carmeliet P, Denef C. Immunocytochemical and pharmacological evidence for an intrinsic cholinomimetic system modulating prolactin and growth hormone release in rat pituitary. Endocrinology 1988;123:1128-39 Ben-Jonathan N, Chen S, Dunckley JA, et al. Estrogen receptor-alpha mediates the epidermal growth factor-stimulated prolactin expression and release in lactotrophs. Endocrinology 2009;150:795-802 Brooks CL. Molecular mechanisms of prolactin and its receptor. Endocr Rev 2012;33:504-25 Comprehensive presentation of molecular mechanisms of prolactin. Nicoll CS, Mayer GL, Russell SM. Structural features of prolactins and growth hormones that can be related to Expert Opin. Drug Metab. Toxicol. [Early Online] their biological properties. Endocr Rev 1986;7:169-203 16. Bole-Feysot C, Goffin V, Edery M, et al. Prolactin (PRL) and its receptor: actions, signal transduction pathways and phenotypes observed in PRL receptor knockout mice. Endocr Rev 1998;19:225-68 17. Perks CM, Keith AJ, Goodhew KL, et al. Prolactin acts as a potent survival factor for human breast cancer cell lines. Br J Cancer 2004;91:305-11 Demonstration of the role of prolactin in survival of human breast cancer cell lines. . 18. Clevenger CV, Furth PA, Hankinson SE, Schuler LA. The role of prolactin in mammary carcinoma. Endocr Rev 2003;24:1-27 19. Wieck A, Haddad PM. Antipsychotic-induced hyperprolactinaemia in women: pathophysiology, severity and consequences. Selective literature review. Br J Psychiatry 2003;182:199-204 Review of the clinical consequences of hyperprolactinemia in women. .. 20. Haga Y, Iwanaga Y, Matsumura F, et al. Curatively resected primary malignant melanoma of the esophagus: report of a case. Surg Today 1993;23:820-4 21. Bushe CJ, Bradley AJ, Wildgust HJ, et al. Schizophrenia and breast cancer incidence: a systematic review of clinical studies. Schizophr Res 2009;114:6-16 22. Dekkers OM, Romijn JA, de Boer A, et al. The risk for breast cancer is not evidently increased in women with 11 V. Voicu et al. hyperprolactinemia. Pituitary 2010;13:195-8 23. Peuskens J, Sienaert P, De Hert M. Sexual dysfunction: the unspoken side effect of antipsychotics. Eur Psychiatry 1998(13):23s-30s 24. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry 2004;161:1324-33 25. Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. 26. 27. 28. . 29. 30. 31. 32. 12 Shibli-Rahhal A, Schlechte J. The effects of hyperprolactinemia on bone and fat. Pituitary 2009;12:96-104 Asai-Sato M, Okamoto M, Endo M, et al. Hypoadiponectinemia in lean lactating women: prolactin inhibits adiponectin secretion from human adipocytes. Endocr J 2006;53:555-62 Frih H, Sahraoui L, Frih N, et al. Facteurs prédictifs de la survenue du stress post-traumatique chez des individus ayant vécu deux évènements de vie majeurs (tremblement de terre et terrorisme en Algérie): réponse corticotrope et prolactinique à une faible dose de dexaméthasone (0.50 mg). L’Évolution Psychiatrique 2009;74:581-91 Olff M, Guzelcan Y, de Vries GJ, et al. HPA- and HPT-axis alterations in chronic posttraumatic stress disorder. Psychoneuroendocrinology 2006;31:1220-30 Description of changes of HPA and HPT axis induced by PTSD and of consequences on prolactin levels. Nunes LV, Moreira HC, Razzouk D, et al. Strategies for the treatment of antipsychotic-induced sexual dysfunction and/or hyperprolactinemia among patients of the schizophrenia spectrum: a review. J Sex Marital Ther 2012;38:281-301 Paper on the management of sexual dysfunction and of hyperprolactinemia reported during the treatment with antipsychotics. 