* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Opportunistic pathogens and their biofilm “Food for thought”
Molecular mimicry wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Neonatal infection wikipedia , lookup
Phospholipid-derived fatty acids wikipedia , lookup
Quorum sensing wikipedia , lookup
Marine microorganism wikipedia , lookup
Metagenomics wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Infection control wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Antimicrobial copper-alloy touch surfaces wikipedia , lookup
Antibiotics wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Human microbiota wikipedia , lookup
Community fingerprinting wikipedia , lookup
Antimicrobial surface wikipedia , lookup
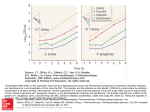
Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) Opportunistic pathogens and their biofilm “Food for thought” Amro A. Amara1,2 1 Protein Research Department, GEBRI, Mubarak City for Scientific Research and Technology Applications, Alexandria, Egypt. 2 Microbiology Division, Pharmaceutics Department, Collage of Pharmacy, King Saud University, Riyadh, Kingdom of Saudi Arabia "The philosophy behind being calm or pathogen should stop us to think, what those opportunistic pathogens want to tell us?" The author Opportunistic pathogens are a group of microbes which can live friendly without causing diseases for healthy individuals and become virulence with unhealthy and immuno-compromised ones. They are opportunistic and can get the chance whenever there is a chance. Most of them can live in harsh conditions. Especially those are able to produce biofilm. Biofilm protect microbes from many environmental virulence factors. Microbes in biofilm use minimum nutrients and water. Biofilm producing microbes are tricky microbes and need special tools and procedures for their control. Some of those microbes such as Pseudomonads aeruginosa is responsible for most of the secondary infections acquired by patients especially in the hospitals. In fact, even the biofilms produced by opportunistic pathogens has been a subject for studies by many authors there are still many gaps in their control. In this study the resistant to disinfectant, EDTA, H2O2 and phenol. have been investigated in presence and absence of alginate produced by P. aeruginosa on the different tested microbial strains using different test methods. The P. sp and Gordonia sp biofilms on glass and rubber gloves respectively have been induced and then investigated using scanning electron microscope. P. sp show an ability to produce fast biofilm (30 minutes) while G. sp being able to perform biofilm inside and outside the rubber of the gloves. β-lactamase the major enzymes responsible for the degradation of penicillin has been produced and used for evaluating the effect of the alginate biofilm in presence of penicillin/streptomycin combination. The multiple alignments and the phylogenic tree for fifty different P. aeruginosa species has been analyzed. A β-lactamase protein model for P. aeruginosa PO1 has been generated using Modeller 9v8 software. The data prove the diversity of this enzyme and its role in resistant. A discussion about the factors responsible for the dominancy of the opportunistic pathogen in hospital has been included and some simple experiments have been conducted to support the discussions within the text. Protocol/advices for controlling the opportunistic pathogens in hospital have been suggested. Keywords Opportunistic pathogens; Biofilm; Pseudomonas aeruginosa; Offline control. 1. Introduction 1.1.The resistant to the antimicrobial agents It is clear from the number of the published data in different microbiological fields and applications that microbes either being naturally resistant or are able to acquire and build resistant [1, 2]. They can gain the required resistant gene(s) against different antimicrobial agents and drugs through different mechanisms. These mechanisms include recombination, plasmid and transposon elements, transformation and transduction, phage, hyperdization and any possible mechanism for gene(s) transfer. There are many criteria govern the probability of the elevation of the resistant and its control [3]. These criteria include almost all aspects and factors which responsible for its elevation. They can be categorized in three major factors: biological, chemical and physical. Those factors are linked to each other. The resistant or the antimicrobial resistant is the ability of particular microbe(s) to survive in presence of compound(s) proves to be able to kill other microbe(s). Or it’s the ability of the biological system of the microbe to degrade, deactivate, prevent, inhibit or block the antimicrobial agents. In conclusions it is any mechanism involved in the survival of certain microbe(s) from being killed by antimicrobial compounds proves to be harmful or sidle for others. 1.2. Biological factor Biological factor is the most important one because it deals with the feature of the microbe itself and its response to the different antimicrobial agents. Physical and chemical factors are not separated from the biological factor but for simplicity I will describe the biological factor as a separate part. It describes mainly the microbial strain(s) which being naturally resistant to antimicrobial agent(s). Did microbes can be naturally resistant? Yes. This is a fact. P. aeruginosa as an example has the ability to degrade many types of hydrocarbons, disinfectant and antimicrobial drugs. Those compound are either bacteriostatic or bacteriocidel. It has sufficient genetic material to do that. Even some antimicrobial compounds and mainly disinfectants are recognized by P. aeruginosa as a carbon source. P. aeruginosa flourish when cultivated in high dose of some type of disinfectants even higher than those recommended by the manufacture, however this is not an invitation for the production of more potent disinfectants. P. aeruginosa could resist compounds such as phenylmercuric acetate, mercurochrome, fluorescein, mercuric acetate, thimerosal, chlohexidine, cetrimide, acetamide, phenol and antibiotics [4 and the references within]. Amara and Hussain (2006) as well as many ©FORMATEX 2011 813 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) others authors have been described that the un-wise use of disinfectant lead to the flourish of some bacterial species [4]. There are many scientific concepts around that will be discussed within this study. This is due to that disinfectants kill all P. aeruginosa competitors' strains and moreover supply it with water and a suitable carbon source. Furthermore, if the disinfectant which is usually diluted with water has been contaminated by resistant microbe such as P. aeruginosa in a certain container and for some purposes this container has been left for a suitable time which enables an enough microbial multiplication and growth; this mixture will be a source for infection rather than disinfection. Microbes such as P. aeruginosa found in the hospitals environment a comfortable place. In other hand microbes can build a new resistant mechanism either by mutating certain gene to be a resistant for a particular antimicrobial agent(s) or by activating a certain efflux system for getting rid of the antimicrobial agent and preventing it from damaging its macromolecules. Mutation in β- lactamase gene can cause a multiple antibiotic resistant. β-lactamase is the resistant factor to the β-lactam antibiotics. The plasmid-encoded TEM β-lactamase is the most prevalent one in gram-negative enteric bacteria [5, 6]. A discovery of new generation of β-lactam antibiotics leads to induce new resistant strains that are reported as sensitive. The scientists are typing to understand why microbes have the conversion ability to a newly resistant form. Venkatachalam et al., (1994) have investigated TEM β-lactamase variants with amino acid substitutions in the active-site pocket of the enzyme. The experiments have been identified in natural isolates with increased resistance to extended-spectrum cephalosporins, such as cefotaxime and ceftazidime. Mutants were selected for 100fold more ceftazidime resistance than wild-type. All mutants had a serine substitution at position 238, a lysine or arginine at position 240, and a small amino acid at position 241. This is an example about what could happened in the lab. The nature is more dynamic and the probability that similar or more forms can be happened is very high. There are many other integrated systems for protecting microbes against the antimicrobial agents. Spore forming bacteria can produce spore for the microbes' protection against antimicrobial agents till the condition become suitable for germinating a vegetative cell. Exopolysaccarid formation is another system for the protection. Alginate can cause mechanical protection by coating or immobilizing the microbial cells. Or as a chelating agent. Yes many antimicrobial drugs can pass through the alginate biofilm and kill the bacterial cells but in most cases they cannot eradicate the entire vegetative cell. The dead cells plus the alginate will be a cover protects some of the microbial population. The big microbial biodiversity and the powerful of the biological system give microbes under attack another chance by supplying them