* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Innate cellular responses to rotavirus infection
Hygiene hypothesis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Neonatal infection wikipedia , lookup
Immune system wikipedia , lookup
DNA vaccination wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Infection control wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Hepatitis B wikipedia , lookup
Gastroenteritis wikipedia , lookup
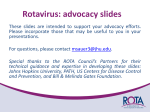
Journal of General Virology (2013), 94, 1151–1160 DOI 10.1099/vir.0.051276-0 Innate cellular responses to rotavirus infection Review Gavan Holloway and Barbara S. Coulson Correspondence Department of Microbiology and Immunology, The University of Melbourne, Victoria 3010, Australia Gavan Holloway [email protected] Received 8 January 2013 Accepted 9 March 2013 Rotavirus is a leading cause of severe dehydrating diarrhoea in infants and young children. Following rotavirus infection in the intestine an innate immune response is rapidly triggered. This response leads to the induction of type I and type III interferons (IFNs) and other cytokines, resulting in a reduction in viral replication. Here we review the current literature describing the detection of rotavirus infection by pattern recognition receptors within host cells, the subsequent molecular mechanisms leading to IFN and cytokine production, and the processes leading to reduced rotavirus replication and the development of protective immunity. Rotavirus countermeasures against innate responses, and their roles in modulating rotavirus replication in mice, also are discussed. By linking these different aspects of innate immunity, we provide a comprehensive overview of the host’s first line of defence against rotavirus infection. Understanding these processes is expected to be of benefit in improving strategies to combat rotavirus disease. Introduction Rotavirus, a double-stranded RNA (dsRNA) virus of the family Reoviridae, is the main aetiological agent of severe dehydrating diarrhoea in infants worldwide. By 2008 estimates, rotavirus causes approximately 453 000 deaths annually in children younger than 5 years of age, mostly in developing countries (Tate et al., 2012). Evidence is accumulating that innate immune responses are critical as a first line of defence, limiting rotavirus replication and disease in the host (Angel et al., 2012; Broquet et al., 2011; Pott et al., 2011, 2012; Sen et al., 2012). In addition, innate responses are potentially important for the intensity and longevity of adaptive responses, as demonstrated with other host–virus models (Cervantes-Barragan et al., 2012; Kasturi et al., 2011). Two recently licensed live rotavirus vaccines, Rotateq and Rotarix, have been effective in reducing severe rotavirus disease and the need for hospitalizations in many settings (Richardson et al., 2011; Vesikari, 2012). However, reduced vaccine efficacy in developing countries, the potential lack of coverage for all serotypes and lingering concerns over the rare side effect of gut intussusception highlight the need for improved vaccines (Lopman et al., 2012; Patel et al., 2011). Therefore, it is crucial to investigate innate responses to rotavirus infection and to obtain a clear picture of rotavirus pathogenesis and the processes contributing to effective immunity. Here, we summarize what has been learned so far about innate immune responses and how innate immunity pathways are triggered following rotavirus infection. Properties of type I, II and III interferons (IFNs) Type I IFNs, including multiple IFN-a isoforms and IFN-b (IFN-a/b), are a key component of the host defence against 051276 G 2013 SGM viral infection and possess powerful antiviral properties (Randall & Goodbourn, 2008). More recently it has been shown that type III IFNs, including IFN-l1 (IL-29), IFN-l2 (IL-28A) and IFN-l3 (IL-28B), are also important in innate immunity (Donnelly & Kotenko, 2010; Kotenko et al., 2003). In general, following detection of viruses within the host, activation of the IFN response factors (IRF) 3 and IRF7 is primarily responsible for the induction of IFN types I and III (Fig. 1). Following secretion from infected cells, IFN-a/b and IFN-l bind to their specific receptors, IFN-a/b receptor (IFNa/bR) and IFN-l receptor (IFN-lR), respectively, on surrounding uninfected and infected cells. While IFN-a/bR is expressed almost ubiquitously, IFN-lR is expressed primarily on epithelial cells (Donnelly & Kotenko, 2010). Activation of the IFN-a/bR or IFN-lR induces a signalling cascade involving JAK and TYK kinases that culminates in the activation of signal transducer and activator of transcription (STAT) 1 and STAT2. Heterodimers of STAT1 and STAT2 associate with IRF9 to form a complex known as IFN stimulated gene factor 3 that induces expression of IFN stimulated genes (ISGs), many of which have the ability to directly inhibit replication of specific viruses (de Veer et al., 2001; Randall & Goodbourn, 2008). STAT1 also forms homodimers that can stimulate expression of a subset of ISGs. IFN-c, the only member of the type II IFN class, is produced by several activated immune cell types and signals largely through STAT1. Therefore, in addition to its important immunostimulatory and immunomodulatory roles, IFN-c has antiviral properties (Randall & Goodbourn, 2008). IFN-a/b also have important immunomodulatory effects on cells participating in the adaptive immune response, including activation of antigen-presenting dendritic cells (DCs) and expansion and differentiation of antibody-producing B cells and virus-specific T cells (Seo & Hahm, 2010). Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Printed in Great Britain 1151 G. Holloway and B. S. Coulson IFN-λ IFN-α/β RV IFN-α/βR IFN-λR TYK JAK cytoplasm RV endosome mitochondrion dsRNA TLR3 RIG-1 ssRNA dsRNA TRIF IκB NSP1 STAT1 MDA5 STAT2 ISG products STAT1 RV NSP1 NF-κB RV replication IRF9 IRF3/7 β-TrCP MAVS STAT1 RV ? viroplasm p38 RV JNK proteasome ER JNK p38 nucleus NF-κB IRF3/7 STAT1 NF-κB IFN-α/β/λ AP-1 STAT2 ISG IL-8 IRF9 Fig. 1. Detection of rotavirus infection and induction of innate responses in intestinal epithelial cells. Following rotavirus (RV)cell entry, melanoma differentiation-associated protein 5 (MDA5) and retinoic acid-inducible gene-I (RIG-I) detect single- or double-stranded viral RNA (ssRNA/dsRNA – precise ligand unknown) and signal through mitochondrial antiviral signalling protein (MAVS) to stimulate the activation of IFN response factors 3 and 7 (IRF3/7) and IFN-a/b/l expression. Nuclear factorkB (NF-kB) and activator protein-1 (AP-1, via JNK/p38) also are activated by rotavirus infection, but a role for RIG-I/MDA5/ MAVS in this process has not been experimentally verified. These transcription factors play a role in the induction of IFN and other cytokines such as IL-8. An alternative pathway of rotavirus detection by TLR3 and its adaptor TIR-domain-containing adaptor-inducing IFN-b (TRIF) has been demonstrated in adult mice, also leading to IRF3/7 activation and IFN expression. The protective effects of secreted IFN-a/b/l are mediated by autocrine/paracrine stimulation of the IFN-a/b and IFN-l receptors (IFN-a/bR and IFN-lR), leading to STAT1/2 activation, IFN stimulated gene (ISG) expression and inhibition of rotavirus replication by