42. Roke Y, van Harten PN, Boot AM, et al. Antipsychotic medication in children and adolescents: a descriptive review of the effects on prolactin level and associated side effects. J Child Adolesc Psychopharmacol 2009;19:403-14 43. Haddad PM, Sharma SG. Adverse effects of atypical antipsychotics: differential risk and clinical implications. CNS Drugs 2007;21:911-36 34. Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1978-81 44. Anderson GM, Scahill L, McCracken JT, et al. Effects of short- and long-term risperidone treatment on prolactin levels in children with autism. Biol Psychiatry 2007;61:545-50 45. 35. Harvey PW, Everett DJ, Springall CJ. Hyperprolactinaemia as an adverse effect in regulatory and clinical toxicology: role in breast and prostate cancer. Hum Exp Toxicol 2006;25:395-404 Presentation of toxicological perspective on hyperprolactinemia. Findling RL, Kusumakar V, Daneman D, et al. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry 2003;64:1362-9 46. Schlosser R, Grunder G, Anghelescu I, et al. Long-term effects of the substituted benzamide derivative amisulpride on baseline and stimulated prolactin levels. Neuropsychobiology 2002;46:33-40 47. Fitzgerald P, Dinan TG. Prolactin and dopamine: what is the connection? A review article. J Psychopharmacol 2008;22:12-19 48. Voicu VA, Medvedovici AV, Miron DS, et al. A novel approach on pharmacokinetic/pharmacodynamic correlations of risperidone: understanding its safety and efficacy profiles. Acta Endocrinologica (Buc) 2010;6:265-85 49. Natesan S, Reckless GE, Nobrega JN, et al. Dissociation between in vivo occupancy and functional antagonism of dopamine D2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 2006;31:1854-63 50. van de Waterbeemd H, Smith DA, Beaumont K, et al. Property-based design: optimization of drug absorption and pharmacokinetics. J Med Chem 2001;44:1313-33 Excellent presentation of the role of lipophilicity in the biological fate of xenobiotics. 33. . . 36. Murthy S, Wylie KR. Sexual problems in patients on antipsychotic medication. Sex Relationship Ther 2007;22:97-107 37. Voicu VA, de Leon J, Medvedovici AV, et al. New insights on the consequences of biotransformation processes on the distribution and pharmacodynamic profiles of some neuropsychotropic drugs. Eur Neuropsychopharmacol 2012;22:319-29 38. Sobrinho LG. Prolactin, psychological stress and environment in humans: adaptation and maladaptation. Pituitary 2003;6:35-9 Pariante CM, Dazzan P, Danese A, et al. Increased pituitary volume in antipsychotic-free and antipsychotic-treated patients of the AEsop first-onset psychosis study. Neuropsychopharmacology 2005;30:1923-31 Emiliano AB, Fudge JL. From galactorrhea to osteopenia: rethinking serotonin-prolactin interactions. Neuropsychopharmacology 2004;29:833-46 Schlechte J, Dolan K, Sherman B, et al. The natural history of untreated hyperprolactinemia: a prospective analysis. J Clin Endocrinol Metab 1989;68:412-18 Friberg LE, Vermeulen AM, Petersson KJ, et al. An agonist-antagonist interaction model for prolactin release following risperidone and paliperidone treatment. Clin Pharmacol Ther 2009;85:409-17 39. Miyamoto S, Miyake N, Jarskog LF, et al. Pharmacological treatment of schizophrenia: a critical review of the pharmacology and clinical effects of current and future therapeutic agents. Mol Psychiatry 2012;17:1206-27 40. Buchanan RW, Kreyenbuhl J, Kelly DL, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull 2010;36:71-93 41. Malik P, Kemmler G, Hummer M, et al. Sexual dysfunction in first-episode schizophrenia patients: results from European First Episode Schizophrenia Trial. J Clin Psychopharmacol 2011;31:274-80 Expert Opin. Drug Metab. Toxicol. [Early Online] . 