with an extra genetic material from another one which could survive and able to supply the others on risk with genes responsible for that. Plasmids transduction and phage attack considered as resistant genes transmitter within microbes. Authors have been described so early that genes can also be transmitted through the genomic DNA. Dead cells which their DNA still un-attacked can be considered as an unlimited source for transferring new genetic materials [7, 9]. Hyperdization can be also existed naturally. As an example which can explain the dynamic of the genes transfer mechanisms enterohemorrhagic E. coli isolates contain virulence plasmids and pathogenicity islands similar to those found in Shigella spp. [7, 8]. Many as 1387 new genes in comparison with the previously sequenced nonpathogenic laboratory strain E. coli K-12 have been acquired [9]. Biological system support the direction which safe creations. Unwise microbial treatment will elevates the harmful or the evil face of the microbes. The concept of microbial treatment should be reevaluated. Some leakage in the knowledge can cause severe problems. H2O2 which is a source for oxidants and produced during the natural defense mechanism of the lung infected with microbes can give negative results. H2O2 mutate P. aeruginosa and stress it to produce more alginate which make serious problems to the patients. The reaction of biological system could not be expected. Amara and Hussain (2006) and Hussain and Amara (2006) as well as many other authors recommended using case-by-case study for evaluating each microbe and each strain as a unique single case rather than using a general method(s) for evaluations [4, 10]. Using chemotherapeutic agent in charge of neglecting the immune system is a most common mistake in the clinical treatment by physician and patients. The immune system should be given the first priority then come the chemotherapeutic agents. I suggested that the academic research on the conditions responsible for producing both natural and induced mutations should be given more support. A pad practice in many medicinal and pharmaceutical sectors nowadays can be observed. Treating patients with browed spectrum antibiotics and the use of single disinfectant all the time are examples. 1.3.Chemical and physical factor The effect of the chemical and physical factors is not separated from the biological one. The optimum growth of microorganism depends upon two factors: favorable physical conditions e.g., temperature, pH etc., and suitable medium. Versus the optimum growth, the controlling of the microbial growth will be by the aid of unfavorable physical condition(s), less or no nutrients and the usage of the antimicrobial agents. Antimicrobial agents are chemicals compounds that kill or inhibit the growth of the microbes. Killing of the microbes is important in everyday practices, such as water purification, milk pasteurization and refrigeration of foods [1, 2]. The principle reasons for practicing methods of microbial control are to prevent transmission of disease and infection, to prevent decomposition and spoilage and to prevent contamination. Conditions which influencing antimicrobial action are including its concentration, its chemical constituents, intensity and nature of physical agent such as time, temperature and the material bearing the organisms. The mode of action can be summarize in the damage to cell wall, alteration of cell permeability, colloidal nature of protoplasm, inhibition of enzyme activity and interference with synthetic processes. Disinfectants are used widely to control microbes. However, there is no ideal or for any and all purposes disinfectant [1, 814 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) 2]. The disinfectant usually specified based on its toxicity to microorganisms, solubility, stability, non-toxicity to man and other animals, homogeneity, capacity to penetrate, non corroding and non-staining, deodorizing ability, detergent capacity and availability. Disinfectants have three mode of action: Initial damage to the cell membrane resulting in the loss of important cell constituents, alkylating agent and oxidizing agent. In case of damage to the cell membrane gram negative bacteria are more sensitive to membrane – active disinfectants than are the gram negative species because of difference in cell wall composition. Gram negative bacteria are relatively resistant because they contain complex lipoprotein and lipopolysaccharides which impede access of antimicrobial agent to the underlying membrane [1, 2]. If these cell wall components are disaggregated and magnesium ions removed by treatment with EDTA the susceptibility of gram-negative bacteria is generally increased [10, 11]. Alkilating agents are able to kill spores, react with nucleic acid and protein. Oxidizing agents are responsible for the oxidizing of the macromolecules in the cell. In case of in vivo controlling microbes two major terms are used; the antibiotic and the chemotherapeutic agents. They must destroy or prevent the activity of a parasitic without injuring the cells of the host or with only minor injury to its cells, it must be able to come in contact with the parasite by penetrating the cells and tissues of the host in effective concentration and it must not interfere with the host's natural defense mechanisms, such as phagocytosis and the production of antibodies [1]. 1.4.Research concerning Pseudomonas aeruginosa P. aeruginosa is an opportunistic pathogen, it can cause severe attack for patients especially those have different kind of problems in their immune system. Using genetic techniques, P. aeruginosa has been studied in more detail comparing with any other pseudomonad. Its physical and genetic chromosome maps have been described. P. aeruginosa complete genome sequence has been published in 2000 [1, 2]. P. aeruginosa has one of the largest sequenced (6.3 Mbp) bacterial genome enables better environmental adaptation [12]. P. aeruginosa contains the highest proportion of regulatory genes (8.4%) observed for a bacterial genome and a large number of genes involved in the catabolism, transport and efflux of organic compounds and a potential chemotaxis systems [13]. The size and complexity of this genome probably reflect an evolutionary adaptation permitting it to thrive in diverse environments and to resist the effect of a variety of antimicrobial substances [12]. However there is no real solution for preventing P. aeruginosa infections due to its various resistant mechanisms. P. aeruginosa can adapt itself in different kind of environmental condition and can survive and replicate in minimum nutrition conditions such as in drinking water containing traces of organic compounds. P. aeruginosa is dominant in hospital environments and need a special care to prevent it from infecting patients. Better understanding for P. aeruginosa regarding to their interaction with, chemicals, antibiotics, drugs, disinfectants, and different environmental factors will lead to a better control and treatment. Recently Amara et al. (2011) show the possibility to map the history of P. aeruginosa's alginate producing genes and investigate their validity and viability [14]. P. aeruginosa can multiply in water environments and also on the surface of suitable organic materials in contact with water. It has been isolated from a range of moist environments such as sinks, water baths, hot water systems, showers and spa pools. P. aeruginosa mediates acute infections, and known as the most dominant pseudomonades species isolated from clinical sources especially immunocompromised patients (Jones, et al., 2003). P. aeruginosa cause severe problems to patients with different kind of illness [15-28]. P. aeruginosa have several virulence factors like extracellular toxins [29] and proteases [30] which adapt specific host tissues infection. The continuous sanitation by a single disinfectant could release a P. aeruginosa resistant strain [31]. P. aeruginosa shows inherent multidrug resistance mechanisms by outer membrane low-permeability and some specific multi-drug efflux (Mix), like Mix XY-OprM [32]. Mutant of nalB gene of P. aeruginosa leads to overexpression of outer membrane protein OprM (49 kDa), with increase in the resistance to quinolones, cephems, penams, meropenem, tetracycline, chloramphenicol and erythromycin [33]. P. aeruginosa like others pathogenic bacteria gained extra resistances through different rots of gene transfer [34]. 