an unidentified mechanism. Cytokine/chemokine expression is likely to result in attraction and activation of immune cells. Rotavirus non-structural protein 1 (NSP1) can reduce IFN expression by degrading IRF3/7. NF-kB activation is also inhibited by certain rotavirus strains through NSP1 degradation of b-transducin repeat-containing protein (b-TrCP), a component required for inhibitor of kB (IkB) degradation. Rotavirus infection also prevents the nuclear accumulation of activated STAT1/2 by the action of an unidentified viral component (RV?). Note: dotted arrow lines indicate signalling events not verified to occur during rotavirus infection. Some pathway intermediates have been omitted for clarity. Mechanisms leading to IFN induction during rotavirus infection The induction of IFN-a/b and IFN-l occurs when viral components are recognized by the infected cell. For many viruses, the major component recognized by the host cell is nucleic acid, including genomic RNA, mRNA and RNA 1152 replication intermediates. Depending on its form, cellular localization and chemical modification, viral RNA can be detected in the host cell by several proteins. These include the cytoplasmic RNA sensors retinoic acid-inducible gene-I (RIG-I) and melanoma differentiation-associated gene 5 (MDA5), and the endosomal RNA sensors toll-like Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Journal of General Virology 94 Innate responses to rotavirus receptor 3 (TLR3), TLR7 and TLR8 (Jensen & Thomsen, 2012). Upon ligand binding, RIG-I and MDA5 signal through the mitochondrial antiviral sensor protein (MAVS or IPS-1), which leads to the activation, through several intermediates, of IRF3/7 and subsequent IFN-a/b and IFN-l expression. TLR3 signals through the TIR-domain-containing adaptor-inducing IFN-b (TRIF), while TLR7 and TLR8 signal through myeloid differentiation primary response 88 (MyD88), leading also to IRF activation and IFN expression. Recent evidence suggests that both MDA5 and RIG-I contribute to the recognition of rotavirus in infected intestinal epithelial cell (IEC) lines and the subsequent induction of type I IFN (Fig. 1). MDA5 and RIG-I were found to play significant and complementary roles in IFNb induction by rotavirus in IEC lines, and to be mutually redundant in mouse embryonic fibroblasts (Broquet et al., 2011; Hirata et al., 2007; Sen et al., 2011). Furthermore, adult mice lacking MAVS supported significantly greater rhesus rotavirus (RRV) and simian SA11 rotavirus replication compared to wild-type animals (Broquet et al., 2011). It appeared that TLR3 and its adaptor TRIF played no part in IFN-b induction in IECs from RRV-infected adult mice in this study, and rotavirus intestinal replication and faecal shedding were unaffected in TLR3-deficient mice. Notably, a recent study showed that TLR3 and its adaptor TRIF are required for induction of IFN-b by epizootic diarrhoea of infant mice (EDIM) rotavirus infection in adult but not infant mice, consistent with the increase in TLR3 expression as mice age (Fig. 1) (Pott et al., 2012). In the same study rotavirus replication was enhanced when TLR3 was absent from the non-haematopoietic cell compartment, suggesting involvement of TLR3 expressed in IECs. The reasons for the inconsistency between reports examining a role for TLR3 in rotavirus infection are not clear, but the different experimental outcomes may be due to the high replication capacity in mice of the homologous EDIM compared to the heterologous RRV and SA11. RIG-I can detect short to medium length dsRNA (from 21 b to ~1 kb) while MDA5 recognizes long dsRNA (.1 kb) (Kato et al., 2008; Marques et al., 2006). As rotavirus genomic dsRNA segments range from 0.5 to 3.2 kb, it seems reasonable to speculate that rotavirus dsRNA is the ligand of RIG-I and MDA5 in infected intestinal cells, although this has not been formally demonstrated. This is consistent with the observation that rotavirus dsRNA is present in the cytoplasm of infected cells, although this is not necessarily genomic dsRNA and may be singlestranded RNA with stretches of dsRNA secondary structure (Li et al., 2010; Rojas et al., 2010). In addition, delivery of rotavirus dsRNA or the dsRNA analogue polyinosinepolycytidylic acid into the cytoplasm of IEC lines or mouse embryonic fibroblasts can induce an IFN response (Hirata et al., 2007; Sen et al., 2011). However, it is unclear how detection of rotavirus dsRNA occurs during infection, given that dsRNA is synthesized in intact double-layered particles (Silvestri et al., 2004). http://vir.sgmjournals.org RIG-I also is potently activated by dsRNA and singlestranded RNA containing a 59-triphosphate moiety that is produced by some viral RNA polymerases. The 59 end of the plus-sense strand of rotavirus dsRNA contains a 59triphosphate that is capped by the viral methyl-guanylyl transferase viral protein 3 (VP3), likely providing protection from recognition by RIG-I in a manner similar to selfmRNA (Hornung et al., 2006; Imai et al., 1983; Pizarro et al., 1991). However, if capping is not completely efficient then rotavirus plus-sense RNA could be an activating ligand for RIG-I. It has been reported that MDA5 also can be activated by complex mRNA secondary structure that could also be present in rotavirus mRNA (Li et al., 2010; Pichlmair et al., 2009). As rotavirus plus-sense RNA message must be present in the cytoplasm for protein synthesis to occur, it seems plausible that this might be the activating ligand for RIG-I/MDA5. The identity of the molecular activators of RIG-I and MDA5 during rotavirus infection remains to be established. IFN expression during rotavirus infection It is now clear that rotaviruses have evolved a strategy to limit the expression of type I IFN in infected cells, through the ability of the non-structural protein 1 (NSP1) to bind IRF3, 5 and 7 and mediate their degradation by the proteasome (Fig. 1) (Barro & Patton, 2005, 2007; Graff et al., 2002). This topic has been the subject of several reviews and therefore will not be discussed here in detail (Arnold & Patton, 2009; Liu et al., 2009; Sherry, 2009). The ability to reduce IFN-a/b expression appears to be reasonably well conserved amongst rotavirus strains, although there is some variability in the IRF subtypes targeted (Arnold & Patton, 2011). As IRF activation is important for IFN-l expression, it is highly probable that IFN-l also would be negatively regulated by rotavirus NSP1. NSP1 from some rotavirus strains is unable to degrade IRF from all host species, most likely due to divergent IRF sequences, which may play a role in restricting host range (Feng et al., 2009; Sen et al., 2009). Despite the ability of rotavirus NSP1 to mediate the degradation of IRFs, many studies have shown that IFN-a/ b are still expressed in substantial amounts during rotavirus infection in vivo and in cell culture. For example, early induction of intestinal and serum IFN-a/b was observed in newborn calves infected with bovine rotavirus, and elevated serum IFN-a/b can be detected in children with rotavirus gastroenteritis (De Boissieu et al., 1993; La Bonnardiere et al., 1981). Infection of the IEC line HT-29 with RRV, a virus that effectively targets IRF3 and 7 for degradation, can also induce substantial levels of IFN-a/b (Frias et al., 2010). Rotavirus cannot completely inhibit