* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 59-year old male with shortness of breath
Survey
Document related concepts
Globalization and disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Infection control wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Behçet's disease wikipedia , lookup
Chagas disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Transcript
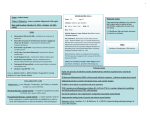
59-year old male with shortness of breath State University of New York Polytechnic Institute Presented by Francine Bassett Patient & Source of Encounter • T.I., 59-year old male • Elizabethtown Community Hospital – Emergency Department HPI • • • • 59- year old male patient presents to the ER via personal vehicle with c/o shortness of breath x 3 days. Pt reports his illness began on Monday morning. By Monday evening, pt reports he lied down and it became difficult to breath, with sudden onset. He had chest pressure that lasted approximately 30 seconds that went away after he sat up and took a deep breath. He was also clammy. Pt tried to take “cough syrup” once on Tuesday which didn’t work. He hasn’t taken any since then. Denies taking any other medications, antibiotics, or tried other interventions. Pt continues with a dry, non-productive cough, worse when laying flat and at night. Pt states he has been sleeping in the tripod position with pillows since Monday night. Today (Thursday), the school pt works at called the ER stating he was coming in. Upon arrival to the ER, pt admits to constant, non-radiating, mid-sternal chest pressure, worse when lying down, improved by sitting up. Denies pain. Admits to dyspnea, orthopnea, cough, body aches. Denies chills, fever, nausea, vomiting, abd pain, ear pain, sore throat. Denies any recent travel/limited movement. Daily cig Smoker = 10 pack years. Denies ETOH abuse or recreational drugs. Denies any known past medical history. Doesn’t recall last visit to a health care provider. Denies any medication history. Denies receiving flu and pneumonia vaccine. Denies sick contacts. ROS • • • • • • • • • General: Denies fever, chills, night sweats. Skin: Admits to sweating. Ears: Denies ear ache. Nose/sinus: Admits to clear nasal discharge. Denies post nasal discharge, sinus pain or infections. Mouth/throat: Denies sore throat. Respiratory: Admits to pain, dyspnea, orthopnea, wheezing, cough. Denies asthma, bronchitis, COPD, sputum. Cardiac: Admits to pressure, dyspnea. Denies HTN, syncope, edema Peripheral vascular: Denies blood clots. GI: Denies nausea, vomiting, abd pain. History • PMHx – Patient denies any known past medical history. – Medications:OTC Cough syrup x1 past Tuesday – unknown name. – Hospitalizations/injuries/accide nts: Denies. – Allergies: Denies allergy to food, latex, environment, or medications. – Immunizations: Denies flu and pneumonia. • Family Hx – Denies any familial hx of cardiac, blood disorders, or respiratory problems. • Social Hx – Occupational: Maintenance at grade school – Habits: 10 pack year smoker. Denies illicit drug use. Denies ETOH abuse. Physical Exam • • • • • • • • • • • • General appearance: 59-year old acutely ill male, pale, in moderate respiratory distress, sitting upright on stretcher. VS: T98.1, RR 20, P 90, BP 171/70, Spo2 92% RA (on arrival)97%2LNC Ht/Wt/BMI: 72in/160lb/21.7 Skin: Pale, warm, dry. Absence of rashes. Eyes: Sclera white, anicteric. Ear: EAC’s without drainage or edema. TM’s pearly gray, cone of light 5 o’clock Right, 7 o’clock left. Throat/mouth:. Posterior pharynx pink, without exudates. Uvula midline. Tonsils +1 bilaterally. Neck: Absence of lymphadenopathy. Trachea midline. Chest/lungs: Labored, deep, respirations. AP diameter 1:2. Coarse crackles bases bilaterally. Upper lobes with expiratory wheezes. Using accessory muscles, supraclavicular retractions. Mid-sternal pressure. Resonant to percussion. CV/PV: RRR. S1:S2. No murmurs, gallos, rubs, clicks, heaves, thrills. Absence of carotid bruits. Cap refill <2seconds. Strong 2+ radial and pedal pulses bilaterally. Absence of peripheral edema. Abdomen: Flat. Absence of hepatosplenomegaly. Neurological: Alert and oriented to self, place and time. Speech intact. Differential Diagnosis (so far) • • • • • • • DVT Pulmonary Embolism MI CHF Pneumonia Bronchitis COPD/asthma exacerbation Diagnostics/Work-up • • • • • • • CXR EKG CBC CMP D-Dimer Troponin BNP Treatment • Saline lock • 2LNC Oxygen • Duoneb (Albuterol/Ipratropium) INH x1 – Short acting bronchodilator/short acting anticholinergic Post-treatment • Oxygen: Spo2 92%97% 2LNC95% RA at discharge • After Duoneb Wheezes improved upper lobea. Coarse crackles absent. Clear bases bilaterally. • VS: BP 148/76, HR 87, Spo2 99% 2LNC, rr 18 Diagnostics - Results CXR No infiltrates or consolidation. Nml. EKG Sinus rhythm CBC WNL CMP WNL D-Dimer 50 (<=250) Troponin <0.02 BNP 586 (<200) Diagnosis – Rule out • • • • • • • DVT Pulmonary Embolism MI CHF Pneumonia Bronchitis COPD/asthma exacerbation Diagnosis • Obstructive chronic bronchitis with Exacerbation ICD-9 491.21 Etiology • Prolonged exposure to bronchial irritants – Smoking, environmental, occupational – Chronic, poorly controlled respiratory allergies – Chronic respiratory infections – Low birth weight (Hollier & Hensley, 2011, p. 576)(Global Initiative for Chronic Obstructive Lung Disease, 2015,p. 6) Incidence • 14.2 million people – COPD • 12.5 million people – Chronic bronchitis • Fourth leading cause of death in United States (Hollier & Hensley, 2011, p. 576) Pathophysiology •Inflammatory disease of the mucus membranes of the bronchi •Increased amount of sputum throughout part or the entire year. •Chronic irritation leads to increase in mucus production •Mucus gland hyperplasia and increased risk for infection •Airway narrowing and increased airway resistance, fibrosis around bronchioles •All these factors result in airway narrowing = obstructive disease (Higginson, 2010, p.107-108) Management Plan • Ventolin MDI (Albuterol sulfate) 90mcg 2 puffs INH Q4-6H PRN – Short acting bronchodilator • Prednisone taper (corticosteroid) • Z-pak Zithromax (Azithromycin) 250mg PO daily x6days – Macrolide Abx Education • Minimize exposure to irritants • Pneumococcal & influenza vaccine • Reduce exposure to persons with respiratory infection • Increase fluid intake • Pursed lip breathing (if needed) • Smoking cessation Follow-up • Every 3-6 months for stable disease • Maintain close follow-up with patients with acute respiratory infections • Review treatment plan with patient at each visit (Hollier & Hensely, 2011,p. 576) References • Global Initiative for Chronic Obstructive Lung Disease. (2015). Pocket guide to COPD diagnosis, management, and prevention. Retrieved February 18, 2015 from http://www.goldcopd.org/uploads/users/files/GOLD_P ocket_2015.pdf • Higginson, R. (2010). COPD: pathophysiology and treatment. Nurse Prescribing, 8(3), 102-110. • Hollier, A., & Hensley,R. (2011). Clinical guidelines in primary care: A reference and review book. Lafayette,LA: Advanced Practice Education Associates.