* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CV exam_faz III_OCT2013
Survey
Document related concepts
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Myocardial infarction wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Aortic stenosis wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
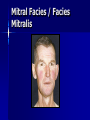
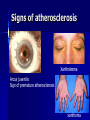
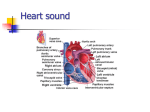
CARDIOVASCULAR EXAMINATION Assoc Prof Elif Eroğlu Büyüköner October 2013 EXAMINATION of the CARDIOVASCULAR SYSTEM General inspection Specific inspection Pulse Carotid Neck veins Praecordium Auscultation Lung bases,liver, ankles Veins and arteries in the legs GENERAL INSPECTION General build and appearence Colour Respiration (abnormal breathing pattern, shortness of breath) Signs of distress and response Conscious level Myxoedema Hyperthyroidism Mitral Facies / Facies Mitralis Ear Lobe Crease Down Syndrome Moonface Acromegaly SPECIFIC INSPECTION Cyanosis – Central: mucous membranes-tongue – Peripheral: extremities Clubbing Anemia Edema Peripheral perfusion Body habitus Specific signs of cardiac pathologies: IE stigmata, arcus senilis, xanthome and xanthelasma CYANOSIS and CLUBBING Central Cyanosis Peripheral Cyanosis Icterus Petechiae Erythema Marginatum Signs of atherosclerosis Xanthelesma Arcus juvenilis Sign of premature atherosclerosis xanthoma Xantoma IE/specific signs Body habitus: Marfan syndrome, thorax abnormalities The PULSE Rate – Normal sinus 60-100bpm – Sinus bradycardia <60 bpm – Sinus tachycardia >100 bpm Regularity – Sinus arrhytmia: varies with respiration – Intermittant irregularity: ectopic beats – Continously irregular: atrial fibrillation Carotid examination Carotid upstroke – Brisk/normal/delaye d – Volume:increased/n ormal/decreased – Anacrotic/bisferiens Carotid auscultation – Bruit – Transmitted murmur – A2 audible in the neck Carotid pulse contour A. Hyperkinetic:AR B.Bisferiens: AS/AR C.Bifid: IHSS D.Hypokinetic/alterna ns: LVD E.Parvus et tardus: AS BLOOD PRESSURE MEASUREMENT Recommended technique for BP measurement Juguler venous pulse Patient position for JVP assessment JVP measurement Jugular Venous Pressure Waveform Normal JVP waves and descents a wave - atrial systole x descent – onset of atrial relaxation c wave - small positive notch in the 'x' descent due to bulging of the AV ring into the atria in ventricular contraction. x' (prime) descent !!! – occurs during systole due to RV contraction pulling down the TV valve ring “descent of the base” – a measure of RV contractility v wave - after the x' descent - slow y descent - rapid emptying of the positive wave due to right atrial filling from venous return RA into RV due to TV opening Abnormal “a” wave AV valve obstruction: TS, RA myxoma Decreased RV compliance:RVH, PS, PHT AV dysassociation:AV blocks, “Cannon” a waves Severe HCM: Bernheim effect No visible “a” wave in AF X’ descent Beginning of the RA diastole, before venous filling to the RA, during RV systole. RVFW moves to the septum, TV moves to the apex and RA base is pulled down (RA pressure falls) More prominent during inspiration Increases with RV contractility:tamponade RV volume inc: ASD, VSD RV pressure inc: PD, PHT Decreases in RV contractility: reduced x’ v wave RA filling, together with S2 Severe TR: CV fusion, no X’ descent y descent • RV filling (early diastole) • Inc: TR, CP, RCM • Dec: Tamponade, TS Apical Impulse: Visualization to assess ventricular size/thickness Normally distinct and located at 4ICS at/inside the midclavicular line Apical Impulse (abnormal): Hyperdynamic impulse in normal location: think increased cardiac output or LVH Hyperdynamic and downward/leftwardly displaced: think LVE Indistinct impulse associated with RVH Precordial heave is seen with RVE Thrills: Palpation of a loud murmur Found in the precordial, suprasternal, or carotid artery area If low intensity murmur, probably just a pulsation and NOT a thrill Auscultation Heart Sounds S1 (cont.): If split heard better at the apex, may actually be S4 or ejection click Tends to be more low-pitched and long as compared to S2 Differentiate S1 from S2 by palpating carotid pulse: S1 comes before and S2 comes after carotid upstroke Decreased S1: Slowed ventricular ejection rate/volume Mitral insufficiency Increased chest wall thickness Pericardial effusion Hypothyroidism Cardiomyopathy LBBB Shock Aortic insufficiency First degree AV block Other Abnormal S1 (cont.): Increased S1: Increased cardiac output Increased A-V valve flow velocity (mitral stenosis) S2: From closure vibrations of aortic and pulmonary valves Divided into A2 and P2 (aortic and pulmonary closure sounds) Best heard at LMSB/2LICS Higher pitched than S1/better heard with diaphragm S2 splitting (normal): Normally split due to