the IFN response in mice, as less virus replication is observed in wild-type mice compared to genetically modified mice with impaired IFN responses (Broquet et al., 2011; Sen et al., 2012). These examples illustrate that although rotavirus can restrict IFN production, sufficient IFN is Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 1153 G. Holloway and B. S. Coulson still produced to impact on rotavirus replication. IECs are a likely source of IFN-a/b and IFN-l during rotavirus infection, either before IFN induction is switched off by NSP1 or when IRF degradation has been incomplete. Immune cells such as DCs that have taken up virus but are not productively infected and do not express NSP1 also may produce IFN-a/b in response to rotavirus exposure (Deal et al., 2010). Interestingly, it was reported that IFN expression is suppressed in the IECs of mice infected with murine rotavirus and the majority of intestinal IFN-a/ b is produced in haematopoietic cells (Sen et al., 2012). Like many viruses, rotavirus can reduce the impact of IFN by inhibiting IFN signalling (Randall & Goodbourn, 2008). This occurs through an unknown mechanism that prevents the nuclear accumulation of activated STAT1 and STAT2 (Fig. 1) (Holloway et al., 2009). This finding supports the concept that reduction of IFN production alone is not sufficient for rotavirus to effectively evade innate immunity. Sensitivity of rotavirus to IFN The observations that rotaviruses actively limit IFN-a/b induction and signalling suggest that infection by these viruses is sensitive to the effects of IFN-a/b. Varying levels of sensitivity have been reported, which may be a reflection of differences in rotavirus strain, host species or experimental methods. IFN-a treatment was found to protect newborn calves against severe rotavirus disease, but not virus shedding (Schwers et al., 1985). Both high and low sensitivities of bovine rotavirus infection to bovine IFN-a/b have been reported from cell culture studies (Derbyshire, 1989; La Bonnardiere et al., 1980). However, much evidence suggests that rotaviruses are only moderately sensitive to IFN-a/b. In the Caco-2 and HT-29 human IEC lines, a human rotavirus and RRV showed approximately 1-log reductions in infectivity following a long (3 day) pre-treatment with IFN-a (Bass, 1997). Short pre-treatment with IFN-a, even at high concentrations, had little effect on virus growth. In the MA104 monkey kidney epithelial cell line, in which IFNa/b signalling is intact, rotaviruses are even less sensitive to IFN-a/b (McKimm-Breschkin & Holmes, 1982). Overall, it seems clear that rotavirus is far less sensitive to IFN-a/b than a number of other viruses. For example, the titre of vesicular stomatitis virus grown in cell culture can be reduced up to 6 logs by IFN-a/b pre-treatment (Belkowski & Sen, 1987). The role of IFN in protecting against rotavirus infection in mice has been studied by several groups. In infant and adult mice lacking the IFN-a/bR little or no increased susceptibility to murine rotavirus infection was observed, suggesting that IFN-a/b play only a minor role in controlling homologous rotavirus replication in vivo (Angel et al., 1999; Pott et al., 2011). Supporting this finding, oral or intraperitoneal administration of IFN-a/b did not delay or diminish diarrhoeal symptoms in mice 1154 infected with murine rotavirus (Angel et al., 1999). Rotavirus replication in mice deficient in IFN-c also is not enhanced (Franco et al., 1997). In STAT1-deficient infant mice RRV replicated much more efficiently and caused systemic disease; but murine rotaviruses showed, at most, modest increases in replication (Feng et al., 2008; Sen et al., 2012; Vancott et al., 2003). However, large increases in RRV and murine EDIM rotavirus intestinal replication were observed in adult STAT1-deficient mice (Vancott et al., 2003). These results suggest that in mice, homologous rotavirus is less sensitive to IFN than heterologous rotavirus. A recent report provides evidence that signalling through STAT1, but not the IFN-a/b receptor, is important in limiting murine rotavirus replication. It was shown that IFN-l is important for controlling rotavirus replication in the mouse intestine (Pott et al., 2011). In mice lacking IL-28Ra, an essential component of the IFN-lR, murine rotavirus EDIM replication was markedly increased compared to control animals (Pott et al., 2011). In the same study, mice lacking the IFN-a/bR supported a much smaller increase in EDIM replication. It was shown that, despite intestinal induction of both IFN-a/b and IFN-l by rotavirus, the subsequent expression of ISGs in IECs was mostly dependent upon IFN-l signals. This was possibly due to the ability of polarized IECs to respond to basolaterally applied IFN-l but not IFN-a/b, although this was demonstrated only in cell culture. Importantly, injection of IFN-l was highly effective in protecting mice from rotavirus infection while IFN-a was only partially protective (Pott et al., 2011). Further study is required to determine the exact nature of IFN-l action against rotavirus and whether IFN-l is important in limiting rotavirus infection in humans and other animals. Another recent study showed that the absence of STAT1 does not confer a further growth advantage for murine rotavirus EW strain over IFN-a/bR and IFN-c receptor (IFN-cR) deficient mice (Sen et al., 2012). This would seem to suggest IFN-l is not important in controlling homologous rotavirus infection in mice. However, as EW replication was analysed early in infection, a possible caveat is that differences later in replication were missed. This study does, however, support a modest role for IFN-l in suppressing the early replication of heterologous RRV in mice. While some inconsistencies have been reported regarding the role of IFN in controlling rotavirus infection in mice, it seems likely that IFN-a/b and IFN-l play important roles in limiting rotavirus replication. It also appears that the ability of the rotavirus strain being tested to evade innate immune responses may be correlated with the level of sensitivity to IFN, as appears to be the case when comparing nonhomologous and homologous rotavirus infection in mice (Sen et al., 2012). The role of NSP1 and possibly other rotavirus proteins in conferring replicative advantages in mice is an important area that could be studied using reassortant rotaviruses. Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Journal of General Virology 94 Innate responses to rotavirus The role of IFN-induced antiviral proteins in controlling rotavirus infection The protective effects of type I and III IFNs against rotavirus infection are likely to be mediated through the induction of ISGs with antiviral properties (Fig. 1). To date, little evidence of specific antiviral protein activity against rotavirus has been reported. Interestingly, pretreatment of cells with UV-inactivated rotavirus and IFNa/b suppresses rotavirus infection to a greater extent than IFN treatment alone, suggesting antiviral proteins activated by dsRNA may be able to limit rotavirus replication (McKimm-Breschkin & Holmes, 1982). These include the dsRNA-activated protein kinase R that causes host cell translational shut off through phosphorylation of eukaryotic initiation factor-2a, and 29,-59-oligoadenylate synthetase, which activates RNase L leading to viral and cellular mRNA degradation (Randall & Goodbourn, 2008). However, one report provides evidence that protein kinase R, although activated, cannot inhibit rotavirus protein synthesis during infection of mouse embryonic fibroblasts or MA104 cells (Rojas et al., 2010). The identification of ISG products with anti-rotavirus activity will provide insight into the stages of the replication cycle at which rotavirus is vulnerable and may give clues to aid new therapeutic strategies. However, this may prove challenging due to possible redundancy among ISGs that can target rotavirus, and the relatively low sensitivity of rotavirus infection to IFN, which may be due to direct interference with one or more ISG products able to target rotavirus. Rotavirus-induced cytokine induction and the role of nuclear factor-kB (NF-kB) In addition to IFN, the induction of numerous cytokines is an important part of the innate response in virus-infected cells. While some cytokines are produced in many cell types including IECs, others including TNF and IL-1b are largely restricted to haematopoietic cells. Key roles of cytokines are to attract immune cells by chemotaxis and to activate their effector functions. Some cytokines, including TNF, also have been reported to possess antiviral properties (Bartee et al., 2009). Expression of many cytokines is heavily dependent on the activation of the transcription factor NF-kB following detection of viral components within the host cell. Initial studies of cytokine induction by rotavirus utilized IEC line infection models. In HT-29 cells a robust induction of the chemokine IL-8 was observed following rotavirus infection (Sheth et al., 1996). IL-8 is a potent attractor of neutrophils, and while evidence of an intestinal neutrophil infiltrate has been observed in bird and lamb rotavirus infection models, whether neutrophil recruitment to sites of rotavirus infection plays a role in viral clearance in humans is unknown (Snodgrass et al., 1977; Yason et al., 1987). The induction of IL-8 by rotavirus was found to be caused by NFkB activation and binding to the IL-8 promoter (Casola et al., 2002; Rollo et al., 1999). In contrast to HT-29 cells, IL-8 http://vir.sgmjournals.org induction following rotavirus infection of Caco-2 cells was low despite the capacity of this cell line to produce this chemokine, at least at the mRNA level, in response to other viral infections (Casola et al., 1998; Rodrı́guez et al., 2009; Spiegel & Weber, 2006). In addition to IL-8, several other cytokines and chemokines that at least partially rely on NFkB for their induction have been detected in IEC lines and mouse intestines following rotavirus infection. These include RANTES, GM-CSF, GRO-a, MIP-1b and IP-10 (Casola et al., 1998; Rollo et al., 1999). These secreted molecules can attract various immune cells including T cells, DCs and monocytes but the relative importance of each chemokine in immune responses to rotavirus is unknown (Stadnyk, 2002). Due to the importance of NF-kB activation in cytokine induction, many viruses have evolved strategies to actively limit NF-kB activation (Randall & Goodbourn, 2008). It was found that some rotavirus strains can inhibit the activation of NF-kB by the NSP1-mediated degradation of b-transducin repeat-containing protein (b-TrCP), which is required for the degradation of inhibitor of kB to allow the subsequent release of active NF-kB (Fig. 1) (Graff et al., 2009). Molecular analysis has suggested that NSP1 from porcine OSU and bovine NCDV rotaviruses can degrade b-TrCP but the NSP1 molecules of most rotavirus strains including RRV lack this ability (Arnold & Patton, 2011). We have found that the human rotavirus Wa strain is very efficient at blocking NFkB nuclear translocation, while RRV infection at a high m.o.i. can also block NF-kB (Holloway et al., 2009). For these viruses the mechanism of inhibition has not been defined and is potentially NSP1-independent. The full extent of NFkB inhibition by rotavirus and its impact upon cytokine expression require further investigation. NF-kB is important for the induction of IFN-l and IFN-b, but not IFN-a subtypes, many of which require IRF7 (Lenardo et al., 1989; Siegel et al., 2011). IRF7 is not constitutively expressed in most cell types, where an IFN-b signal is required for its induction. Therefore, the rotaviruses that can inhibit NF-kB may be able to limit the induction of both IFN-b and other IFN types (Arnold & Patton, 2011; Graff et al., 2009). Signalling through MAVS, via the recruitment of signalling intermediates including TNF receptor-associated factors (TRAFs) and TANK-binding kinase 1, can activate NF-kB (Fig. 1). However, it is unclear whether NF-kB activation in IECs following infection with rotavirus occurs primarily through MAVS. Other mechanisms of NF-kB activation have been proposed, such as the interaction of cytoplasmic rotavirus VP4 protein with cellular TRAF-binding proteins (LaMonica et al., 2001), and the action of NSP1 (Bagchi et al., 2010). UV-inactivated rotavirus can activate NF-kB and induce IL-8 expression, although with much less efficiency than replicating rotavirus, demonstrating that replication is required for efficient NF-kB-driven cytokine expression in intestinal cells (Casola et al., 1998; Frias et al., 2010; Holloway & Coulson, 2006; Rollo et al., 1999). The kinases Jun N-terminal kinase (JNK) and p38 are activated during rotavirus infection of epithelial cells and Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 1155 G. Holloway and B. S. Coulson play a role in IL-8 induction due to their ability to activate the activator protein-1 transcription factor that can stimulate IL-8 expression (Fig. 1) (Casola et al., 2002; Holloway & Coulson, 2006). MAVS-dependent activation of JNK and p38 has been demonstrated, although such a link has not been shown during rotavirus infection (Mikkelsen et al., 2009; Seth et al., 2005). MAVSindependent activation of JNK and p38 through the unfolded protein response is also possible, and it is known that this process is triggered during rotavirus infection (Kim et al., 2009; Trujillo-Alonso et al., 2011). Rotavirus interactions with innate immune cells, and their effects on adaptive immunity and rotavirus disease DCs are uniquely equipped to rapidly produce high levels of type I IFN and pro-inflammatory cytokines when encountering viruses. When combined with their ability to present antigen and activate T and B cells, these properties endow DCs with a pivotal ability to connect the innate and adaptive arms of the antiviral immune response. Of particular relevance to rotavirus infection, priming by DCs from the small intestine, Peyer’s patches and mesenteric lymph nodes promotes the expression of guthoming receptors on B and T cells (Soloff & Barratt-Boyes, 2010). These homing cells are crucial for resolution of murine rotavirus infection and protection against reinfection (Rosé et al., 1998; Weitkamp et al., 2005; Youngman et al., 2002). Although a single correlate of protection against rotavirus disease in humans has not been identified (Desselberger & Huppertz, 2011), several studies implicate rotavirus-specific serum IgA levels, which can reflect intestinal IgA production, or intestinal IgA itself (Brown et al., 2000; Coulson et al., 1992; Franco et