* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Naloxone - Spirit of Healing: Alberta First Nations Conquering
Survey
Document related concepts
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Neuropharmacology wikipedia , lookup
Transcript
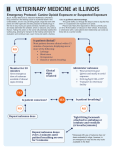
Naloxone NARCAN® What is Naloxone (Narcan®)? Naloxone is an opioid antagonist derived from an opiate alkaloid called thebaine. It is also known by the brand name Narcan®. Naloxone blocks the pharmacological effects of opioid analgesics, and instantly brings on withdrawal. It returns a person who has taken an opioid to a state where opioid effects are not present. Naloxone rapidly reverses opioid overdose effects, including respiratory depression. Naloxone does not work for non-opioid related overdose. 2 Opioid Antagonists Opioid antagonists bind to opioid receptors and are used to block the effects of opioids by blocking the receptor sites to prevent any action of an opioid agonist. Antagonists do not activate receptors, and they prevent receptors from being activated by agonist compounds. An antagonist is like a key that fits in a lock but does not open it and prevents another key from being inserted to open the lock. Physical Appearance Naloxone is a slightly off-white, odorless crystalline substance soluble in water and slightly soluble in alcohol. It is dispensed in liquid form in ampules for purposes of injection. A typical adult dosage is between 0.1 and 2.0 mg, repeated if necessary. Forms of Naloxone There are two forms of Naloxone: ◦ Injectable Naloxone, which is injected directly into the muscle, skin or veins. ◦ Nasal Naloxone, is administered through the nasal cavity (not currently available in Canada) Medical Uses The primary medical use is to reverse respiratory depression and other effects of opioid analgesics such as fentanyl, heroin, morphine, codeine. Naloxone is also used when treating asphyxia in newborn infants whose mothers were treated with opioid analgesics during labour. Naloxone does not lead to overdose. Effects of Short-Term Use: Low Doses Naloxone takes action within 1-2 minutes when given intravenously, and in 2-5 minutes if given subcutaneously or intramuscularly. The duration of its effect depends on the size of dose and route of administration – typically 30-60 minutes. Opioid-dependent individuals will immediately experience withdrawal symptoms very similar to following abrupt cessation of opioid use – except the symptoms appear within minutes and last about two hours. Naloxone Blocks Effects of Opioids If an opioid is taken shortly after naloxone has been taken, the effects of the opioid will be partially or totally blocked. For example, 1 mg of naloxone has been demonstrated to completely block the effects of 25 mg of heroin. Tolerance & Dependence Physical tolerance to Naloxone’s antagonist actions does not develop. However, long-term administration of opioid antagonists such as naloxone increase the density of opioid receptors in the brain and cause temporary exaggeration of responses to subsequent administration of opioid analgesics. Extended use of naloxone will not cause harmful physical or psychological dependence. Can Naloxone be Abused? Naloxone does nothing to a person who has not taken opioids, all it does is block the effects of opioids in the brain and causes individuals that are dependent on opioids to go into instant withdrawal. Naloxone cannot get a person high, and does not promote opioid use. Naloxone is used under medical supervision and is not a drug of abuse. Opioid Overdose Antidote Opioid overdose cause respiratory depression (breathing slows or completely stops), which is reversed by naloxone. For a brief period the patient’s breathing may become more rapid than prior to the overdose. Death, severe brain damage and other harms due to oxygen deprivation during an opioid overdose has been shown to be reduced through overdose education and community-based naloxone programs. Opioid Overdose Opioid overdose is common and one of the major causes of death in addicts. The highest risk time for overdose is in the period after drug use has been discontinued because tolerance to opioid medication is quickly lost. Respiratory depression can also occur from drug overdose. Abusing pain relievers along with other substances such as alcohol, antihistamines, and general anesthetics can increase the chances of respiratory depression. 