1.5.Biofilm formation Biofilm formation is a common future in different kind of bacterial strains. It is an efficient mechanisms which protect microbes against different environmental factors [35-39]. In case of Pseudomonads they are able to adapt a quick biofilm as shown in this study. A biofilm composed of P. aeruginosa starts growing on a surface when a flow of liquid medium and bacteria passes by, and some of the bacteria adhere to the surface. This adhesion is reversible during the first couple of hours; later the adhesion becomes irreversible due to pili and glycocalyx of the bacteria (mainly polysaccharides) [40]. The bacteria can metabolize the organic molecules on the surface, and some bacterial genes are only activated when the bacteria adhere to surfaces; other genes are activated by altered environmental conditions, e.g., phosphate starvation, nitrogen starvation, increased NaCl concentration, dehydration etc., leading to production of exopolysaccharides and adhesion [41]. The growing biofilm consists of multiple cellular layers [42]. There are qualitative and quantitative changes in the components of the bacterial cell wall lipopolysaccharide (LPS) and outer membrane proteins [43]. P. aeruginosa which is the dominant pathogen in hospitals; its biofilm play a major role in its survive [44]. In case of lung infection it become fatal based on their ability to produce alginate especially with Cystic Fibrosis patients [45-46]. Different mechanisms have been introduced to control the bacterial biofilm in general and P. aeruginosa particularly [47-48]. The alginate chemical structure is composed of a polymer arranged in homopolymeric ©FORMATEX 2011 815 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) block structure of urinic acid β-D-mannuronate and its C-5 epimer α-L-guluronate. The well-studied relatively flexible gel alginate-Ca2+ from P. aeruginosa do not contain polyguluronate block [49] which present on those rigid gels from Azotobacter vinelandii alginate-Ca2+. The research done on P. aeruginosa biofilm did not establish a clear protocol for its prevention [51-52]. Alginate lyase enhances the antibiotic killing of mucoid Pseudomonas aeruginosa in biofilms [52]. Many researchers have been done on alginate lyase aiming to control P. aeruginosa biofilm; however and based on its protein nature; its application might be limited to superficial treatment [57-57]. Authors start to study the P. aeruginosa response to different antibiotics in their biofilm structure [58-62]. The biofilm/oxygen interactions have been studied [63-64]. P. aeruginosa reported to mediate glass dissolution and sorption of metals by its cells and biofilm [65]. When pathogenic bacteria are able to produce biofilm the story will take another image while biofilm will protect microbial cell (even partially) against antibiotics and different kind of drugs [66-67]. In case of P. aeruginosa which is the dominant pathogen in hospitals biofilm play a major role in its survive [50, 68]. 2. Material and Methods 2.1.Microbial strain All bacterial strains represent Pseudomonas aeruginosa, Pseudomonas. sp, Pseudomonas syrangia, Staphylococcus aurese and Gordonia sp were grown routinely in LB and NB or NA medium at 37oC. 2.2.Experiments concerning biofilm formation and analysis 2.2.1.Screaning P. sp strain for their ability to produce fast biofilm Pseudomonas. sp strain isolated in my lab has been investigated for their ability to biofilm formation, which is an indicator for the role of alginate in protection. In 100 ml flask contain 20 ml water a 50 µl from an overnight P. sp culture has been added and left at room temperature for 30 min. One clean new microscopic glass slide has been inoculated with a water drop contain P. sp and allowed to dry at 37oC. The slide then was taken and scanned using the scanning electron microscope to confirm the biofilm formation. 2.2.2.Rubber pieces sterilization and Gordonia sp biofilm formation To sterilize the rubber pieces without deformation of its surface; the pieces were incubated in LB media for one hr, followed by fast freezing in -80oC for 3 hr then washed by cold ethanol several times, and then washed with sterile distilled water. After sterilization each pieces was added to a 100 ml flask contain 25 ml nutrient broth and incubated at 30oC for 24 hr under static conditions. Contaminated flasks were omitted and the uncontaminated flasks which contain the rubber pieces were further used. The sterilize rubber pieces and 100 µl of nutrient broth overnight Gordonia sp culture has been added to 250 ml flasks contain 100 ml of sterilize tap water and incubated in static incubator for seven days at 37oC. 2.2.3.Sample preparation for electron microscopy To study the fast biofilm formation ability of P. sp and the slow one of Gordonia sp on the rubber surface; the scanning electron microscope has been used. In case of P. sp the dried bacterial smear has been used. The rubber part which show surface growth of the Gordonia sp was carefully cut and transferred gently to peteri-dish, the wet pieces washed gently with distilled water several times to remove any salt contaminate the rubber surface. The water wet rubber piece then transferred to the surface of a clean flat glass slide and allowed to dry slowly at 37°C. The slow dry of the rubber on the surface of a flat glass slide enable well attached. 2.2.4.Scanning electron microscope Both of the microscopic slides which contain P. sp and that contain rubber gloves pieces (Gordonia sp biofilm) have been coated with approximately 15 nm gold (SPI-ModuleTM sputter Coater). The golden coated samples then scanned using analytical scanning electron microscope (Jeal JSM-6360LA) with secondary element at 20 KV acceleration voltages at room temperature. The digital image were adjusted and saved. 2.3.In flask alginate production at 37oC For alginate production P. aeruginosa was cultured in static 500 ml LB broth culture using 1 liter glass bottel at 37oC. The amount of alginates produced was determined after 72h. 2.3.1.Alginate purification Alginate has been collected and purified using simple method. Twenty ml of 100 mM EDTA has been added to the culture and the mixture has been vortex gently. The cell has been separated from the supernatant using centrifugation at 1500 rpm for 10 min. The supernatant then collected and double volume of cold ethanol has been added. The mixture then has been put in -70oC refrigerator for 1h. The precipitate then collected by centrifugation at 13000 rpm. The 816 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) precipitate then dialyzed against distilled water (pH 8) in 2L water volume. The dialysis process has been continued for 2 days and the water changed regularly (nearly each 6 hr). The alginate in the dialysis page collected and precipitated with two volume of cold ethanol. The mixture then was stored in -80oC to allow alginate precipitation. The precipitate then collected by centrifugation at 13000 rpm and dried at room temperature (25oC under aseptic condition). The dried alginate preserved in suitable sterile container for further investigation. 2.3.2.FT-IR analysis for alginate The alginate has been examined using FT-IR spectrophotometer. One mg of pure dried alginate was used for FT-IR analysis following the method described by Sherborochk-Cox et al. (1984) [49]. The IR spectrum was compared with a known authentic alginate standard sample using Shimadzu-Spectrophotometer. 2.4.Long term incubation in presence and absence of H2O2 A simple experiment has been conducted to evaluate the effect of H2O2 on the P. aeruginosa in case of long term incubation. Two flasks of 100 ml NB medium have been used. Each flask has been inoculated with heavy inoculum of P. aeruginosa. In one flask 1 ml of 3% H2O2 has been added. Both flasks then incubated at 37oC for three months. The viability of the microbial growth in both flasks has been monitored. 2.5.Evaluation of the effect of H2O2 on P. aeruginosa in presence or absence of the alginate The effect of H2O2 on P. aeruginosa has been evaluated. The experiment conducted in test tube containing 6 ml NB. The following final concentration of alginate have been used, 333, 666 and 1000 µg/ml. In each tube the following final H2O2 concentration have been used 0.041, 0.083 and 0.166 ml of 3%H2O2/ml medium. Constant volume (100 µl) of a fresh culture about 109 CFU then added to each tube. The control was same as above but without the addition of the alginate. The test tubes left at room temperature (25oC) for three days. After that 100µl has been taken from each tube and diluted in 5 ml H2O and then mixed well. 100 µl then transferred again in 5 ml water and 200 µl taken and spread on the surface of the agar plates. The bacterial number in each final dilution for each treatment (1, 2 and 3) has been counted. The colony number of each treatment has been counted and the results have been summarized in Table 1. 2.6.The effect of different antimicrobial agents in P. aeruginosa and P. syringae in presence or absence of alginate Four antimicrobial agents represented in EDTA, H2O2, commercial disinfectants (Chlorophinol as active ingredient the Rideal-Walker coefficient of 3.0-5.0) and phenol have been used against P. aeruginosa and P. syringae. The final concentration/ml of the antimicrobial agents represents 125 mM edta,14.3% phenol, 0.5% H2O2 and six time dilution disinfectant (While it recommended to be used after dilution to 40 time). The different antimicrobial agents have been filtered each using microbial filter (0.22 µm). The microbes has been cultivated each in test tube contain 5 ml NB medium till about 106 CFU. 100 l of each have been added to 6 ml water and from each 800 l has been spread on the surface of agar plate. 800 l of each antimicrobial agent prepared as stock solution has been spread too. The plats left overnight at 37oC. The inhibition in the microbes' number determined as % and the data summarized in Table 2. 