al., 2006; Hjelt et al., 1987). However, rotavirus-specific serum IgA levels may not be an optimal correlate of protection following vaccination, particularly in developing countries (Angel et al., 2012). In mice, intestinal anti-rotavirus antibody is the primary effector of protection, whereas both specific T cells and IgA are important for virus clearance (Feng et al., 2008). Additionally, several DC subsets responding to RRV infection in neonatal mice together activate natural killer cells and stimulate T cell proliferation, leading to bile duct inflammation and damage, and experimental biliary atresia (Saxena et al., 2011). In diabetes-prone mice, DCs activated by RRV infection in the mesenteric and pancreatic lymph nodes also may play a role in RRV-mediated acceleration of type 1 diabetes onset (Pane et al., 2013). Several groups have sought to delineate the interactions between DCs and rotaviruses. The activation and maturation of cultured human myeloid DCs and mouse bone marrowderived DCs have been observed following exposure to rotavirus (Douagi et al., 2007; Istrate et al., 2007; Narváez et al., 2005). DCs in Peyer’s patches from rotavirus-infected mice also showed similar signs of activation and cytokine induction (Lopez-Guerrero et al., 2010). Exposure of human plasmacytoid DCs (pDCs) to RRV led to virus replication, as 1156 measured by NSP2 expression, in approximately 1–2 % of cells so the great majority of pDC are refractory to productive infection (Deal et al., 2010). Exposure of these pDC to live or inactivated rotavirus induced the expression of IFN-a, IFN-b and numerous cytokines including TNF-a, IL-6, IL-8, IP-10, MIP-1a, MIP-1b and RANTES, indicating that in contrast to IECs, rotavirus replication is not required for NF-kB activation in pDCs. Cytokine expression also required the presence of rotavirus genomic dsRNA. Notably, the small proportion of pDCs expressing high levels of rotavirus antigen showed reduced IFN-a expression, providing evidence that RRV can effectively antagonize IFN induction in productively infected cells. This was likely due to NSP1mediated degradation of IRF7, the main regulator of IFN production by pDC (Deal et al., 2010). An earlier study also showed that rotavirus-exposed human pDCs express IFN-a and, at least in whole peripheral blood mononuclear cell (PBMC) cultures, these cells were found to be required for the efficient stimulation of IFN-c-expressing, rotavirusspecific memory T cells (Mesa et al., 2007). Supporting a role for DCs during rotavirus infection, an unidentified immune cell type was shown to be the source of most of the IFN-a/b produced in mouse intestine following infection with murine rotavirus (Sen et al., 2012). Interestingly, in mice lacking the IFN-a/bR and IFN-cR, early type I IFN expression is markedly reduced, suggesting an IFN feedback mechanism is required for the IFN response (Sen et al., 2012). The processes of entry of rotavirus into pDCs and induction of IFN-a/b are not entirely clear. Activation of pDCs, at least by RRV, appears to rely on typical receptormediated entry, as it is inhibited by non-neutralizing antiVP7 antibodies (Deal et al., 2010). However, pDC activation requires endosomal acidification, which is not considered to be required for RRV entry into epithelial cells (Wolf et al., 2011). This suggests that TLR7, the primary endosomal sensor of viral RNA in pDCs, triggers IFN-a/b expression following pDC exposure to RRV (Gilliet et al., 2008). It remains to be determined which DC subtypes are important for controlling rotavirus replication in vivo and how virus recognition occurs within these cells. In addition to DCs, macrophages also play an important role in innate sensing and clearance of some viruses (Karupiah et al., 1996; Kumagai et al., 2007). Intestinal macrophage numbers in gnotobiotic pigs were found to increase dramatically following rotavirus infection (Zhang et al., 2008). Infected macrophages in mouse tissues, including Peyer’s patches, mesenteric lymph nodes and pancreas, also have been occasionally observed (Brown & Offit, 1998; Graham et al., 2007). The macrophage cell line RAW264.7 can be infected with rotavirus, which leads to expression of IFN-a/b, TNF and MIP-2, an attractor of neutrophils (Mohanty et al., 2010). The role of macrophages in innate control of rotavirus infection and activation of the adaptive immune response is an important question for future studies. Limited information is available on the role of innate responses in the development of adaptive immunity to Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Journal of General Virology 94 Innate responses to rotavirus rotavirus. While IFN induction and signalling are required to reduce viral loads, the absence of IFN signalling does not increase the time taken for viral clearance (Angel et al., 1999; Broquet et al., 2011; Pott et al., 2011; Vancott et al., 2003). In addition, the anti-rotavirus intestinal IgA response, a good correlate of virus clearance, is normal in STAT1-deficient mice, suggesting IFNs are not required for the adaptive immune response to rotavirus (Vancott et al., 2003). It was also found that IFN signalling during an initial rotavirus infection does not appear to play a role in protection from viral shedding during subsequent challenge in mice (Vancott et al., 2003). A lack of dependence on IFN for clearance of respiratory syncytial virus also has been observed (Durbin et al., 2002). These findings are not entirely consistent with other experimental models where IFN-a/b are crucial in enhancing DC maturation and T and B cell responses (Fitzgerald-Bocarsly & Feng, 2007). More work is needed to further assess the role of innate responses in enhancing the quality of short- and longer-term adaptive immune response to rotavirus infection. Conclusions and perspectives Continuing study of innate responses to rotavirus is fundamental to our greater understanding of rotavirus pathogenesis and immunity. Inroads already have been made in many areas, including the mechanisms behind rotavirus recognition by infected IECs and the blockade of IFN induction by rotavirus NSP1. Studies of the role of IFN in controlling rotavirus infection in the mouse model are also providing valuable information. The role of specialized innate immune cells, such as DCs, is likely to prove crucial in the control of RV replication in vivo and is worthy of further attention. In some studies, innate responses in IECs appear less important than those in immune cells due to the strong suppression of innate responses by particular homologous rotavirus strains. Therefore careful use of rotavirus strains, including reassortants that differ in their abilities to suppress innate immunity, will also provide insights into how rotaviruses have evolved to evade the host response. Processes that are likely to be important in rotavirus control but remain largely unexplored include the expression of chemokines, their role in attracting immune cells and the ability of different rotavirus strains to inhibit their expression. The role of ISG products in repressing rotavirus replication, and viral measures to counteract these antiviral proteins, are also important areas for future study. When taken together, these insights into the various aspects of innate immunity to rotavirus may allow the