13 Why Does Overdose Happen? Opioid overdose happens when an opioid user takes more than their body can handle. Opioid overdose can occur for numerous reasons, such as: ◦ When someone takes an opioid drug (e.g. Fentanyl) with a higher concentration might be expected. ◦ When someone misuses or abuses opioids and combines the drug with alcohol or another depressant drug. ◦ When someone returns to opioid use after a period of abstinence and previously acquired tolerance has been lost. Signs of Opioid Overdose ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Person cannot stay awake Can’t talk or walk Slow or no pulse Slow or no breathing, gurgling Skin looks pale or blue, feels cold Pupils are pinned or eyes rolled back Vomiting Body is limp No response to noise or knuckles being rubbed hard on the breast bone Step 1: Rescue Breathing Attempt to stimulate the overdose victim by calling their name or lightly rubbing the sternum. If the overdosing person is unresponsive call 911. If the person is not breathing effectively, perform rescue breathing. Step 2: Prepare Naloxone injection Use a long needle (1 to 1 ½ inches) called an intramuscular needle (IM). These needles can be located at either needle exchange programs or pharmacies. Now, pop off the orange top vial of naloxone. From the vial, draw up to 1cc of naloxone into the syringe. 1cc=1 mL=100 u Step 3: Administer Naloxone Inject the needle straight into a muscle. Thick muscle works best, such as: ◦ Thigh muscle ◦ Upper, outer quadrant of the rear ◦ Shoulder muscle Be sure to inject straight to make sure the muscle is hit. Step 4: Continue rescue efforts After injection of naloxone, continue rescue breathing for 2 to 3 minutes. If there is no change in their breathing after 3 minutes, administer another dose of Naloxone and continue rescue breathing. If the second dose of Naloxone does still not revive the person, something else may be wrong (either the heart has already stopped, there are no opioids in their system, non-opioid drugs are the cause of the overdose, or the opioid drugs were too strong for the Naloxone) Step 5: Monitor the person Stay with the person until emergency responders arrive. If you must leave them alone for any length of time, or if they are unconscious, position them in the recovery position so their airway is clear and they are less likely to choke on their own vomit, as they could aspirate and die if left on their back. If the person revives they will likely be in full opioid withdrawal and want to use. Use every effort to persuade them not to. Key messaging Key messages to reduce risk of death from opioid overdose include: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Do not use alone Use safer routes (i.e. not injecting) Do a test hit first Know the signs and symptoms of an OD Do not mix drugs Carry Naloxone Call 911 if someone is overdosing Know where to find resources Naloxone reverses overdoses but does not treat addiction. Availability of Naloxone To date, Naloxone is not available over the counter, meaning it requires a prescription. Take-home Naloxone kits are available with both a prescription and training on its administration. Health Canada is putting forward an amendment to the prescription drug list to allow non-prescription use of naloxone specifically for emergency use for opioid overdose outside hospital settings. Naloxone Take Home Kit A Naloxone take home kit would include: ◦ 2 glass ampoules of 0.4 mg/ml of naloxone wrapped in gauze inside a pill bottle for protection. Label includes information. ◦ 2 rectangle VanishPoint® safety syringes: 3cc-25g X 1 ◦ 2 alcohol swabs ◦ 2 latex gloves ◦ One-way rescue breathing barrier mask ◦ THN Administration information form with Kit identifier information ◦ Steps to respond to opioid overdose 24 Naloxone Training Training and education on Naloxone include: ◦ ◦ ◦ ◦ Learning the signs of opioid overdose How to perform rescue breathing How to put someone in the recovery position How to administer injectable Naloxone Research has shown that with basic training, almost anybody would be able to recognize an overdose and successfully administer. AHS Online Naloxone Training Alberta Health Services has made a Take Home Nalaxone online training available to non-AHS health professionals. The training includes helpful resources for download. To take this training visit: http://cdm.absorbtraining.ca/#/login 1. 2. 3. 4. Complete sign-up as non-AHS learner. Login to account Click ‘Catalogue’, then click ‘Chronic Disease Management’, then click ‘Addictions and Mental Health’ Choose the Take Home Naloxone Training by selecting ‘Open’. Ensure Pop-up Blocking is turned off, then click ‘Launch’ Website Resources & References Brands, B., Sproule, B., & Marshman, J. (eds) (1998). Drugs & drug abuse (3rd ed.). Canada: Centre for Addiction and Mental Health Drugs Fool (Alberta Health Services campaign): ◦ http://www.albertahealthservices.ca/drugsfool.asp Harm Reduction Coalition: ◦ http://harmreduction.org/issues/overdose-prevention/overview/overdosebasics/responding-to-opioid-overdose/administer-naloxone/ Toward the Heart: ◦ Website: http://towardtheheart.com ◦ Overdose survival guide: http://towardtheheart.com/assets/uploads/files/OD_Survival_Guide_Tips_to_Sa ve_a_Life_2012.08.29_upright_for_website.pdf Know Your Source: ◦ http://knowyoursource.ca Contact Info Sue Howard Landline: (604) 535-2124 Cell: (250) 809-1066 Email: sue@suehowardconsulting. ca 28