* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dental Caries
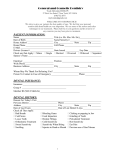
Survey
Document related concepts
Public health genomics wikipedia , lookup
Health equity wikipedia , lookup
Patient safety wikipedia , lookup
Dental amalgam controversy wikipedia , lookup
Dental implant wikipedia , lookup
Race and health wikipedia , lookup
Maternal health wikipedia , lookup
Forensic dentistry wikipedia , lookup
Tooth whitening wikipedia , lookup
Water fluoridation in the United States wikipedia , lookup
Scaling and root planing wikipedia , lookup
Dental avulsion wikipedia , lookup
Focal infection theory wikipedia , lookup
Dental degree wikipedia , lookup
Transcript
L1 Community Community dentistry is an applying field, it is concerned with identifying and attempting to resolve problems related to dentistry at the community level .The community is a dynamic environment priorities are continually changing. Social, cultural, economic and biological variables interact in an infinite variety of patterns There are many methods for approaching Some are more effective than others, regardless the methods used. They are most all satisfy/two/ criteria.. • • 1/Recognition . that the community is dynamic complex environment With numerous interacting factors. • • 2.Development or Systemic approach, on. problem identification and resolution 1. Definition to know what is the problem? . how it is identified ? • What are the characters of the problem ? what are the terms and the Processes used to describe problem ? and why it is a problem . • • • 2.Distribution or epidemiology .in relation to age, sex, region were the Problem is present. What is the distribution of the problem in the Specified population and the epidemiology. And how it frequently is Observed . • • 3.Causality. what factors were responsible for the problem • Beginning and what factors were responsible for the continuation Of the problem, which variables are involved? And how do they Interrelate? • • • • • 4.Resolution, what methods or techniques have been or could be used to resolve the problem. 5.Outcome. what were the outcomes of various methods used • • And what are the potential outcomes of the most method to Resolve problems? what have been or may be the outcome of failure to intervene • Dental public health. By /ADA/ it is defined as the science and art of • preventing and controlling dental diseases and promoting dental health through organized community efforts . It is the form of dental practice which regards the community as a patient rather than the individuals. • It is concerned with administration of group of dental care programs .as well as the prevention and control of dental diseases on a community bases . Note. Distribution e.g. dental caries as a problem .Age. it prevails • mostly in children and continue . but to less extent in adults of third decade of age . where as periodontal diseases prevail in patient who have been passed the fourth decade of age, with less occurrence of dental caries. • Sex. Males and females are equally effected by dental caries . also caries prevalence vary in different regions. • L2 Dental public health &the private practitioner: that dentistry exits to serve the public. The private practitioner deals with individual patient, but the other people who can not go to the clinic must also receive a dental health care & this is done by dental public health programs & the need for the public health program is achieved by periodic survey of a cross section of public from time to time. Because of misunderstanding between private & public sectors in health care the basic similarities between them should be clear. A-Examination / Survey: when patient first come to dental office, we do examination, chief complain, medical history, extra oral & intra oral examination, but in the community, we'll call it "Survey" instead of examination, the survey deal with chief complain of population like lack of access to dental care for elderly people, or the survey may be an epidemiology assessment of oral diseases, problem of a chosen group. So, in dental public health, the word survey: usually means clinical assessment, extent & survey of disease in population. B- Diagnosis/ Analysis: Private clinic following examination, next step is diagnosis, in dental public health we do analysis of survey data by statical methods to process & analyze the survey data. C- Treatment planning / program planning: Treatment planning in private clinic is complex because of many factors must be balanced, patient interest, cost, patient agreement on type of treatment. So, thepatient is an cative part in treatment decision. Also in program planning for community, the health professional when do planning, the planning must be accepted bu community. Government may reject it or carry out part of it or adept a less costly alternative program, & decision depends on community health problem in comparison to other community problems that are in need of attention. D- Treatment / program: Clinics do specific schedule for carrying out the indicated treatment or referring patient to a specialist for certain procedures. For community puplic health program, we do puplic health team I,e. for elderly people in nursing home, programs are involving super vision of the home, nurses, workers, private dental practitioners, dental hygienist & others. E- Payment/ program funding: The government may pay the program & in health professional must know the how to secure & then to manage. F- Evaluation/ program appraisal: Dentist evaluation of progress begins during course of treatment & is repeated at each visit, observation made during the initial examination, such as extent of plaque, calculus deposits & then evaluation is made from time to time. Similarly data collected initial survey series as the basic line against which program appraisal can be made to assist the effectiveness of public health program. The differences: In addition