design of improved live-attenuated vaccines, non-live vaccines and novel therapeutics against rotavirus. References Angel, J., Franco, M. A., Greenberg, H. B. & Bass, D. (1999). Lack of a role for type I and type II interferons in the resolution of rotavirusinduced diarrhea and infection in mice. J Interferon Cytokine Res 19, 655–659. Angel, J., Franco, M. A. & Greenberg, H. B. (2012). Rotavirus immune responses and correlates of protection. Curr Opin Virol 2, 419–425. Arnold, M. M. & Patton, J. T. (2009). Rotavirus antagonism of the innate immune response. Viruses 1, 1035–1056. Arnold, M. M. & Patton, J. T. (2011). Diversity of interferon antagonist activities mediated by NSP1 proteins of different rotavirus strains. J Virol 85, 1970–1979. Bagchi, P., Dutta, D., Chattopadhyay, S., Mukherjee, A., Halder, U. C., Sarkar, S., Kobayashi, N., Komoto, S., Taniguchi, K. & ChawlaSarkar, M. (2010). Rotavirus nonstructural protein 1 suppresses virus-induced cellular apoptosis to facilitate viral growth by activating the cell survival pathways during early stages of infection. J Virol 84, 6834–6845. Barro, M. & Patton, J. T. (2005). Rotavirus nonstructural protein 1 subverts innate immune response by inducing degradation of IFN regulatory factor 3. Proc Natl Acad Sci U S A 102, 4114–4119. Barro, M. & Patton, J. T. (2007). Rotavirus NSP1 inhibits expression of type I interferon by antagonizing the function of interferon regulatory factors IRF3, IRF5, and IRF7. J Virol 81, 4473–4481. Bartee, E., Mohamed, M. R., Lopez, M. C., Baker, H. V. & McFadden, G. (2009). The addition of tumor necrosis factor plus b interferon induces a novel synergistic antiviral state against poxviruses in primary human fibroblasts. J Virol 83, 498–511. Bass, D. M. (1997). Interferon gamma and interleukin 1, but not interferon alfa, inhibit rotavirus entry into human intestinal cell lines. Gastroenterology 113, 81–89. Belkowski, L. S. & Sen, G. C. (1987). Inhibition of vesicular stomatitis viral mRNA synthesis by interferons. J Virol 61, 653–660. Broquet, A. H., Hirata, Y., McAllister, C. S. & Kagnoff, M. F. (2011). RIG-I/MDA5/MAVS are required to signal a protective IFN response in rotavirus-infected intestinal epithelium. J Immunol 186, 1618– 1626. Brown, K. A. & Offit, P. A. (1998). Rotavirus-specific proteins are detected in murine macrophages in both intestinal and extraintestinal lymphoid tissues. Microb Pathog 24, 327–331. Brown, K. A., Kriss, J. A., Moser, C. A., Wenner, W. J. & Offit, P. A. (2000). Circulating rotavirus-specific antibody-secreting cells (ASCs) predict the presence of rotavirus-specific ASCs in the human small intestinal lamina propria. J Infect Dis 182, 1039–1043. Casola, A., Estes, M. K., Crawford, S. E., Ogra, P. L., Ernst, P. B., Garofalo, R. P. & Crowe, S. E. (1998). Rotavirus infection of cultured intestinal epithelial cells induces secretion of CXC and CC chemokines. Gastroenterology 114, 947–955. Casola, A., Garofalo, R. P., Crawford, S. E., Estes, M. K., Mercurio, F., Crowe, S. E. & Brasier, A. R. (2002). Interleukin-8 gene regulation in intestinal epithelial cells infected with rotavirus: role of viral-induced IkB kinase activation. Virology 298, 8–19. Acknowledgements We are grateful to Jessica Pane and Izabel Di Fiore for critical reading of the manuscript. This work was supported by the National Health and Medical Research Council of Australia (project grant 1023786). http://vir.sgmjournals.org B. S. C. is a Senior Research Fellow of the National Health and Medical Research Council. Cervantes-Barragan, L., Lewis, K. L., Firner, S., Thiel, V., Hugues, S., Reith, W., Ludewig, B. & Reizis, B. (2012). Plasmacytoid dendritic cells control T-cell response to chronic viral infection. Proc Natl Acad Sci U S A 109, 3012–3017. Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 1157 G. Holloway and B. S. Coulson Coulson, B. S., Grimwood, K., Hudson, I. L., Barnes, G. L. & Bishop, R. F. (1992). Role of coproantibody in clinical protection of children Graham, K. L., O’Donnell, J. A., Tan, Y., Sanders, N., Carrington, E. M., Allison, J. & Coulson, B. S. (2007). Rotavirus infection of infant and during reinfection with rotavirus. J Clin Microbiol 30, 1678–1684. young adult nonobese diabetic mice involves extraintestinal spread and delays diabetes onset. J Virol 81, 6446–6458. De Boissieu, D., Lebon, P., Badoual, J., Bompard, Y. & Dupont, C. (1993). Rotavirus induces a-interferon release in children with Hirata, Y., Broquet, A. H., Menchén, L. & Kagnoff, M. F. (2007). de Veer, M. J., Holko, M., Frevel, M., Walker, E., Der, S., Paranjape, J. M., Silverman, R. H. & Williams, B. R. (2001). Functional Activation of innate immune defense mechanisms by signaling through RIG-I/IPS-1 in intestinal epithelial cells. J Immunol 179, 5425–5432. classification of interferon-stimulated genes identified using microarrays. J Leukoc Biol 69, 912–920. Hjelt, K., Paerregaard, A., Nielsen, O. H.,, Krasilnikoff, P. A. & Grauballe, P. C. (1987). Protective effect of preexisting rotavirus- Deal, E. M., Jaimes, M. C., Crawford, S. E., Estes, M. K. & Greenberg, H. B. (2010). Rotavirus structural proteins and dsRNA are required for the human primary plasmacytoid dendritic cell IFNa response. specific immunoglobulin A against naturally acquired rotavirus infection in children. J Med Virol 21, 39–47. gastroenteritis. J Pediatr Gastroenterol Nutr 16, 29–32. PLoS Pathog 6, e1000931. Holloway, G. & Coulson, B. S. (2006). Rotavirus activates JNK and viruses. Can J Vet Res 53, 52–55. p38 signaling pathways in intestinal cells, leading to AP-1-driven transcriptional responses and enhanced virus replication. J Virol 80, 10624–10633. Desselberger, U. & Huppertz, H. I. (2011). Immune responses to Holloway, G., Truong, T. T. & Coulson, B. S. (2009). Rotavirus Derbyshire, J. B. (1989). The interferon sensitivity of selected porcine rotavirus infection and vaccination and associated correlates of protection. J Infect Dis 203, 188–195. Donnelly, R. P. & Kotenko, S. V. (2010). Interferon-l: a new addition to an old family. J Interferon Cytokine Res 30, 555–564. Douagi, I., McInerney, G. M., Hidmark, A. S., Miriallis, V., Johansen, K., Svensson, L. & Karlsson Hedestam, G. B. (2007). Role of interferon regulatory factor 3 in type I interferon responses in rotavirus-infected dendritic cells and fibroblasts. J Virol 81, 2758– 2768. Durbin, J. E., Johnson, T. R., Durbin, R. K., Mertz, S. E., Morotti, R. A., Peebles, R. S. & Graham, B. S. (2002). The role of IFN in respiratory syncytial virus pathogenesis. J Immunol 168, 2944–2952. Feng, N., Kim, B., Fenaux, M., Nguyen, H., Vo, P., Omary, M. B. & Greenberg, H. B. (2008). Role of interferon in homologous and heterologous rotavirus infection in the intestines and extraintestinal organs of suckling mice. J Virol 82, 7578–7590. Feng, N., Sen, A., Nguyen, H., Vo, P., Hoshino, Y., Deal, E. M. & Greenberg, H. B. (2009). Variation in antagonism of the interferon response to rotavirus NSP1 results in differential infectivity in mouse embryonic fibroblasts. J Virol 83, 6987–6994. Fitzgerald-Bocarsly, P. & Feng, D. (2007). The role of type I interferon production by dendritic cells in host defense. Biochimie 89, 843–855. Franco, M. A., Tin, C., Rott, L. S., VanCott, J. L., McGhee, J. R. & Greenberg, H. B. (1997). Evidence for CD8+ T-cell immunity to murine rotavirus in the absence of perforin, fas, and gamma interferon. J Virol 71, 479–486. Franco, M. A., Angel, J. & Greenberg, H. B. (2006). Immunity and correlates of protection for rotavirus vaccines. Vaccine 24, 2718– 2731. Frias, A. H., Vijay-Kumar, M., Gentsch, J. R., Crawford, S. E., Carvalho, F. A., Estes, M. K. & Gewirtz, A. T. (2010). Intestinal epithelia activate anti-viral signaling via intracellular sensing of rotavirus structural components. Mucosal Immunol 3, 622–632. Gilliet, M., Cao, W. & Liu, Y. J. (2008). Plasmacytoid dendritic cells: sensing nucleic acids in viral infection and autoimmune diseases. Nat Rev Immunol 8, 594–606. Graff, J. W., Mitzel, D. N., Weisend, C. M., Flenniken, M. L. & Hardy, M. E. (2002). Interferon regulatory factor 3 is a cellular partner of antagonizes cellular antiviral responses by inhibiting the nuclear accumulation of STAT1, STAT2, and NF-kB. J Virol 83, 4942– 4951. Hornung, V., Ellegast, J., Kim, S., Brzózka, K., Jung, A., Kato, H., Poeck, H., Akira, S., Conzelmann, K. K. & other authors (2006). 