different impedance of systemic and pulmonary vascular beds Audible split with > 20 msec difference Split in 2/3 of newborns by 16 hrs. of age, 80% by 48 hours Harder to discern in heart rates > 100 bpm S2 splitting (normal, cont.): Respiratory variation causes splitting on inspiration: pulmonary vascular resistance When supine, slight splitting can occur in expiration When upright, S2 usually becomes single with expiration S2 splitting (abnormal, cont.): Fixed splitting ASD S2 splitting (abnormal, cont.): Wide /mobile splitting Mild PS RVOTO Large VSD or PDA Idiopathic PA dilation Severe MR RBBB PVC’s S2 splitting (abnormal, cont.): Reversed splitting LBBB WPW Paced beats PVC’s AS PDA LV failure Extra heart sounds S3 (gallop): Usually physiologic Low pitched sound, occurs with rapid filling of ventricles in early diastole Due to sudden intrinsic limitation of longitudinal expansion of ventricular wall S3 (cont.): Best heard with patient supine or in left lateral decubitus Increased by exercise, abdominal pressure, or lifting legs LV S3 heard at apex and RV S3 heard at LLSB S3 (abnormal): Seen in HF, severe MR--disappears after treatment S4 (gallop): Nearly always pathologic Can be normal in elderly or athletes Low pitched sound in late diastole Due to elevated LVEDP (poor compliance) causing vibrations in stiff ventricular myocardium as it fills S4 (cont.): Better heard at the apex or LLSB in the supine or left lateral decubitus position Occurs separate from S3 or as summation gallop (single intense diastolic sound) with S3 S4 Associations: CHF!!! HCM severe systemic HTN pulmonary HTN Ebstein’s anomaly myocarditis S4 Associations (cont.): Tricuspid atresia TAPVR CoA AS Kawasaki’s disease Ejection clicks Timing of Heart Sounds Cardiac murmurs Basic Pathophysiology Systolic Diastolic Describing a heart murmur 1. Timing – murmurs are longer than heart sounds – HS can distinguished by simultaneous palpation of the carotid arterial pulse – systolic, diastolic, continuous 2. Shape – crescendo (grows louder), decrescendo, crescendodecrescendo, plateau 3. Location of maximum intensity – is determined by the site where the murmur originates – e.g. A, P, T, M listening areas Describing a heart murmur con’t: 4. Radiation – reflects the intensity of the murmur and the direction of blood flow 5. Intensity – graded on a 6 point scale Grade 1 = very faint Grade 2 = quiet but heard immediately Grade 3 = moderately loud Grade 4 = loud Grade 5 = heard with stethoscope partly off the chest Grade 6 = no stethoscope needed *Note: Thrills are assoc. with murmurs of grades 4 - 6 Describing a heart murmur con’t: 6. Pitch – high, medium, low 7. Quality – blowing, harsh, rumbling, and musical 8. Others: i. Variation with respiration Right sided murmurs change more than left sided ii. Variation with position of the patient iii. Variation with special maneuvers Valsalva/Standing => Murmurs decrease in length and intensity EXCEPT: Hypertrophic cardiomyopathy and Mitral valve prolapse Systolic Murmurs Derived from increased turbulence associated with: 1. Increased flow across normal SL valve or into a dilated great vessel 2. Flow across an abnormal SL valve or narrowed ventricular outflow tract - e.g. aortic stenosis 3. Flow across an incompetent AV valve - e.g. mitral regurg. 4. Flow across the interventricular septum Systolic Murmurs Early Systolic murmurs 1. Acute severe mitral regurgitation – decrescendo murmur – best heard at apical impulse – Caused by: i. Papillary muscle rupture ii. Infective endocarditis iii. Rupture of the chordae tendineae iv. Blunt chest wall trauma 2. Congenital, small muscular septal defect 3. Tricuspid regurg. with normal PA pressures Midsystolic (ejection) murmurs Are the most common kind of heart murmur Are usually crescendo-decrescendo They may be: 1. Innocent common in children and young adults 2. Physiologic can be detected in hyperdynamic states e.g. anemia, pregnancy, fever, and hyperthyroidism 3. Pathologic are secondary to structural CV abnormalities e.g. Aortic stenosis, Hypertrophic cardiomyopathy, Pulmonic stenosis Pansystolic (Holosystolic) Murmurs Are pathologic Murmur begins immediately with S1 and continues up to S2 1. Mitral valve regurgitation – Loudest at the left ventricular apex – Radiation reflects the direction of the regurgitant jet i. To the base of the heart = anterosuperior jet (flail posterior leaflet) ii. To the axilla and back = posterior jet (flail anterior leaflet – Also usually associated with a systolic thrill, a soft S3, and a short diastolic rumbling (best heard in left lateral decubitus 2. Tricuspid valve regurgitation 3. Ventricular septal defect Diastolic Murmurs Almost always indicate heart disease Two basic types: 1. Early decrescendo diastolic murmurs – signify regurgitant flow through an imcompetent semilunar valve e.g. aortic regurgitation 2. Rumbling diastolic murmurs in mid- or late diastole – suggest stenosis of an AV valve e.g. mitral stenosis Diastolic Murmurs Continuous Murmurs Begin in systole, peak near s2, and continue into all or part of diastole. 