51. van de Waterbeemd H, Smith DA, Jones BC. Lipophilicity in PK design: methyl, ethyl, futile. J Comput Aided Mol Des 2001;15:273-86 Drug-induced hypo- and hyperprolactinemia: mechanisms, clinical and therapeutic consequences 52. 53. Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. . 54. 55. . Arakawa R, Ito H, Takano A, et al. Dose-finding study of paliperidone ER based on striatal and extrastriatal dopamine D2 receptor occupancy in patients with schizophrenia. Psychopharmacology (Berl) 2008;197:229-35 Olsen CK, Brennum LT, Kreilgaard M. Using pharmacokineticpharmacodynamic modelling as a tool for prediction of therapeutic effective plasma levels of antipsychotics. Eur J Pharmacol 2008;584:318-27 Key article on the role of PK--PD modeling in the development of new antipsychotic entities. Kelder J, Grootenhuis PJ, Bayada D, et al. Polar molecular surface as a dominating determinant for oral absorption and brain penetration of drugs. Pharm Res 1999;16:1514-19 Presentation of the biopharmaceutical consequences of PSA. Sunderland T, Cohen BM. Blood to brain distribution of neuroleptics. Psychiatry Res 1987;20:299-305 57. Champion MC, Hartnett M, Yen M. Domperidone, a new dopamine antagonist. CMAJ 1986;135:457-61 58. Friedman G. The GI drug column. Subcommittee on FDA related matters, American College of Gastroenterology. Am J Gastroenterol 1983;78:47-8 Reddymasu SC, Soykan I, McCallum RW. Domperidone: review of pharmacology and clinical applications in gastroenterology. Am J Gastroenterol 2007;102:2036-45 60. Pardridge WM. Brain drug development and brain drug targeting. Pharm Res 2007;24:1729-32 61. Seeman P. An update of fast-off dopamine D2 atypical antipsychotics. Am J Psychiatry 2005;162:1984-5 Letter to editor specifying the relationship between transient occupation/fast dissociation of antipsychotics from dopamine D2 receptors and normal levels of prolactin. . 62. 63. 64. 65. Zhang L, Zhu H, Oprea TI, et al. QSAR modeling of the blood-brain barrier permeability for diverse organic compounds. Pharm Res 2008;25:1902-14 56. 59. receptors by amisulpride: effects on hormone secretion in healthy volunteers. J Psychiatr Res 1994;28:461-73 Wetzel H, Wiesner J, Hiemke C, et al. Acute antagonism of dopamine D2-like 66. 67. 68. 69. 70. 71. Duval F, Guillon MS, Mokrani MC, et al. Relationship between prolactin secretion, and plasma risperidone and 9-hydroxyrisperidone concentrations in adolescents with schizophreniform disorder. Psychoneuroendocrinology 2008;33:255-9 . treatment-pharmacological mechanisms. Pharmacol Ther 2010;125(1):169-79 Critical analysis of the mechanisms of antipsychotic-induced metabolic side effects. 72. Psychoactive Drug Screening Program. Available from: pdsp.med.unc.edu/ indexR.html [Last accessed 4 January 2013] 73. Henderson DC, Doraiswamy PM. Prolactin-related and metabolic adverse effects of atypical antipsychotic agents. J Clin Psychiatry 2008;69:32-44 74. Seeman P, Tallerico T. Antipsychotic drugs which elicit little or no parkinsonism bind more loosely than dopamine to brain D2 receptors, yet occupy high levels of these receptors. Mol Psychiatry 1998;3:123-34 75. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63:56-62 76. Tenback DE, van Harten PN, Slooff CJ, et al. Tardive dyskinesia in schizophrenia is associated with prolactin-related sexual disturbances. Neuropsychopharmacology 2006;31:1832-7 77. Aisenberg AC. Coherent view of non-Hodgkin’s lymphoma. J Clin Oncol 1995;13:2656-75 78. Fenton WS, Wyatt RJ, McGlashan TH. Risk factors for spontaneous dyskinesia in schizophrenia. Arch Gen Psychiatry 1994;51:643-50 79. Voicu V, Radulescu FS, Medvedovici A. Toxicological considerations of acetylcholinesterase reactivators. Expert Opin Drug Metab Toxicol 2013;9:31-50 80. Kirschbaum KM, Uhr M, Holthoewer D, et al. Pharmacokinetics of acute and sub-chronic aripiprazole in P-glycoprotein deficient mice. Neuropharmacology 2010;59:474-9 Weiden PJ, Buckley PF. Reducing the burden of side effects during long-term antipsychotic therapy: the role of "switching" medications. J Clin Psychiatry 2007;68:14-23 81. Schmitt U, Abou El-Ela A, Guo LJ, et al. Cyclosporine A (CsA) affects the pharmacodynamics and pharmacokinetics of the atypical antipsychotic amisulpride probably via inhibition of P-glycoprotein (P-gp). J Neural Transm 2006;113:787-801 Volavka J, Citrome L. Oral antipsychotics for the treatment of schizophrenia: heterogeneity in efficacy and tolerability should drive decision-making. Expert Opin Pharmacother 2009;10:1917-28 82. McEvoy JP, Citrome L, Hernandez D, et al. Effectiveness of lurasidone in patients with schizophrenia or schizoaffective disorder switched from other antipsychotics: a randomized, Paulzen M, Grunder G. Amisulpride-induced hyperprolactinaemia is not reversed by addition of aripiprazole. Int J Neuropsychopharmacol 2007;10:149-51 Kirschbaum KM, Henken S, Hiemke C, et al. Pharmacodynamic consequences of P-glycoprotein-dependent pharmacokinetics of risperidone and haloperidol in mice. Behav Brain Res 2008;188:298-303 El Ela AA, Hartter S, Schmitt U, et al. Identification of P-glycoprotein substrates and inhibitors among psychoactive compounds - implications for pharmacokinetics of selected substrates. J Pharm Pharmacol 2004;56:967-75 Schmitt U, Kirschbaum KM, Poller B, et al. In vitro P-glycoprotein efflux inhibition by atypical antipsychotics is in vivo nicely reflected by pharmacodynamic but less by pharmacokinetic changes. Pharmacol Biochem Behav 2012;102:312-20 Doran A, Obach RS, Smith BJ, et al. The impact of P-glycoprotein on the disposition of drugs targeted for indications of the central nervous system: evaluation using the MDR1A/1B knockout mouse model. Drug Metab Dispos 2005;33:165-74 Reynolds GP, Kirk SL. Metabolic side effects of antipsychotic drug Expert Opin. Drug Metab. Toxicol. [Early Online] 13 V. Voicu et al. 6-week, open-label study. J Clin Psychiatry 2013;74(2):170-9 83. 84. Expert Opin. Drug Metab. Toxicol. Downloaded from informahealthcare.com by 188.27.9.12 on 04/22/13 For personal use only. 85. 86. 87. 88. . 89. 90. 91. 92. 14 Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry 2007;164:1404-10 93. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 2011;10:52-77 94. Byerly M, Nakonezny P. A pilot study to determine a prolactin threshold that identifies improved sexual functioning when switching from a prolactin-elevating to a prolactin-neutral antipsychotic. Clin Schizophrenia Related Psychoses 2010;3:209-16 Torre DL, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag 2007;3:929-51 Wahl R, Ostroff R. Reversal of symptomatic hyperprolactinemia by aripiprazole. Am J Psychiatry 2005;162:1542-3 95. Basterreche N, Zumarraga M, Arrue A, et al. Aripiprazole reverses Paliperidone induced hyperprolactinemia. Actas Esp Psiquiatr 2012;40:290-2 Correll CU, Carlson HE. Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. J Am Acad Child Adolesc Psychiatry 2006;45:771-91 96. Mir A, Shivakumar K, Williamson RJ, et al. Change in sexual dysfunction with aripiprazole: a switching or add-on study. J Psychopharmacol 2008;22:244-53 Ramaswamy S, Vijay D, William M, et al. Aripiprazole possibly worsens psychosis. Int Clin Psychopharmacol 2004;19:45-8 97. DeQuardo JR. Worsened agitation with aripiprazole: adverse effect of dopamine partial agonism? J Clin Psychiatry 2004;65:132-3 98. Chiu YH, Chen CH, Lu ML. Worsening psychosis after adding aripiprazole to clozapine. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:291-2 99. Thone J. Worsened agitation and confusion in schizophrenia subsequent to high-dose aripiprazole. J Neuropsychiatry Clin Neurosci 2007;19:481-2 Miller KK. Management of hyperprolactinemia in patients receiving antipsychotics. CNS Spectr 2004;9:28-32 Key article on the management of hyperprolactinemia in antipsychotic therapy. Hoffer ZS, Roth RL, Mathews M. Evidence for the partial dopamine-receptor agonist aripiprazole as a first-line treatment of psychosis in patients with iatrogenic or tumorigenic hyperprolactinemia. Psychosomatics 2009;50:317-24 dos Santos Nunes V, El Dib R, Boguszewski CL, et al. Cabergoline versus bromocriptine in the treatment of hyperprolactinemia: a systematic review of randomized controlled trials and meta-analysis. Pituitary 2011;14:259-65 Wang AT, Mullan RJ, Lane MA, et al. Treatment of hyperprolactinemia: a systematic review and meta-analysis. Syst Rev 2012; published online 24 July 2012; doi:10.1186/ 2046-4053-1-33 De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 2011;10:138-51 100. Kodama M, Hamamura T. Aripiprazole-induced behavioural disturbance related to impulse control in a clinical setting. Int J Neuropsychopharmacol 2010;13:549-51 101. Tadori Y, Forbes RA, McQuade RD, et al. Receptor reserve-dependent properties of antipsychotics at human dopamine D2 receptors. Eur J Pharmacol 2009;607:35-40 102. Steiner W, Laporta M, Chouinard G. Neuroleptic-induced supersensitivity psychosis in patients with bipolar affective disorder. Acta Psychiatr Scand 1990;81:437-40 103. Cousins DA, Young AH. Partial agonists in schizophrenia. Br J Psychiatry 2005;186:354 104. Kapur S, Langlois X, Vinken P, et al. The differential effects of atypical antipsychotics on prolactin elevation are explained by their differential Expert Opin. Drug Metab. Toxicol. [Early Online] blood-brain disposition: a pharmacological analysis in rats. J Pharmacol Exp Ther 2002;302:1129-34 105. Molitch ME. Medication-induced hyperprolactinemia. Mayo Clin Proc 2005;80:1050-7 .. Broad analysis of clinical implication and treatment of drug-induced hyperprolactinemia. 106. Molitch ME. Drugs and prolactin. Pituitary 2008;11:209-18 107. Kishimoto T, De Hert M, Carlson HE, et al. Osteoporosis and fracture risk in people with schizophrenia. Curr Opin Psychiatry 2012;25:415-29 108. Rehm S, Stanislaus DJ, Williams AM. Estrous cycle-dependent histology and review of sex steroid receptor expression in dog reproductive tissues and mammary gland and associated hormone levels. Birth Defects Res B Dev Reprod Toxicol 2007;80:233-45 Affiliation Victor Voicu†1, Andrei Medvedovici2, Aurelian Emil Ranetti3 & Flavian Ştefan Rădulescu4 † Author for correspondence 1 Professor, University of Medicine and Pharmacy Carol Davila, Faculty of Medicine, Department of Clinical Pharmacology, Toxicology and Psychopharmacology, Scoala Floreasca Street #8, Bucharest 011643, Romania E-mail: [email protected] 2 Professor, University of Bucharest, Faculty of Chemistry, Department of Analytical Chemistry, Panduri Avenue # 90, Bucharest 050663, Romania 3 Doctor, Central Universitary Emergency Military Hospital, Department of Endocrinology, Mircea Vulcănescu Street #88, Bucharest 010825, Romania 4 Doctor, University of Medicine and Pharmacy Carol Davila, Faculty of Pharmacy, Department of Drug Industry and Pharmaceutical Biotechnology, Traian Vuia Street # 6, Bucharest 020956, Romania