59-Triphosphate RNA is the ligand for RIG-I. Science 314, 994– 997. Imai, M., Akatani, K., Ikegami, N. & Furuichi, Y. (1983). Capped and conserved terminal structures in human rotavirus genome doublestranded RNA segments. J Virol 47, 125–136. Istrate, C., Douagi, I., Charpilienne, A., McInerney, G. M., Hidmark, A., Johansen, K., Larsson, M., Magnusson, K. E., Poncet, D. & other authors (2007). Bone marrow dendritic cells internalize live RF-81 bovine rotavirus and rotavirus-like particles (RF 2/6-GFP-VLP and RF 8*2/6/7-VLP) but are only activated by live bovine rotavirus. Scand J Immunol 65, 494–502. Jensen, S. & Thomsen, A. R. (2012). Sensing of RNA viruses: a review of innate immune receptors involved in recognizing RNA virus invasion. J Virol 86, 2900–2910. Karupiah, G., Buller, R. M., Van Rooijen, N., Duarte, C. J. & Chen, J. (1996). Different roles for CD4+ and CD8+ T lymphocytes and macrophage subsets in the control of a generalized virus infection. J Virol 70, 8301–8309. Kasturi, S. P., Skountzou, I., Albrecht, R. A., Koutsonanos, D., Hua, T., Nakaya, H. I., Ravindran, R., Stewart, S., Alam, M. & other authors (2011). Programming the magnitude and persistence of antibody responses with innate immunity. Nature 470, 543–547. Kato, H., Takeuchi, O., Mikamo-Satoh, E., Hirai, R., Kawai, T., Matsushita, K., Hiiragi, A., Dermody, T. S., Fujita, T. & Akira, S. (2008). Length-dependent recognition of double-stranded ribonucleic acids by retinoic acid-inducible gene-I and melanoma differentiationassociated gene 5. J Exp Med 205, 1601–1610. Kim, I., Shu, C. W., Xu, W., Shiau, C. W., Grant, D., Vasile, S., Cosford, N. D. & Reed, J. C. (2009). Chemical biology investigation of cell death pathways activated by endoplasmic reticulum stress reveals cytoprotective modulators of ASK1. J Biol Chem 284, 1593–1603. Kotenko, S. V., Gallagher, G., Baurin, V. V., Lewis-Antes, A., Shen, M., Shah, N. K., Langer, J. A., Sheikh, F., Dickensheets, H. & Donnelly, R. P. (2003). IFN-lambdas mediate antiviral protection rotavirus NSP1. J Virol 76, 9545–9550. through a distinct class II cytokine receptor complex. Nat Immunol 4, 69–77. Graff, J. W., Ettayebi, K. & Hardy, M. E. (2009). Rotavirus NSP1 inhibits NFkB activation by inducing proteasome-dependent degradation of b-TrCP: a novel mechanism of IFN antagonism. Kumagai, Y., Takeuchi, O., Kato, H., Kumar, H., Matsui, K., Morii, E., Aozasa, K., Kawai, T. & Akira, S. (2007). Alveolar macrophages are the primary interferon-a producer in pulmonary infection with RNA PLoS Pathog 5, e1000280. viruses. Immunity 27, 240–252. 1158 Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Journal of General Virology 94 Innate responses to rotavirus La Bonnardiere, C., de Vaureix, C., L’Haridon, R. & Scherrer, R. (1980). Weak susceptibility of rotavirus to bovine interferon in calf Intussusception risk and health benefits of rotavirus vaccination in Mexico and Brazil. N Engl J Med 364, 2283–2292. kidney cells. Arch Virol 64, 167–170. Pichlmair, A., Schulz, O., Tan, C. P., Rehwinkel, J., Kato, H., Takeuchi, O., Akira, S., Way, M., Schiavo, G. & Reis e Sousa, C. (2009). La Bonnardière, C., Cohen, J. & Contrepois, M. (1981). Interferon activity in rotavirus infected newborn calves. Ann Rech Vet 12, 85–91. LaMonica, R., Kocer, S. S., Nazarova, J., Dowling, W., Geimonen, E., Shaw, R. D. & Mackow, E. R. (2001). VP4 differentially regulates TRAF2 signaling, disengaging JNK activation while directing NF-kB to effect rotavirus-specific cellular responses. J Biol Chem 276, 19889– 19896. Lenardo, M. J., Fan, C. M., Maniatis, T. & Baltimore, D. (1989). The involvement of NF-kB in b-interferon gene regulation reveals its role as widely inducible mediator of signal transduction. Cell 57, 287–294. Li, W., Manktelow, E., von Kirchbach, J. C., Gog, J. R., Desselberger, U. & Lever, A. M. (2010). Genomic analysis of codon, sequence and Activation of MDA5 requires higher-order RNA structures generated during virus infection. J Virol 83, 10761–10769. Pizarro, J. L., Sandino, A. M., Pizarro, J. M., Fernández, J. & Spencer, E. (1991). Characterization of rotavirus guanylyltransferase activity associated with polypeptide VP3. J Gen Virol 72, 325–332. Pott, J., Mahlakõiv, T., Mordstein, M., Duerr, C. U., Michiels, T., Stockinger, S., Staeheli, P. & Hornef, M. W. (2011). IFN-l determines the intestinal epithelial antiviral host defense. Proc Natl Acad Sci U S A 108, 7944–7949. Pott, J., Stockinger, S., Torow, N., Smoczek, A., Lindner, C., McInerney, G., Bäckhed, F., Baumann, U., Pabst, O. & other authors (2012). Age-dependent TLR3 expression of the intestinal epithelium structural conservation with selective biochemical-structure mapping reveals highly conserved and dynamic structures in rotavirus RNAs with potential cis-acting functions. Nucleic Acids Res 38, 7718–7735. contributes to rotavirus susceptibility. PLoS Pathog 8, e1002670. Liu, K., Yang, X., Wu, Y. & Li, J. (2009). Rotavirus strategies to evade interplay between induction, signalling, antiviral responses and virus countermeasures. J Gen Virol 89, 1–47. host antiviral innate immunity. Immunol Lett 127, 13–18. Randall, R. E. & Goodbourn, S. (2008). Interferons and viruses: an Lopez-Guerrero, D. V., Meza-Perez, S., Ramirez-Pliego, O., Santana-Calderon, M. A., Espino-Solis, P., Gutierrez-Xicotencatl, L., Flores-Romo, L. & Esquivel-Guadarrama, F. R. (2010). Rotavirus Richardson, V., Parashar, U. & Patel, M. (2011). Childhood diarrhea infection activates dendritic cells from Peyer’s patches in adult mice. J Virol 84, 1856–1866. Rodrı́guez, L. S., Barreto, A., Franco, M. A. & Angel, J. (2009). Lopman, B. A., Pitzer, V. E., Sarkar, R., Gladstone, B., Patel, M., Glasser, J., Gambhir, M., Atchison, C., Grenfell, B. T. & other authors (2012). Understanding reduced rotavirus vaccine efficacy in low deaths after rotavirus vaccination in Mexico. N Engl J Med 365, 772– 773. Immunomodulators released during rotavirus infection of polarized Caco-2 cells. Viral Immunol 22, 163–172. Rojas, M., Arias, C. F. & López, S. (2010). Protein kinase R is responsible for the phosphorylation of eIF2a in rotavirus infection. socio-economic settings. PLoS ONE 7, e41720. J Virol 84, 10457–10466. Marques, J. T., Devosse, T., Wang, D., Zamanian-Daryoush, M., Serbinowski, P., Hartmann, R., Fujita, T., Behlke, M. A. & Williams, B. R. (2006). A structural basis for discriminating between self and Rollo, E. E., Kumar, K. P., Reich, N. C., Cohen, J., Angel, J., Greenberg, H. B., Sheth, R., Anderson, J., Oh, B. & other authors (1999). The epithelial cell response to rotavirus infection. J Immunol nonself double-stranded RNAs in mammalian cells. Nat Biotechnol 24, 559–565. 