2.7.Agar disc diffusion methods (Antibiotics-sensitivity test) Conventional agar disc diffusion method was performed, as described in NCCLS documents (NCCLS 1999) [10, 69], to determine the antibiotic sensitivity. Pinicillin/Streptomycin (P/S) [Gibco BRL-Life technologyies Inc. USA (5000 units Pinicillin /ml:5000 µg/ml Streptomycin sulphate upon dehydration with 20 ml water)] has been prepared manually and 5µl added on a filter paper disk (For each one µl contain 5 units penicillin and 5 µg streptomycin). The antibiotic disks have been loaded on the surface of NA plates contain one of the tested organisms (on its surface). The tested organisms are: Staphylococcus aureus, Pseudomonas syringae and Pseudomonas aeruginosa. The plates with the tested strains and antibiotic disks have been incubated overnight at 37oC. The diameter of the inhibition zone for each antibiotic has been determined and the results represented as sensitive (s), resistant (r) or moderet (m). 2.8.Production of Pencillinase enzyme (β-Lactamase) From the antibiotic resistence profile in Table 1, P. aeruginosa which prove to be resistant to Peniciline/streptomycin was selected for the production of pencillinase. 10 ml of 5000 units pencillin/ml and 5000µg/ml streptomycine mixture both were added to 1 liter bottle contain 500 ml NB medium. The mixture mixed well with the medium and a heavy enoculam of P. aeruginosa then added to the bottle. The bottle incubated for 3 days at 37oC under static condition. 2.8.1.Isolation of the pencillinase 15 ml of the medium was filtered to separate the bacteria using sterile bacterial filter (0.22 µm). Immidiatly the filterate preserved at -20oC for further investigations. The protein content determined spectrophotometrically at 280 nm (PerkinElmer-UV/VIS Spectrometer Lambda) and the amount of protein calculated from a protein standard curve. ©FORMATEX 2011 817 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) 2.9.Study the performance of the antibiotic in the presence of alginate or alginate/β-lactamase An experiment was designed same to the above antibiotic disk diffusion method. After spreading S. aurese (sensitive to P/S and unable to produce alginate) on the surface of the plat, the plat left for the complete dryness and to allow the organism to establish themselves on the surface. Different concentration of the alginate has been used represent 0, 333, 666, 1000 and 1333 µg/ml. On the surface of each plat 50µl of the alginate different concentration has been loaded each in one plat respectively just beside the center of the plat. The antibiotic disk then put in the center of the plat as above. In another group of plates another disk has been loaded additionally contain 5µl of β-lactamase. Plates incubated at 37oC for overnight and the effect of alginate alone or alginate plus β-lactamase on the S. aurese has been evaluated. 2.10.Blast analysis, alignment, phylogenic tree and model study for β-lactamase The Blast databases has been conducted to screen the existence of β-lactamase against the β-lactamase protein sequence of the P. aeruginosa PO1 which has been used as a template and the first fifty protein sequences which represent different β-lactamases of different Ps. aeruginosa have been selected. The fifty protein sequences of βlactamases have been saved in one file as a fasta format. Using Bioedit software v.7.0.9.0 a multiple alignment (for the fifty protein sequences) has been conducted using the alignment option in the Bioedit. The phylogenic tree has been generated too. A model from the evaluable β-lactamase pdb files (2whg, 2wrs, 2wzx and 3if6) using modeller 9v8 software and P. aeruginosa PO1 protein sequence as a template has been generated. The structure of the model has been captured as 3D protein structure. 3. Results and discussion Opportunistic pathogens cause diseases in individuals with immune deficiencies [1]. A wide range of bacteria can act as opportunistic pathogens including species of the gram-negative genera Pseudomonas, Acinetobacter, Serratia and Ligionella; gram positive bacteria such as S. epidermidis, C. jeikeium, L. monocytogenes; and the acid-fast Mycobacterium species [2]. Opportunistic pathogens, such as species of Psudomonas, Acinetobacter, Proteus or Klebsiella are unlikely to affect healthy persons, although they present a serious risk to hospital patients whose immunity to infection is naturally defective or therapeutically depressed [1, 2]. Health care facilities include hospitals, nursing homes, extended care facilities, medical and dental clinic, podiatry and acupuncture patients. Patients occupied or uses of these facilities may be susceptible to infection from their environment [2]. Normal immunological responses are compromised also, to a lesser extent, by the natural process of aging and activities such as smoking [2]. Consequently, nosocomial bacteraemias and penumonias are well-recognized complications of the use of intravenous catheters for the administration of nutrients, fluids or therapeutic drugs and of mechanical ventilation in the treatment of patients in intensive therapy units [70]. This study is a trial to understand the opportunistic pathogen regarding to the increase in the number of problems they are causing and their wide existence in hospitals. Most of the opportunistic pathogen are able to survive in harsh conditions, as an example P. aeruginosa can leave in water contain traces of organic materials! There are two critical questions about the opportunistic pathogens. The first: Why they become suddenly a pathogen? [7-10]. The second: Why they are dominant in a place such as the hospitals? [15-28]. These creatures have enough genetic materials to be pathogen in particular cases and for some extent virulence and fetal pathogenic elements. However they are not pathogen in all cases because there is a better deal makes them nonpathogen [71]. The environment around them supply them with a suitable carbon source satisfy their need and can be utilized with minimal metabolic efforts and in best cases in the form of sugar. No need to fight. In most cases they are satisfy. Perhaps a good example from my previous study was observed during the optimization of the phenol degradation; Acinetobacter sp was the used microbe. When glucose is coexisted with phenol, the microbe did not degrade the phenol at all. However, if there is no glucose in the medium the microbe degrades the phenol efficiently [71]. Microbes are wiser than we expected. The second point that there is no real danger stimulate a critical defense conditions. Living in peace and good environment make those microbes calm and friendly to us. Yes! Because they are usually responsible for degrading wide range of waste compounds and materials. So what has been happened make such a change? To understand this point and to be able to answer this question we should know that the microbes sense the materials around them in most cases in the behave that they are food or non-food. Or they are a safe or a harmful food. In case of the presence of a powerful immune response, microbe will specify us as a harmful food while in case of immunocompromized patients it will specify them as a source of good food. If the microbe gets the sense or the signal that there is a food, it will start mechanically to react either by drawing this food to its cytoplasm or by excreting some enzymes able to degrade it [1, 2]. This material under degradation can be part of our body. In contrast when our body or the cells in a particular tissue or part in our body sense that there is an invader the immune system was show a fast interaction by the evaluable entire weapon at once. The organism will specify us as a harmful food. This is made a sort of respect between the opportunistic pathogen and us. However for many reasons our immune system become inefficient and the microbe sense that and start to attack. So the opportunisty is nothing but it is a condition where the microbes have no problem to invade our body and react with it as a source of nutrient. In another words the origin of the problem in case of the opportunistic pathogens come from us and not from the microbes. This clearly clarify that one 818 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) should maintain his immune system and allow it to rebuild itself by given it the chance to reacts with the pathogens. Excess treatments with antimicrobial agents should be minimized. In some other cases microbes enter to the blood circulation by accident and found no defenses and start to attack. In this case the problem will be exponential due to the toxins excreted by the microbes which harm us a lot. This is highlighted that the microbes did not turned to a pathogen but we who become susceptible. This did not explain the dominance and the existence of the opportunistic microbes in places such as hospitals. To understand what going on an example will be described. Cetrimide and acetamide are two components used widely to kill microbes while they are really having these criteria but not all of them will be killed [4]. P. aeruginosa is one of the microbes which did not killed by those two potent compounds. So what is really happened? The disinfectants contain such two compounds kill most of the existing microbes and leave P. aeruginosa and some other alone. Those survived or resistant microbes grow well and extend the area of their existence in charge of those have been eradicated. This is explaining why P. aeruginosa is usually found as