1. Cervical venous hum – Audible in kids; can be abolished by compression over the IJV 2. Mammary souffle – Represents augmented arterial flow through engorged breasts – Becomes audible during late 3rd trimester and lactation 3. Patent Ductus Arteriosus – Has a harsh, machinery-like quality 4. Pericardial friction rub – Has scratchy, scraping quality Back to the Basics 1. When does it occur - systole or diastole 2. Where is it loudest - A, P, T, M I. Systolic Murmurs: 1. Aortic stenosis - ejection type 2. Mitral regurgitation - holosystolic 3. Mitral valve prolapse - late systole II. Diastolic Murmurs: 1. Aortic regurgitation - early diastole 2. Mitral stenosis - mid to late diastole SUMMARY A. Presystolic murmur – Mitral/Tricuspid stenosis B. Mitral/Tricuspid regurg. C. Aortic ejection murmur D. Pulmonic stenosis (spilling through S20 E. Aortic/Pulm. diastolic murmur F. Mitral stenosis w/ Opening snap G. Mid-diastolic inflow murmur H. Continuous murmur of PDA Summary Innocent murmurs Characteristics of Pathologic Murmurs Signs and symptoms of cardiovascular diseases Common Cardiac Symptoms Chest Pain Dyspnoea Tachycardia Fatigue Syncope Dizziness Cyanosis Oedema Cough Haemoptysis Appetite & weight loss Hoarseness Nausea & Vomiting Nocturia Chest Pain Localization Radiation Character Duration Precipitating factors Alleviating factors Accompanying findings Dyspnea The sensation of breathlessness or inadequate breathing. Most common complaint of patients with cardiopulmonary diseases Shortness of breath, breathlessness Uncomfortable/abnormal breathing Dyspnea Hyperventilation: Increase in respiratuary workload – Hypoxemia – Hypercapnia – Acidosis Hypoventilation:Decrease in ventilation capacity – COPD Cyanosis Cyanosis is a bluish or purplish tinge to the skin and mucous membranes. Approximately 5 g/dL of unoxygenated hemoglobin in the capillaries generates the dark blue color appreciated clinically as cyanosis Peripheral cyanosis Peripheral cyanosis is a dusky or bluish tinge to the fingers and toes and may occur with or without central cyanosis (ie, with or without hypoxemia). When unaccompanied by hypoxemia, as determined by blood gas analysis, peripheral cyanosis is caused by peripheral vasoconstriction Causes All common causes of central cyanosis Arterial obstruction Cold exposure (due to vasoconstriction) Raynaud's phenomenon (vasoconstriction) Reduced cardiac output (e.g. heart failure, hypovolaemia) Vasoconstriction Venous obstruction (e.g. deep vein thrombosis) Central cyanosis Central cyanosis is often due to a circulatory or ventilatory problem that leads to poor blood oxygenation in the lungs or greater oxygen extraction due to slowing down of blood circulation in the skin's blood vessels. 1. Central Nervous System: – Intracranial hemorrhage – Cerebral anoxia – Drug overdose (e.g. Heroin ) 2. Respiratory System: – Bronchiolitis – Bronchospasm (e.g. Asthma) – Lung disease – Pulmonary embolism – Hypoventilation 3.Cardiac Disorders: – Congenital heart disease (e.g. Tetralogy of Fallot, Right to left shunts in heart or great vessels) – Heart failure – Heart valve disease – Myocardial infarction 4.Blood: – Methemoglobinemia – Polycythaemia 5.Others: – High altitude – Hypothermia – Congenital cyanosis Differential cyanosis Differential cyanosis, meaning cyanosis and clubbing of the lower extremities with normal upper extremity nailbeds, is diagnostic of patent ductus arteriosus with pulmonary hypertension Differential cyanosis Desaturated blood from the ductus enters the aorta distal to the left subclavian artery, sparing the brachiocephalic circulation. The oral mucosa and tongue receive saturated blood and are not cyanotic. In some cases, ductal flow will enter the left subclavian artery and cause clubbing of the left hand as well as the feet. Differential Diagnosis of Chest Pain / Göğüs Ağrısının Ayırıcı Tanısı Nonkardiyak intratorasik dokular / Noncardiac intrathorasic tissues Boyun & “göğüs duvarı” dokuları / Neck & “chest wall” tissues Subdiafragmatik organlar / Subdiaphragmatic organs Differential Diagnosis of Dyspnoea Cardiac Pulmonary Chest wall abnormalities Anemia Obesity Hypoxia Physicogenic Central nervous system Cardiac Dyspnoea Exertional Dyspnoea Orthopnoea Paroxysmal nocturnal dyspnoea Pulmonary oedema Cheyne-Stokes ventilation Systemic Diseases that may lead to Heart Diseases Endocrine System Diseases Collagen Tissue Disorders Haematologic Diseases Metabolic Disorders Infectious Diseases Chromosome Abnormalities Malign Disorders Muscle Diseases