* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download What is mental life
Survey
Document related concepts
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Toxicodynamics wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Theralizumab wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
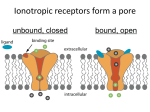
Lecture 32: Ocular Pharmacology Timothy Beer (Modified by Dave Reilly 2013) Ocular Antihypertensives (Glaucoma) **Prostaglandin Analogs: the #1 drug of choice for glaucoma o MOA Upregulate matrix metalloproteinasesincreased uveoscleral outflow Almost all the other glaucoma drugs are about “turning off the faucet” (aka decreasing aqueous production). o Clinical Use Drug of choice for glaucoma Once daily dosing o Clinical Efficacy Produces a greater reduction in intraocular pressure (IOP) than beta-blockers o Side Effects (not too bad, overall) Turns hazel eyes brown (15%), by increasing size (not number) of melanocytes Hypertrichosis (lengthening of the lashes) Eye redness (so bedtime dosing is preferred) Periorbital skin darkening Uveitis (prostaglandins are pro-inflammatory) Reversible Cystoid macular edema o Agents Xalatan **Beta-blockers: NOT the drug of choice for glaucoma o MOA Antagonize circulating catecholamines at B1 and B2 receptors at ciliary body epithelium decreased aqueous production o Clinical Use In the past, 75% of glaucoma patients used beta-blockers No longer the drug of choice Can be used adjunctively to prostaglandin analogs o Side Effects o o Carbonic Anhydrase Inhibitors Dorzolamide o o o o Decreased HR and BP Shortness of breath Fatigue Depression Decreased libido Adverse effect on lipid profiles Contraindications Asthma or other pulmonary disease Bradycardia Myasthenia gravis Agents Carteolol Non-selective beta-blocker Decreased side effects Decreased adverse effects on lipid profiles Betoptic S Cardioselective B1-blocker Less breathing problems MOA Inhibit carbonic anhydrase in pigmented and non-pigmented epithelium of ciliary body decreased aqueous humor production Note: these drugs are sulfonamide derivatives Clinical Use Used short-term emergently (orally) Drops can be used adjunctively with a B-blocker (Timolol) Side Effects Systemic effects Metallic taste Tingling Renal stones Metallic acidosis Ocular effects Burning eyes Eye redness Induced myopia (near sightedness) – ciliary body swells and pushes lens apparatus forward = lengthens distance between retina and lens = near-sighted. Contraindications Sulfa allergy – can cause serious reaction in pt w/ true sulfa allergy. Renal stones Liver or kidney disease Addison’s disease Adrenal insufficiency Thiazide diuretics Steroids Digitalis Aspirin Anticholinergics (Mydriatics/Cycloplegics) o MOA Block effect of acetylcholine Paralyze the parasympathetic iris sphincter and circular muscle of ciliary body Move the lens-iris diaphragm Stabilize the blood-aqueous barrier o o o o Alpha Adrenergic Agonists (Sympathomimetics) o o o o Clinical Use Used to for dilation (eye exam) Side Effects Atropine toxicity (Hot as a hare, red as a beet, dry as a bone, blind as a bat and mad as a hatter) Contraindications Predisposed individuals with narrow angle Can precipitate angle-closure attack Agents Atropine MOA Decrease aqueous production Side Effects Allergic reaction (redness, itching) Allergic conjunctivitis Dry mouth/nose, syncope, eyelid retraction, mydriasis Contraindications **MAOIs **Children Agents Alphagan P Iopidine Miotics (Cholinergic agents): Pilocarpine, Carbachol o o o MOA Activates the M3 cholinergic receptors on pupillary constrictor muscle - Causes dramatic miosis which stetches the iris away from the outflow tract = increased outflow. Side Effects Pilocarpine toxicity (salivation, lacrimation, sweating, N/V/D, bronchiolar spasm, pulmonary edema Worsens parkinson’s disease RARELY USED ANYMORE. Essentially only pts that have been on them forever, and in emergency/surgical setting **Anti-VEGF (Angiogenesis Inhibitors) Indications o Any ocular disease associated with neovascularization, including: Macular degeneration Diabetic retinopathy Retinal vein occlusions o GREAT DRUG!!!!!!!!! Side Effects (mostly d/t route of administration- injection) o Blurred vision o Redness of the eye o Sensitivity to light o Increased intraocular pressure o Cataract o Infection o Retinal detachment o Allergic reaction o Possible increased risk of thromboembolic events** Agents o Ranibizumab Recombinant monoclonal antibody targeting VEGF-A o Bevacizumab Antiinflammatory Agents Ocular Complications Associated with Steroids o Steroid-induced glaucoma o Cataract o Delayed wound healing, enhanced microbial or fungal proliferation, punctate keratopathy Antibiotics In contact lens wearers, use fluoroquinolone, because it covers Pseudomonas!!!!!!! The Logistics of Using Medicated Eye Drops After taking drops, close eyes and rest for a second, don’t blink o Increases contact time o Reduces systemic side effects The best time interval between eye drops is 5 minutes Major draining is through the inferior punctum – for maximum exposure you want to occlude the puctate to avoid loss of drug through the naso-lacrimal system. o Punctal occlusion = reduce systemic toxicity, avoid tasting the drops. Always occlude in pregnancy and when using -blockers! What if you think you miss getting the drop in? o Re-dose IMMEDIATELY. You cannot overdose as long as you do it right away. The cul-du-sac of the eye can only hold so much, the rest will overflow onto the cheek. The longer you wait the more time the med has to work on the eye, which means if you didn’t miss, you might overdose. PRACTICAL CLINICAL PEARLS 5 minutes between drops punctual occlusion!! Immediate redosing if necessary Chill the drops! Ask about eye meds!! Cap color is helpful Fluoroquinolones for contact lens wearers needing topical antibiotic. High Yield Receptors Muscarinic (acetylcholine) M3: pupillary constriction, ciliary body constriction (accommodation), aqueous production from ciliary body. 1 receptor: Pupil dilation receptors: increase aqueous humor production from the ciliary body, (but also increases aqueous outflow at the trabecular meshwork)