secondary infections in hospitals. The nature of the microbial ecosystem is built in certain balance where no one become dominant but all survive and existed side by side. Our continuous changing to the environment lead to the change of this biological balance and problems reveled. In nature P. aeruginosa has different self protection mechanisms. But its number is limited due to other microbes around. By killing most of the microbes around it, we give it the chance to multiply and to grow in more space. Being dominant is not mean that they are become harmful for a healthy persons' but the chance to attack nonhealthy or immunocomperimized patients will be high. Most of the microbiologists know that the microbes which have been built the revolution of the biotechnology have been mutagenized to increase their productivity. This has been happened in the early research using mutagenic chemicals. What we do to a microbe such as P. aeruginosa when we but it under attack from different chemical compounds in a places such as hospitals? We mutagenize it to produce more harmful structure for us. As an example P. aeruginosa mucoid conversion using chemical compounds has been reported wildly. Amara et al. (2011), conducted in tube experiment to show that P. aeruginosa different strains have different responses to H2O2 based on the viability and the validity of their algs genes which are responsible for the alginate production [14]. Let us imagine this scenario: P. aeruginosa which is naturally nonmucoid as a wild type, moves from place to place and from generation to generation without any problem safely. In such cases its genetic materials most probably will not be changed and still wild. Suddenly and by accident it found itself in a hospital by one or another way. This peacefully microbe found itself under attack by huge number of chemicals of different types but "God wellness" it has enough genetic materials to defense themselves. However and for some extent and due to the severity of the attack some of those compounds mutate one or more genes such as genes responsible for the alginate production. A patient with immunocompermised immune system inters the same hospital for some reasons. During treatment P. aeruginosa alginate overexpresion mutant found itself in the patient lung. Yes the immune system is compromised but it still active. The lung starts to attack this invader while it starts to attack the lung. The attack was by H2O2. H2O2 is really potent oxidant cause damage for the macromolecules of the microbe and the lung simultaneously. The microbe starts to excrete alginate to neutralize the situation, to make everything calm and to protect them-selves. The patient will be severely suffered from the alginate, the microbes' virulence factors and H2O2. H2O2 and the viscous polysaccharide will interfere with the lung function. H2O2 could not stand alone in case of immunocompermized patients and the patient will suffer. This is only one example from hundred have the same concept. This explains that we make our enemy by wrongly mutated microbes by unwise attacking. It is wise to understand the nature balance and that we could not eradicate those microbes without harming ourselves. One should highlighted that P. aeruginosa when survive in nature it can protect other microbes as this study addressed. The ability of P. sp to produce fast biofilm has been evaluated Fig 1 a). As well as the biofilm formed by the Gordonia sp on/inside the rubber gloves. P. sp shows an ability to produce fast biofilm (in 30 min). In case of the rubber gloves which are used wildly in hospital Gordonia sp has been grown on its surface and inside it Fig b). The bad management of the rubber gloves wastes or similar materials can favors the formation of Gordonia and similar microbe's biofilm. Rubber gloves take its importance from that it used in hand which is the main responsible part in the body for the transmitting of the diseases. The electron scanning microscope show that Gordonia sp has been growing inside the rubber gloves. This can be happened nearly in all natural or synthetic compounds. In materials used inside the body the problem will be more complicated. a) b) c) Fig 1 Biofilm of P. sp and a) Biofilm of Gordonia sp b) IR analysis of alginate: the upper curve is the isolated alginate and the lower curve is the alginate standard c) ©FORMATEX 2011 819 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) The P. aeruginosa alginate has been produced. The static cultivation proves to be efficient where about 2 gm alginate /L has been produced under the experimental conditions. The produced alginate has been isolated and purified using simple method. It has been characterized using FT-IR against P. aeruginosa authentic alginate standard sample. Both of the alginate and the standard sample are nearly identical Fig 1 c). The alginate produced by P. aeruginosa was used in a series of experiments to prove its protection against the different tested antimicrobial agents. A simple experiment has been conducted to evaluate the effect of H2O2 on the P. aeruginosa grown on NB medium in closed bottel. Unexpectedly the presence of H2O2 lead to the survive of P. aeruginosa when incubated at 37oC for three months while the other bottle which contain no H2O2, P. aeruginosa has been dead after forty days Fig 2. Perhaps this experiment can explain why P. aeruginosa can survive in the presence of oxidants. Its survive in our experiment conditions might be explained that H2O2 will reduce the number of cells and keep the nutrient longer and O2 enable P. aeruginosa to survive under the experimental conditions. Fig 2 Long term incubation of P. aeruginosa, on the left flask without H2O2 and on the right flask with H2O2 The effect of different amounts of H2O2 in presence of different amounts of alginates has been evaluated in the treatment 1, 2 and 3 as in Table 1. In treatment 1 and 3 the use of the H2O2 has reduce the bacterial number. In case of treatment 2 the use of H2O2 increases the bacterial number. This can be explained that there is a certain balance between the amount of H2O2 and the amount of alginate. In treatment 2, mutants might be elevated which responsible for the increase in the microbial number upon the treatment with H2O2. Or that microbe reproduces faster as a mechanism for resistant. In contract in treatment 3 the balance between H2O2 and alginate become nearly in the same edge. Table 1. The effect of different amounts of H2O2 in presence of different amounts of alginate Treatment 1 Treatment 2 Treatment 3 H2O2 µl/ml (3%) Alginate µg/ml 0.041 0.083 0.166 333 666 1000 Without H2O2 With H2O2 Colony numbers 500 344 300 381 700 600 Another experiment has the same concept has been conducted on plat by using EDTA, phenol, commercial disinfectant and H2O2. The experiment gives the same results and proves the protective effect of the alginate against various antimicrobial compounds. In case of using H2O2 a mucoid conversion of some colonies have been observe. The elevation of mucoid only in case of H2O2 is a sign for its mutagenic capacity. Mucoid conversion by P. aeruginosa can be used to evaluate different kind of antimicrobial agents. The existent of alginate prevent the eradication of P. aeruginosa upon the existence of H2O2. The data show great variation between P. aeruginosa and P. syringae. P. syringae which isolated from plant source and less adapted to various used antimicrobial agents. P. aeruginosa is more resistant to all antimicrobial agents comparing with P. syringae, in spite of the case of H2O2. In case of the used commercial disinfectant P. aeruginos nearly not effected as shown in Table 2. Table 2. Effect of different antimicrobial agents in P. aeruginosa and P. syringae Control EDTA H2O2 Disinfectant Phenol P. syringae P. aeruginosa % of inhibition 0 0 10 0 40 70 100 10 100 60 Three microbes used in this study and represent S. aureus, P. syringae and P. aeruginosa to investigate their sensitivity against Penicillins/Streptomycin. S. aurese and P. syringae were sensitive while P. aeruginosa was resistant. P. aeruginosa which was completely resistant to Penicillins/Streptomycin has been selected for the production of lactamase. The mixed Penicillin/Streptomycin has been used for the induction of the -lactamase production in NB. The 820 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) supernatant which contain the -lactamase has been purified using bacterial membrane filter (0.22µm) and refrigerate at -20oC for further investigation. Penicillins/Streptomycin combination has been used while it contains two antibiotics. By using -lactamase produced from the P. aeruginosa it is possible to inactivate the effect of penicillin but streptomycin will still existed. This will enable better detection for the role of the alginate in the protection against antibiotics. Moreover while streptomycin inhibit the bacterial ribosome it will be more possible for preventing its action by the aid of alginate. So streptomycin ineffective if alginate layer was prevents it from being in contact with the microbes ribosomes. Table 3. Antibiotic (P/S) sensitivity test Antibiotic name Microbial names and antibiotic sensitivity results S. aureus P. syringae P. aeruginosa S S R P/S 5µl/disk The results show that alginate has a basic role in