to similarities between private & public health practice, there are some differences. Major differences are that in goals of public health. Are socially determined, but the private only coincidentally related to social goals. Public health seeks to minimize the chances that the worst possible outcome will occur. The privates work alone, will public health work as team, so government not ones owns decision. Public health reach to people can not go to private clinic because it is expensive to reach & also it reaches to handicapped & isolated community. The administration of dental health programs include health promotion, community prevention & provision of dental care to specify groups [handicapped poor & elderly]. Dental public health practice almost always. Involves a team effort with other professional such as physicians, nurses, social workers & nutritionists. The dental public health practice gets away from office, its program require cooperation efforts which cover the hole city. Country or even hole community. So serv larg group of people rather than single pat. Personal & community health care: The severalties Community A. Examination Survey B. Diagnosis Analysis C. Treatment planning Program planning D. Treatment Program operation E. Payment Program funding F. Evaluation Program appraisal L3 Epidemiology of dental caries Caries in ancient man Limited knowledge were available. The only way is the examination of The ancient skull. Hunting and gathering was the Principle source of food. In Britain caries prevalence (500 AD-1500AD) little change Diet was coarse cause dental attrition • Cervical or root caries were mostly observed. Caries were uncommon in primary teeth • • Occlusal caries were diminished because of attrition Occlusal and proximal caries were appear In Western country in 1600 A.D due to the • • • • Changes in dietary habit (due to increase in refine diet ) and more intake of sugar. In 1900 A.D. (nineteenth century) in Britain and most Western countries. Dental caries is a disease of civilization. High prevalence of dental caries in • Developed country (Western Europe, • North America, Australia, New Zealand and Japan. • • • • • Low prevalence of dental caries in • Developing Country (Central Africa and less economic developing country). • • Dental caries was related with refine carbohydrate . • Developing countries dental caries start to be increased. For example Iraq .7 • • 3. 5 9 years Greenland 1.5 10.4 Vietnam 2.0 6.3 • 20 years 11 years • • In U.S.A. There is decline in DMF • Which is due to water fluoridation ,school Water fluoridation and using of fluoridated Dentifrices. • Dental Caries by age ,sex and race • 25.8% of children aged 1-5 have caries. Dental caries begin early in life. • • Hagerstown studies by Klien and Palmer • • • (pioneer study) susceptibility of teeth to Dental caries 1937. L76-67 L7-7 • L6-6 U76-67 U54-45---L5-5 • • • U21-12 U3-3 L4-4 L321-123 • • Caries experience as measured by DMF index continue to increase steadily with • Age and sharply in youth and early adult and more slowly in the later years of life. Age related problem is root caries due to gingival recession • Female generally appear to develop Higher DMF scores than do male • • • Female state better oral hygiene than • Male and female visit dentist frequently • • African and Indian show much freedom Of dental caries than European and • Show more immunity and may be due to environment than of internal racial Attribute. • • • • Black and White in U.S.A show differences in DMF scores Blacks show less DMF even when groups were standardize for income and education. Genetic factor of minor influence on D.C Diet :oral intake of substance Nutrition: Absorption of nutrient • • D.C. is lowest in low living standards of live. • • • • • D.C. is a disease of civilization. • Urban area show high D.C. than rural area. • • Little effect of deficiency of micronutrient And vitamins on D.C. except fluoride • • Low cariogenicity of diet was attributed • Not to the presence of hard and fibrous food But to the absence of fermentable Carbohydrates in the diet • • • Vipeholm study in Sweden 1945-1952 • In mental institution (un ethical study) • groups • They gave them 0-24 sticky toffees /day Sugar intakes Conclusion; • • • 1-sugar consumption increase-caries increase 2-D.C. increase (C.A.) in sticky form 3- Risk increase when sugar taken between • Meals in sticky form. 4-Great individual variation. 5-Increase in carries disappearance upon Withdrawal of sticky food stuffs. 6-Caries can still occur in the absence Of refine sugar. • • Hopewood House institution in Australian State of New south Wales (15y study) on • Children Vegetarian diet (restrict in sucrose )(81 child) age 4-9(78%) caries free • • 13 53% caries free compared to 4% of same age non institutionalized Carioginic potential of food stuffs and dietary patterns still need further research. • • L4 EPIDEMIOLOGY of Dental Caries Definition of Dental Caries The word Health Organization ( 1988 ) define dental caries as : "a bacterial disease of the dental hard tissue , it begins with acid demineralization of the outer enamel surface and , if not arrested or treated ,the dissolution of enamel continues into the dentin and pulp increasing cavitation and loss of tooth substance " Dental Caries is an infectious, microbiological disease that result in localized dissolution and distraction of the calcified tissues of the teeth . Dental Caries is a multifactorial disease requiring the presence of a susceptible host, cariogenic microflora and a diet conductive to enamel demineralization (Miller 1890) Dental Caries In daily practice , the lay person and dental personnel usually talk about dental caries as the cavity in the tooth .However the carious cavity represents a sign or a symptom of the disease and is ,as such ,a rather late reflection of the disease itself . The disease dental caries is a dynamic process taking place in the microbial deposits