163, 4442–4452. McKimm-Breschkin, J. L. & Holmes, I. H. (1982). Conditions Rosé, J. R., Williams, M. B., Rott, L. S., Butcher, E. C. & Greenberg, H. B. (1998). Expression of the mucosal homing receptor a4b7 required for induction of interferon by rotaviruses and for their sensitivity to its action. Infect Immun 36, 857–863. correlates with the ability of CD8+ memory T cells to clear rotavirus infection. J Virol 72, 726–730. Mesa, M. C., Rodrı́guez, L. S., Franco, M. A. & Angel, J. (2007). Saxena, V., Shivakumar, P., Sabla, G., Mourya, R., Chougnet, C. & Bezerra, J. A. (2011). Dendritic cells regulate natural killer cell Interaction of rotavirus with human peripheral blood mononuclear cells: plasmacytoid dendritic cells play a role in stimulating memory rotavirus specific T cells in vitro. Virology 366, 174–184. Mikkelsen, S. S., Jensen, S. B., Chiliveru, S., Melchjorsen, J., Julkunen, I., Gaestel, M., Arthur, J. S., Flavell, R. A., Ghosh, S. & Paludan, S. R. (2009). RIG-I-mediated activation of p38 MAPK is essential for viral induction of interferon and activation of dendritic cells: dependence on TRAF2 and TAK1. J Biol Chem 284, 10774– 10782. Mohanty, S. K., Ivantes, C. A., Mourya, R., Pacheco, C. & Bezerra, J. A. (2010). Macrophages are targeted by rotavirus in experimental biliary atresia and induce neutrophil chemotaxis by Mip2/Cxcl2. Pediatr Res 67, 345–351. activation and epithelial injury in experimental biliary atresia. Sci Transl Med 3, 102ra194. Schwers, A., Vanden Broecke, C., Maenhoudt, M., Béduin, J. M., Wérenne, J. & Pastoret, P. P. (1985). Experimental rotavirus diarrhoea in colostrum-deprived newborn calves: assay of treatment by administration of bacterially produced human interferon (Hu-IFN alpha 2). Ann Rech Vet 16, 213–218. Sen, A., Feng, N., Ettayebi, K., Hardy, M. E. & Greenberg, H. B. (2009). IRF3 inhibition by rotavirus NSP1 is host cell and virus strain dependent but independent of NSP1 proteasomal degradation. J Virol 83, 10322–10335. Narváez, C. F., Angel, J. & Franco, M. A. (2005). Interaction of Sen, A., Pruijssers, A. J., Dermody, T. S., Garcı́a-Sastre, A. & Greenberg, H. B. (2011). The early interferon response to rotavirus is rotavirus with human myeloid dendritic cells. J Virol 79, 14526– 14535. regulated by PKR and depends on MAVS/IPS-1, RIG-I, MDA-5, and IRF3. J Virol 85, 3717–3732. Pane, J. A., Webster, N. L., Graham, K. L., Holloway, G., Zufferey, C. & Coulson, B. S. (2013). Rotavirus acceleration of murine type 1 Sen, A., Rothenberg, M. E., Mukherjee, G., Feng, N., Kalisky, T., Nair, N., Johnstone, I. M., Clarke, M. F. & Greenberg, H. B. (2012). Innate diabetes is associated with a T helper 1-dependent specific serum antibody response and virus effects in regional lymph nodes. Diabetologia 56, 573–582. immune response to homologous rotavirus infection in the small intestinal villous epithelium at single-cell resolution. Proc Natl Acad Sci U S A 109, 20667–20672. Patel, M. M., López-Collada, V. R., Bulhões, M. M., De Oliveira, L. H., Bautista Márquez, A., Flannery, B., Esparza-Aguilar, M., Montenegro Renoiner, E. I., Luna-Cruz, M. E. & other authors (2011). Seo, Y. J. & Hahm, B. (2010). Type I interferon modulates the battle http://vir.sgmjournals.org of host immune system against viruses. Adv Appl Microbiol 73, 83– 101. Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 1159 G. Holloway and B. S. Coulson Seth, R. B., Sun, L., Ea, C. K. & Chen, Z. J. (2005). Identification and Trujillo-Alonso, V., Maruri-Avidal, L., Arias, C. F. & López, S. (2011). characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kB and IRF 3. Cell 122, 669–682. Sherry, B. (2009). Rotavirus and reovirus modulation of the Rotavirus infection induces the unfolded protein response of the cell and controls it through the nonstructural protein NSP3. J Virol 85, 12594–12604. interferon response. J Interferon Cytokine Res 29, 559–567. Vancott, J. L., McNeal, M. M., Choi, A. H. & Ward, R. L. (2003). The role Sheth, R., Anderson, J., Sato, T., Oh, B., Hempson, S. J., Rollo, E., Mackow, E. R. & Shaw, R. D. (1996). Rotavirus stimulates IL-8 of interferons in rotavirus infections and protection. J Interferon Cytokine Res 23, 163–170. secretion from cultured epithelial cells. Virology 221, 251–259. Vesikari, T. (2012). Rotavirus vaccination: a concise review. Clin Siegel, R., Eskdale, J. & Gallagher, G. (2011). Regulation of IFN-l1 promoter activity (IFN-l1/IL-29) in human airway epithelial cells. J Immunol 187, 5636–5644. Microbiol Infect 18 (Suppl. 5), 57–63. Weitkamp, J. H., Kallewaard, N. L., Bowen, A. L., Lafleur, B. J., Greenberg, H. B. & Crowe, J. E., Jr (2005). VH1-46 is the dominant replication: plus-sense templates for double-stranded RNA synthesis are made in viroplasms. J Virol 78, 7763–7774. immunoglobulin heavy chain gene segment in rotavirus-specific memory B cells expressing the intestinal homing receptor alpha4beta7. J Immunol 174, 3454–3460. Snodgrass, D. R., Angus, K. W. & Gray, E. W. (1977). Rotavirus Wolf, M., Vo, P. T. & Greenberg, H. B. (2011). Rhesus rotavirus entry infection in lambs: pathogenesis and pathology. Arch Virol 55, 263–274. Soloff, A. C. & Barratt-Boyes, S. M. (2010). Enemy at the gates: dendritic into a polarized epithelium is endocytosis dependent and involves sequential VP4 conformational changes. J Virol 85, 2492–2503. cells and immunity to mucosal pathogens. Cell Res 20, 872–885. Yason, C. V., Summers, B. A. & Schat, K. A. (1987). Pathogenesis of Spiegel, M. & Weber, F. (2006). Inhibition of cytokine gene rotavirus infection in various age groups of chickens and turkeys: pathology. Am J Vet Res 48, 927–938. Silvestri, L. S., Taraporewala, Z. F. & Patton, J. T. (2004). Rotavirus expression and induction of chemokine genes in non-lymphatic cells infected with SARS coronavirus. Virol J 3, 17. Stadnyk, A. W. (2002). Intestinal epithelial cells as a source of inflammatory cytokines and chemokines. Can J Gastroenterol 16, 241– 246. Youngman, K. R., Franco, M. A., Kuklin, N. A., Rott, L. S., Butcher, E. C. & Greenberg, H. B. (2002). Correlation of tissue distribution, developmental phenotype, and intestinal homing receptor expression of antigen-specific B cells during the murine anti-rotavirus immune response. J Immunol 168, 2173–2181. Tate, J. E., Burton, A. H., Boschi-Pinto, C., Steele, A. D., Duque, J., Parashar, U. D. & WHO-coordinated Global Rotavirus Surveillance Network (2012). 2008 estimate of worldwide rotavirus-associated Zhang, W., Wen, K., Azevedo, M. S., Gonzalez, A., Saif, L. J., Li, G., Yousef, A. E. & Yuan, L. (2008). Lactic acid bacterial colonization and mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis 12, 136–141. human rotavirus infection influence distribution and frequencies of monocytes/macrophages and dendritic cells in neonatal gnotobiotic pigs. Vet Immunol Immunopathol 121, 222–231. 1160 Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 12 May 2017 16:01:13 Journal of General Virology 94