protecting microbes against the antibiotics and that the result could be improved upon the use of -lactamase however, the alginate concentration is a critical factor Fig 3. This experiment represent what exactly happened in the nature where microbes defense themselves by the possible existing mechanisms and that upon this reaction it could be survived and other surrounding microbes could be survived too. In presence of antibiotics; P. aeruginosa can use both of alginate and -lactamase to overcome the situation. In our experiment P. aeruginosa did not do that by itself but its -lactamase and alginate both have do that. a) b) c) Fig. 3 S. aureus sensitivity test against P/S a) in low concentration of alginate b) and in high concentration of alginate By evaluating the results obtained from the antibiotic sensitivity test in presence of alginate or alginate plus lactamase as well, the dimension of the inhibition zone as in Figure 3 it is clears that alginate alone is less effective in the protection of S. aureus (the tested strain) than the alginate plus -lactamase. The more the alginate concentration, the more the decrease in the inhibition zone and increase in survive of the microbe as shown in the Fig 3. -lactamase could reduce the effect of Penicillin but the effect of Streptomycin will still be enough to inhibit the growth. However alginate could protect the microbe under its layer from being killed as in the Fig 3. -lactamase which is the enzyme used for degrading Penicillin and which has been investigated in this study has been a subject for further investigation regarding to its protein biodiversity using 50 P. aeruginosa's -lactamases. The -lactamases of P. aeruginosa PO1 has been used as a template. The enzyme proves to be very diverse. In only one microbial species one can found such diversity in one enzyme. This has been proved also by the aid of the protein sequence multiple alignment of these enzymes Fig 4, 5. The protein model generated in this study show that this enzyme built from two group of -sheet and -helix which makes it more resistant to be impaired by mutant happened within its frame Fig 5. The phylogenic tree did not locate -lactamases in one group but in many groups each one has enough distance from the other Fig 5. It is clear from the argument and hypothesis included in this study that opportunistic pathogen have a lot to protect themselves against the used antimicrobial agents, and we should handle the situation more wisely and precisely. It is not only responsible for its own survive but also for surviving of other microbes. Unfortunately, enzymes such as -lactamases are usually spread between microbes through the transduction process by the aid of different forms of the mobile genetic elements (e.g. plasmid). This will increase the scope of the problem. In previous study Amara and Hussain (2006) are introduce an off-line strategy for controlling P. aeruginosa [4]. Based on the data evaluable upon the behavior of P. aeruginosa a handy protocol or advices will be introduced can be used for limiting the spreading of such a pathogen or other opportunistic pathogens especially in the hospitals. 4. Protocol/advices for controlling opportunistic pathogen in hospital 1- All medical materials able to sterilize using autoclave should be sterilized using it. 2- Sterilize disposable materials should be used as much as possible especially for those could not be sterilized by using the autoclave. ©FORMATEX 2011 821 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) 3- Disinfectants or other forms of antimicrobial agents should be used if diluted at once. Excess amount should be not used if left under conditions where microbes could multiplicities. 4- Immunocomperimized patients should be separated each in safe room and disposable sterilize materials should be used in every contact before and after. 5- Instruments, floor etc., should be air dried after being disinfected. 6- All employers in the hospital should be aware with the microbiological aspect and the concept of microbial transmission and control. 7-Microbiological lab should be in every floor and sample from each place, instrument and each person especially those in contact with the patients should be taken regularly and randomly to keep the awareness and to early discover any localization of infections. 8- Food should be either from refrigerator to the patient to the garbage or from coked food to patient to garbage. 9-Any Disinfectant should be changed by another one from time to time. 10-Doctores and nurses must be with high qualifications, well trained and with excellent background in the field of hygiene and microbiology. 11-One patient/one room strategy should be used with all patients in the best case. 12- Filtered air should be used everywhere. 13- Special attention should be directed to the role of the hand in the diseases transmission. I suggest obligatory use of two gloves, so one can be removed in emergence case. 14- Gloves should be evaluable everywhere. 15- The used antiseptics and disinfectants should be tested against any microbe isolated from the hospital environment for early detection for the presence of resistant(s). 16- Fast identification methods should be used such as RAPD technique. 17- Identifying the existence of the microbes through intelligent detection for its DNA/RNA using PCR or RTPCT technology should be established side by side with the convenient biochemical identification methods. 18- The input /output for any material in the hospital should be archived. gi|45273|emb|CAA38522.1| gi|3342495|gb|AAC27624.1| gi|167077402|gb|ABZ10931.1| gi|77539348|dbj|BAE46547.1| gi|77539346|dbj|BAE46546.1| gi|27817549|emb|CAA66659.1| gi|151076|gb|AAA25741.1| gi|151075|gb|AAA25740.1| gi|81345570|gb|ABB71442.1| gi|74422686|gb|ABA06533.1| gi|296550|emb|CAA80304.1| gi|300391745|gb|ADK11242.1| gi|295002675|gb|ADF59108.1| gi|10946341|gb|AAG24865.1|AF30 gi|54303993|emb|CAH04650.1| gi|114881106|ref|YP_758647.1| gi|3859496|gb|AAC77431.1| gi|160334145|gb|ABX24470.1| gi|1389802|gb|AAC46344.1| gi|3220160|gb|AAC23554.1| gi|114703517|emb|CAK12637.1| gi|145651397|emb|CAJ40948.2| gi|145587492|emb|CAJ40947.1| gi|145587490|emb|CAJ40946.1| gi|10946343|gb|AAG24866.1|AF30 gi|45934118|gb|AAS79143.1| gi|5670201|gb|AAD46628.1|AF162 gi|300391788|gb|ADK11274.1| gi|260677492|gb|ACX47976.1| gi|784888|gb|AAC41449.1| gi|4105088|gb|AAD02245.1| gi|156915249|emb|CAO78546.1| gi|156915242|emb|CAO78540.1| gi|1435172|emb|CAA67040.1| gi|48857|emb|CAA41211.1| gi|48810|emb|CAA40146.1| gi|12230878|sp|P24735.2|AMPC_P gi|15599305|ref|NP_252799.1| gi|296387334|ref|ZP_06876833.1 gi|116052144|ref|YP_789012.1| gi|218889605|ref|YP_002438469. gi|152987941|ref|YP_001346370. gi|150963099|gb|ABR85124.1| gi|15600707|ref|NP_254201.1| gi|152987730|ref|YP_001348858. gi|150962888|gb|ABR84913.1| gi|463168|gb|AAA66058.1| gi|162329629|ref|YP_470686.2| gi|603184|gb|AAA57329.1| : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : * 120 * 140 * 160 * 180 * 200 FTATLAGYALTQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FKVVLCGAVLARVDAGDEQLERKIHYRQQD--------------LVDYSPVSEKHLADGMTVGELCAAAITMSDNSAANLLLATVGGPAGLTAFLRQIGD FKGFLAAAVLARSQQQAGLLDTPIRYGKNA--------------LVPWSPISEKYLTTGMTVAELSAAAVQYSDNAAANLLLKELGGPAGLTAFMRSIGD FTVTLAGYALAQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALAQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FKVLLCGAVLSRVDAGQEQLGRRIHYSQND--------------LVEYSPVTEKHLTDGMTVRELCSAAITMSDNTAANLLLTTIGGPKELTAFLHNMGD FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FTTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKIPNAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLTLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKIPNAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLSLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK FKTIACAKLLYDAEQGKVNPNSTVEIKKAD--------------LVTYSPVIEKQVGQAITLDDACFATMTTSDNTAANIILSAVGGPKGVTDFLRQIGD FKVLLCGAVLSRVDAGQEQLGRRIHYSQND--------------LVEYSPVTEKHLTDGMTVRELCSAAITMSDNTAANLLLTTIGGPKELTAFLHNMGD FKVLLCGAVLSRVDAGQEQLGRRIHYSQND--------------LVEYSPVTEKHLTDGMTVRELCSAAITMSDNTAANLLLTTIGGPKELTAFLHNMGD FKIPSAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLTLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK FKIPSAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLSLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK FKIPHTLFALDAGAVRDEFHVFRWDGAKRS----------------FAGHNQDQNLRSAMRNS--------------TVWVYQLFAKEIGENKARSYLEK FKVLLCGAVLSRVDAGQEQLGRRIHYSQND--------------LVEYSPVTEKHLTDGMTVRELCSAAITMSDNTAANLLLTTIGGPKELTAFLHNMGD YKVANSLIGLSTGAVRSADEVLPYGGKPQR----------------FKAWEHDMSLREAIKAS--------------NVPVYQELARRIGLERMRANVSR YKVANSLIGLSTGAVRSADEVLPYGGKPQR----------------FKAWEHDMSLRDAIKAS--------------NVPVYQELARRIGLERMRANVSR YKVANSLIGLSTGAVRSADEVLPYGGKPQC----------------FKAWEHDMSLREAIKAS--------------NVPVYQELARRIGLERMRANVSR FKIPHTLFALDAGAVRDEFQIFRWDGVNRG----------------FAGHNQDQDLRSAMRNS--------------TVWVYELFAKEIGDDKARRYLKK YPSNGLIVRDGDELLLIDTAWGAKN---------------------TAALLAEIEKQIGLPVT--------------RAVSTHFHDDRVGGVDVLRAAGV ---------------------------------------------------------------------------------------------------FKIPNAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLTLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKN FKIPNAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLTLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK FKIPHTLFALDAGAARDEFQVFRWDGIKRS----------------FAAHNQDQDLRSAMRNS--------------TVWIYELFAKEIGEDKARRYLKQ FKIPNAIIGLETGVIKNEHQVFKWDGKPRA----------------MKQWERDLSLRGAIQVS--------------AVPVFQQIAREVGEVRMQKYLKK YPSNGLIVRDGDELLLIDTAWGAKN---------------------TAALLAEIEKQIGLPVT--------------RAVSTHFHDDRVGGVDVLRAAGV YPSNGLIVRDGDELLLIDTAWGAKN---------------------TAALLAEIEKQIGLPVT--------------RAVSTHFHDDRVGGVDVLRAAGV VPKHGLVVLVNAEAYLIDTPFTAKD---------------------TEKLVTWFVER-GYKIK--------------GSISSHFHSDSTGGIEWLNSRSI FKIPNALIGLETGAIKDERQVFKWDGKPRA----------------MKQWEKDLKLRGAIQVS--------------AVPVFQQIAREVGEIRMQKYLNL FKVLNTLIALEEGAISGENQIFHWNGTQYS----------------IANWNQDQTLDSAFKVS--------------CVWCYQQIALRVGALKYPAYIQQ FTATLAGYALTQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALTQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALAQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALAQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDRAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALAQDKMRLDDRASQHWPALQG-SRFDG--------ISLLDLATYTAGGLPLQFP---DSVQKDQAQIRDYYRQWQPTYAPGSQRLYSNPSI FTATLAGYALAQDKMRLDDRASRHWPALQG-SRFDG--------ISLLDLGTYSAGGLPLQFP---DAVQKDPAQIRDYYRQWQPTYAPGSHRQYSNPSI FTATLAGYALAQDKMRLDDRASRHWPALQG-SRFDG--------ISLLDLGTYSAGGLPLQFP---DAVQKDPAQIRDYYRQWQPTYAPGSHRQYSNPSI YKVANSLIGLSTGAVRSADEVLPYGGKPQR----------------FKAWEHDMSLRDAIKAS--------------NVPVYQELARRIGLERMRANVSR LTASASLQLAERGLLPLDSPLQDSLREFYVRSRFHADQGEADRAVTIRRLLSHQSGLPGDHMPDLFDDRPLPLAQLPAKVSGVWLSNPPGTQVAYSNLGY LTASASLQLAERGLLPLDSPLQDSLREFYVRSRFHADQGEADRAVTIRRLLSHQSGLPGDHMPDLFDDRPLPLAQLPAKVSGVWLSNPPGTQVAYSNLGY ---------------------------------------------------------------------------------------------------FTAALASYAEATGELSLSD--PVALLAMKG-RPFGD--------VPLINLGTHTAGGFPLQVP---DDLKSE-GQLMAYLAAWRPSYAAGTRRSYANPSI FKVLLCGAVLSRIDAGQEQLGRRIHYSQND--------------LVEYSPVTEKHLTDGMTVRELCSAAITMSDNTAANLLLTTIGGPKELTAFLHNMGD g : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : : 182 153 156 182 182 152 152 168 152 168 138 168 168 103 152 155 155 138 138 143 155 137 137 137 132 131 138 138 143 138 131 131 112 138 134 182 182 182 182 182 182 182 137 200 200 167 155 Fig 4. Part of the multiple alignment of primary structures of 50 β-Lactamases. Amino acids are shown in one-letter abbreviations. The shaded lines show conserved amino acids. 822 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) 5.Conclusion Opportunistic pathogens are well adapted to various kinds of stress and different antimicrobial agents. It survive and become dominant upon the use of disinfectants while it is either naturally resistant to it, acquired resistant genes or developed its own resistant mechanism. Alginate and the enzymes which responsible for the degradation or the inactivation of antimicrobial agents could be protect the opportunistic pathogens as well as some other around. βLactamases which responsible for the microbial resistant to β-Lactam antibiotics group is very diverse within the same microbial species. Its structure shows flexibility to resist inactivation due to the presence of two major groups of β-sheet and α helix. Wise management for the hospital environment is in argent need to reduce the existence of the opportunistic pathogen. Unwise use of the antimicrobial agents leads to more problems. More study for the mechanisms responsible for elevation and transmission of the resistant(s) are in need. Smart chemical compound that can kill microbe without induce mutagenesis is in need too. a) b) Fig 5. Phylogenetic tree of 50 P. aeruginosa β-lactamase. The branching order and distance score were calculated by the program tree as described by Feng and Doolittle (1987) [72]. The bar indicates the distance corresponding to one amino acid change per 10 amino acid positions a) Threading model of the β-Lactamase of P. aeruginosa PO1 b) References [1] Frobisher M. Fundementals of microbiology, An introduction to the microorganisms with special reference to the procaryons. 8 ED W. B. Saunders Co. USA 1968. [2] Gardner JF, Peel MM. Sterilization and Disinfection and Infection control. 3ED Churchill Livingston Elsevier Science 1998. [3] Martínez JL, Baquero F. Interactions among Strategies Associated with Bacterial Infection:Pathogenicity, Epidemicity, and Antibiotic Resistance. Clinical Microbiology Review 2002;15(4): 647–679 [4] Amara AA, Hussain MZ. Offline controlling of Pseudomonas aeruginosa resistant to protein inhibitor antibiotics using combination of EDTA and Na-citrate or disinfectant(s). Microbiology (China) 2006; 33:95-100 [5] Venkatachalam KV, Huang W, LaRocco M, Palzkil T. Characterization of TEM-1 β-Lactamase Mutants from Positions 238 to 241 with Increased Catalytic Efficiency for Ceftazidim. J. Boil. Chem., 1994; 269: 23444-43450 [6] Matagne A, Lamotte-Brasseur J, Freare J-M. Catalytic properties of class A β-lactamases : efficiency and diversity. J Biochem., 1998; 330: 581-598 [7] Blattner FR, Plunkett G, Bloch CA, Perna NT, Burland V, Riley M, Collado-Vides J, Glasner JD, Rode CK, Mayhew GF, Gregor J. Davis NW, Kirkpatrick HA, Goeden MA, Rose DJ, Mau B, and Shao Y. The complete genome sequence of Escherichia coli K-12. Science 1997; 277:1453–1474. [8] Casadevall A, and Pirofski LA. Host-pathogen interactions: redefining the basic concepts of virulence and pathogenicity. Infect. Immun. 1999; 67:3703–3713. ©FORMATEX 2011 823 Science against microbial pathogens: communicating current research and technological advances ______________________________________________________________________________ A. Méndez-Vilas (Ed.) [9] Makino K, Ishii K, Yasunaga T, Hattori M, Yokoyama K, Yutsudo CH, Kubota Y, Yamaichi Y, Iida T, Yamamoto K, Honda T, Han CG, Ohtsubo E, Kasamatsu M, Hayashi T, Kuhara S, Shinagawa H. Complete nucleotide sequences of 93-kb and 3.3-kb plasmids of an enterohemorrhagic Escherichia coli O157:H7 derived from Sakai outbreak. DNA Res. 1998; 5:1–9. [10] Hussain MZ, Amara AA. Case-by-case study using antibiotic-EDTA combination to control Pseudomonas aeruginosa. Pak. J. Pharm. Sci., 2006; 19(3), 236-243 [11] Russell AD, Furr JR. The antibacterial activityof a new chloroxylenol preparation containing ethylenedianine tetraacetic acid. J Applied Bacteriology 1977; 43:253-260 [12] Stover CK, Pham XQ, Erwin AL, Mizoguchi SD, Warrener P, Hickey MJ., et al., Complete genome sequence of Pseudomonas aeruginosa PAO1, an opportunis- tic pathogen, Nature 2000; 406 959–964. [13] Høiby N, Johansen KH, Moser C, Song Z,. Ciofu O, Kharazmi A. Pseudomonas aeruginosa and the in vitro and in vivo biofilm mode of growth. Microbes and Infection, 2001; 3: 23-35 [14] Amara AA, Hassan MZ, Abulhamd AT, Haroun BM. algs genes: H2O2 Map their Viability and Validity in Pseudomonas aeruginosa. IJBB. 2011; 321-330 [15] Lasisi OA, Nwaorgu OG. Behavioural pattern of malignant otitis external: 10-year review in Ibadan. Afr. J. Med. Med. Sci., 2001; 30: 221-223. [16] Gronowitz E, Pitkanen S, Kjellmer I, Heikinheimo M, Strandvik B. Association between serum oncofetal antigens CA 19-9 and CA 125 and clinical status in patients with cystic fibrosis. Acta. Paediatr. 2003; 92: 1267- 1271. [17] Sanchis Minguez C, Crespo Liern ML, Perez Enguix D, Compte Torrero L, Montero Benzo R. Cardiac tamponade caused by aortic pseudoaneurysm with fistula in the right ventricle. Rev. Esp. Anestesiol. Reanim. 2003; 50: 521-525. [18] Wang R, Pei F, Chai D, Chen Q , Li X. Influence of anti-alginate serum combined with gatifloxacin on mucoid Pseudomonas aeruginosa biofilm morphology. Zhonghua Yi Xue Za Zhi. 2002; 82, 1276-1278. [19] Ross JJ, Shamsuddin H. Sternoclavicular septic arthritis: review of 180 cases. Medicine (Baltimore), 2004; 83: 139-148. [20] Chizuka A, Kami M, Kanda Y, Murashige N, Kishi Y, Hamaki T, Kim SW, Hori A, Kojima R, Mori SI, Tanosaki R, Gomi H, Takaue Y. Value of surveillance blood culture for early diagnosis of occult bacteremia in patients on corticosteroid therapy following allogeneic hematopoietic stem cell transplantation. Bone. Marrow. Transplant, 2005; 35: 577-582. [21] Ramphal R. Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin. Infect. Dis., 2004; 39(Suppl 1): S25-31. [22] Kumar KG, Bakhshi S, Samantaray JC, Banerjee U, Arya LS. Transthoracic lung aspiration in etiology of pneumonia. Indian. J. Pediatr., 2004; 71: 129-132. [23] Chan PC, Huang LM, Wu PS, Chan PY, Yang TT, Lu CY, Lee PI, Chen JM, Lee CY, Chang LY. Clinical management and outcome of childhood lung abscess: a 16-year experience. J. Microbiol. Immunol. Infect., 2005; 38: 183-188. [24] Chaiban G, Hanna H, Dvorak T, Raad I. A rapid method of impregnating endotracheal tubes and urinary catheters with gendine: a novel antiseptic agent. J. Antimicrob. Chemother., 2005; 55: 51-56. [25] Ali Z. Neonatal bacterial septicaemia at the Mount Hope Women's Hospital, Trinidad. Ann. Trop. Paediatr., 2004; 24: 41-44 . [26] Chacko ST, Chandy ST, Abraham OC, Swaminathan, S, Varghese GM, Priscilla R and Mathai D Pacemaker endocarditis caused by Pseudomonas aeruginosa treated successfully. J. Assoc. Physicians India, 2003; 51: 1021-1022. [27] Al-Ghamdi S, Gedebou M, Bilal NE. Nosocomial infections and misuse of antibiotics in a provincial community hospital, Saudi Arabia. J. Hosp. Infect., 2002; 50:115-121. [28] Agnihotri N, Gupta V, Joshi RM. Aerobic bacterial isolates from burn wound infections and their antibiograms--a five-year study. Burns, 2004; 30: 241-243. [29] Ahuja N, Kumar P, Bhatnagar R. The adenylate cyclase toxins. Crit. Rev. Microbiol., 2004; 30: 187-196. [30] Sarkisova S, Patrauchan MA, Berglund D, Nivens DE, Franklin MJ. Calcium-induced virulence factors associated with the extracellular matrix of mucoid Pseudomonas aeruginosa biofilms. J. Bacteriol., 2005; 187: 4327-4337. [31] Ojima M, Toshima Y, Koya E, Ara K, Tokuda H, Kawai S, Kasuga F, Ueda N. Hygiene measures considering actual distributions of microorganisms in Japanese households. J. Appl. Microbiol., 2002; 93: 800-809. [32] Aires JR, Kohler T, Nikaido H, P Plesiat. Involvement of an active efflux system in the natural resistance of Pseudomonas aeruginosa to amino- glycosides. Antimicrob. Agents Chemother., 1999; 43: 2624- 2628 . [33] Sanchez P, Linares JF, Ruiz-Diez B, Campanario E, Navas A, Baquero F, Martinez JL. Fitness of in vitro selected Pseudomonas aeruginosa nalB and nfxB multidrug resistant mutants. J. Antimicrob. Chemother., 2002; 50: 657-64. [34] Shahid M, Malik A, Sheeba Multidrug-resistant Pseudomonas aeruginosa strains harbouring R-plasmids and AmpC betalactamases isolated from hospitalised burn patients in a tertiary care hospital of North India. FEMS. Microbiol. Lett. 2003; 228: 181-186. [35] McLean RJ, Lawrence JR, Korber DR , Caldwell DE. Proteus mirabilis biofilm protection against struvite crystal dissolution and its implications in struvite urolithiasis. J Urol. 1991; 146, 1138-1142. [36] Begun J, Gaiani JM, Rohde H, Mack D, Calderwood SB, Ausubel FM , Sifri CD. Staphylococcal biofilm exopolysaccharide protects against Caenorhabditis elegans immune defenses. PLoS Pathog. 2007; 3, e57. [37] De Stefano L, Rea I, Armenante A, Giardina P, Giocondo M , Rendina I. Self-assembled biofilm of hydrophobins protects the silicon surface in the KOH wet etch process. Langmuir. 2007; 23, 7920-7922. [38] Iumyna Iu M, Koptieva Zh P , Kozlova IP. [Dynamics of microbial populations in the biofilm on protective coating]. Mikrobiol Z. 2009; 71, 37-41. [39] Perez MM, Prenafeta A, Valle J, Penades J, Rota C, Solano C, Marco J, Grillo MJ, Lasa I, Irache JM, Maira-Litran T, JimenezBarbero J, Costa L, Pier GB, de Andres D , Amorena B. Protection from Staphylococcus aureus mastitis associated with polyN-acetyl beta-1,6 glucosamine specific antibody production using biofilm-embedded bacteria. Vaccine. 2009; 27, 2379-2386. [40] Marshall KC. Biofilms: An overview of bacterial adhe- sion, activity, and control at surfaces, ASM News 1992; 58: 202–207. [41] Costerton J.W., Lewandowski Z.,DeBeer D., Caldwell D., Korber D., James G., Biofilms, the customized microniche, J. Bacteriol. 1994; 176: 2137–2142 824 ©FORMATEX 2011 Science against microbial pathogens: communicating current research and technological advances _______________________________________________________________________________ A. Méndez-Vilas (Ed.) [42] Allison DG, Brown MRW, Evans DE, Gilbert P. Surface hydrophobicity and dispersal of Pseudomonas aeruginosa from biofilms, FEMS Microbiol. Lett. 1990; 71: 101–104. [43] Giwercman B, Fomsgaard A, Mansa B, Hoiby N. Polyacrylamide gel electrophoresis analysis of lipopolysaccharide from Pseudomonas aeruginosa growing planktonically and as biofilm, FEMS Microbiol. Immunol. 1992; 71: 225–229. [44] Panmanee W, Hassett DJ. Differential roles of OxyR-controlled antioxidant enzymes alkyl hydroperoxide reductase (AhpCF) and catalase (KatB) in the protection of Pseudomonas aeruginosa against hydrogen peroxide in biofilm vs. planktonic culture. FEMS Microbiol Lett. 2009; 295, 238-244. [45] Manos J, Arthur J, Rose B, Bell S, Tingpej P, Hu H, Webb J, Kjelleberg S, Gorrell MD, Bye P , Harbour C. Gene expression characteristics of a cystic fibrosis epidemic strain of Pseudomonas aeruginosa during biofilm and planktonic growth. FEMS Microbiol Lett. 2009; 292, 107-114. [46] Tre-Hardy M, Traore H, El Manssouri N, Vanderbist F, Vaneechoutte M , Devleeschouwer MJ. Evaluation of long-term coadministration of tobramycin and clarithromycin in a mature biofilm model of cystic fibrosis clinical isolates of Pseudomonas aeruginosa. Int J Antimicrob Agents. 2009; 34, 370-374. [47] Iudina NA , Kurochkina A. [Biofilm control - modern strategy in prevention and treatment of stomatological diseases]. Stomatologiia (Mosk). 2009; 88, 77-81. [48] Lima FG, Romano AR, Correa MB , Demarco FF. Influence of microleakage, surface roughness and biofilm control on secondary caries formation around composite resin restorations: an in situ evaluation. J Appl Oral Sci. 2009; 17, 61-65. [49] Sherbrock-Cox V, Russell NJ, Gacesa P. The purification and chemical characterisation of the alginate present in extracellular material produced by mucoid strains of Pseudomonas aeruginosa. Carbohydr Res. 1984; 135, 147-154. [50] Leid JG, Willson CJ, Shirtliff ME, Hassett DJ, Parsek MR , Jeffers AK. The exopolysaccharide alginate protects Pseudomonas aeruginosa biofilm bacteria from IFN-gamma-mediated macrophage killing. J Immunol. 2005; 175, 7512-7518. [51] Hay ID, Gatland K, Campisano A, Jordens JZ , Rehm BH. Impact of alginate overproduction on attachment and biofilm architecture of a supermucoid Pseudomonas aeruginosa strain. Appl Environ Microbiol. 2009; 75, 6022-6025. [52] Alkawash MA, Soothill JS , Schiller NL. Alginate lyase enhances antibiotic killing of mucoid Pseudomonas aeruginosa in biofilms. APMIS. 2006; 114, 131-138. [53] Brown BJ , Preston JF. 3rd L-guluronan-specific alginate lyase from a marine bacterium associated with Sargassum. Carbohydr Res. 1991; 211, 91-102. [54] Brown BJ, Preston JF, Ingram LO. Cloning of alginate lyase gene (alxM) and expression in Escherichia coli. Appl Environ Microbiol. 1991; 57, 1870-1872. [55] Breguet V, von Stockar U , Marison IW. Characterization of alginate lyase activity on liquid, gelled, and complexed states of alginate. Biotechnol Prog. 2007; 23, 1223-1230. [56] Cao L, Xie L, Xue X, Tan H, Liu Y, Zhou S. Purification and characterization of alginate lyase from streptomyces species strain A5 isolated from banana rhizosphere. J Agric Food Chem. 2007; 55, 5113-5117. [57] Alipour M, Suntres ZE , Omri A. Importance of DNase and alginate lyase for enhancing free and liposome encapsulated aminoglycoside activity against Pseudomonas aeruginosa. J Antimicrob Chemother. 2009; 64, 317-325. [58] Slack MP , Nichols WW. (1981). The penetration of antibiotics through sodium alginate and through the exopolysaccharide of a mucoid strain of Pseudomonas aeruginosa. Lancet. 2, 502-503. [59] Majtan V , Hybenova D. Inhibition of Pseudomonas aeruginosa alginate expression by subinhibitory concentrations of antibiotics. Folia Microbiol (Praha). 1996; 41, 61-64. [60] Kobayashi O, Ota M, Watanabe H , Kobayashi H. [Actions of macrolide antibiotics on alginate production by Pseudomonas aeruginosa]. Jpn J Antibiot. 1997;50 Suppl A, 95-101. [61] Wood LF, Leech AJ , Ohman DE. Cell wall-inhibitory antibiotics activate the alginate biosynthesis operon in Pseudomonas aeruginosa: Roles of sigma (AlgT) and the AlgW and Prc proteases. Mol Microbiol. 2006; 62, 412-426. [62] Yakupogullari Y, Otlu B, Dogukan M, Gursoy C, Korkmaz E, Kizirgil A, Ozden M , Durmaz R. Investigation of a nosocomial outbreak by alginate-producing pan-antibiotic-resistant Pseudomonas aeruginosa. Am J Infect Control. 2008; 36, e13-18. [63] Xu KD, Stewart PS, Xia F, Huang CT, McFeters GA. Spatial physiological heterogeneity in Pseudomonas aeruginosa biofilm is determined by oxygen availability. Appl Environ Microbiol. 1998; 64, 4035-4039 [64] Stewart PS, Wattanakaroon W, Goodrum L, Fortun SM , McLeod BR. Electrolytic generation of oxygen partially explains electrical enhancement of tobramycin efficacy against Pseudomonas aeruginosa biofilm. Antimicrob Agents Chemother. 1999; 43, 292-296. [65] Aouad G, Crovisier JL, Geoffroy VA, Meyer JM, Stille P. Microbially-mediated glass dissolution and sorption of metals by Pseudomonas aeruginosa cells and biofilm. J Hazard Mater. 2006; 136, 889-895. [66] Ngwai YB, Adachi Y, Ogawa Y, Hara H. Characterization of biofilm-forming abilities of antibiotic-resistant Salmonella typhimurium DT104 on hydrophobic abiotic surfaces. J Microbiol Immunol Infect. 2006; 39, 278-291. [67] Kuzma L, Rozalski M, Walencka E, Rozalska B , Wysokinska H. Antimicrobial activity of diterpenoids from hairy roots of Salvia sclarea L.: salvipisone as a potential anti-biofilm agent active against antibiotic resistant Staphylococci. Phytomedicine. 2007; 14, 31-35. [68] Elkins JG, Hassett DJ, Stewart PS, Schweizer HP, McDermott TR. Protective role of catalase in Pseudomonas aeruginosa biofilm resistance to hydrogen peroxide. Appl Environ Microbiol. 1999; 65, 4594-4600. [69] National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Ninth informational supplement. Wayne, Pennsyslvania: NCCLS; 1999: document M100-S9; Vol. 19. No. 1, Table 21. [70] Elliott TSJ. Intravascular-device infections. Journal of Medical Microbiology 1988; 27:161-167 [71] Amara AA, Salem SR. Logical and experimental design for phenol degradation using immobilized Acinetobacter sp. Culture 2010; IIUM Vol. 11, No. 1, 2010. 98-104 [72] Feng, DF, Doolittle, RF. Progressive sequence alignment as a prerequisite to correct phylogenetic trees. J. Mol. Evol. 1987; 25:351-360 ©FORMATEX 2011 825