which results in a disturbance of the equilibrium between tooth substance and the surrounding plaque fluid so that , over time ,the net result is a loss of mineral from the tooth surface . The word Caries is derived from Latin , meaning "rot " or decay ,it is similar to the Greek word Ker meaning death . It is a disease that dates back to antiquity and occurs in populations that have never used sugar or processed food. There is presently an alarming rate of increase in the prevalence of dental caries in developing countries. The introduction of sucrose into the modern diet has been associated with the increased caries prevalence Currently Accepted Theories of the Etiology of Dental Caries There are three general theories regarding the mechanism of dental caries . The proteolysis theory received attention with the identification of protein in human enamel . Gottlieb and Frisbie are among the proponents of this theory .Even though there are those who do not subscribe to the theory , they may admit that proteolysis possibly plays a role in the dental caries process . The proteolytic – chelation theory has recently received considerable attention .The proponents of the theory look upon the enamel as a simple organic structure that is associated with large amounts of inorganic matter to satisfy mechanically its functional requirements Those who advance this theory consider caries to be like any other infections disease and as an attack on an organic body structure ( enamel ). They further believe that all infections disturb the mineral balance locally and systematically and that caries disrupts the inorganic substance when the organic components are attacked . It has now been rather conclusively shown that a number of microorganisms can produce acid of sufficient potential to decalcify tooth structure , particularly lactobacilli , aciduric streptococci ,diphtheroids ,yeasts , staphylococci and certain strains of Sarcina . Epidemiology Dental Caries may be consider a disease of modern civilization, since prehistoric man rarely suffered from this form of tooth destruction. Anthropologic studies revaled that dolicocephalic skull of men from pre Neolithic periods (12.000 BC) did not exhibit caries, but skull from Brachycephalic man of the Neolithic periods ( 12.000 to 3000 BC ) contained carious teeth . The cervical areas of teeth in older persons were frequently affected . Caries in Prehistoric Man (3000 to 750 BC) There is no evidence of dental caries in the relatively few teeth found in the skull fragments of our earliest known ancestors. Evidence of fairly extensive decay was found in at least one skull of a Rhodesion man from the Neanderthal age. Evidence of caries was found in about one half of the 24 skulls of the prehistoric race which lived central Europe about 15.000 years ago .(cited in Essentials of Preventive and Community Dentistry 2004 ) Caries Susceptibility of Individual Teeth Brekhus (1931) studied a group of students at the University of Minnesota and reported the following caries susceptibility incidence of the teeth . Upper and Lower First Molars = 95% Upper and Lower Second Molars = 75 % Upper Second Bicuspids = 45 % Upper First Bicuspids = 35% Lower Second Bicuspids = 35% Upper Central and Lateral Incisors = 30% Upper Cuspids and Lower First Bicuspids = 10% Lower Central and Lateral Incisors. = 3% Lower Cuspids = 3% KLEN and PALMER (1941) studied the problem of individual tooth susceptibility, pointing out that the teeth farthest back in the mouth are more frequently carious. Caries Experience in Schools Children A valuable indication of the effectiveness of any preventive measure in controlling dental caries is the extent to which the first onset of caries is delayed . The high levels of attack soon after eruption , reported by Miller ( 1953 ) ,Jackson ( 1965 ) , Hargreaves and Chester ( 1973 ) and Todd ( 1975 ). The first permanent molars are a problem in children since they may become extensively carious at an early age . The situation is aggravated by the fact that many parents do not recognize first molars as part of the permanent dentition ( Gray et al , 1970 ) . Todd (1975) found that 40% of mothers believed that the first permanent molar did not erupt until 10 years of age or later , 45% of the molars of the 12 – year-old children who had lost one or more permanent molars through that the children had suffered only the extraction of the deciduous teeth This is an unfortunate misconception since , although only half of the parents thought it worthwhile to fill a deciduous molar , 90% preferred filling to extraction of a permanent tooth .However , treatment may not be sought until the first molars have deteriorated badly . Caries of the occlusal surfaces is the most likely form of attack in the • immediate post – eruptive years . Surveys in low fluoride areas have shown that occlusal caries may affect half of all first permanent molars after 1 year in the mouth ( Miller , 1953 ; Jackson , 1965 ) , 80% are carious within 2 years ( Hargreaves and Chester , 1973 ; Lewis and Hargreaves , 1975 ) and 90% carious by the age of10 (Berman and Slack1972) , In studies of 8 – year – old Swedish children , Mansson ( 1977 )and Holur (1978 ) found 42% and 65 % of first molars affected by caries ; respectively . • Virtually all first molars lost have been affected by occlusal caries • (Picton, 1 965; Miller, 1972) .Other sites on the tooth are affected more gradually. Miller (1972) reported that a proximal cavities were found within 1 year of eruption and that they were still appearing 8 years later. Durks ( 1966 )also states that caries start in many molars very early and caries progression is fast .However ,Knuison and Klein ( 1938 ) found that only 30 % of permanent first molar teeth are carious in 8 year old children , Mansson ( 1977 ) records 42% of these teeth as carious at this age , compared with 65 % observed by Holm ( 1978 ) There are ,therefore ,considerable discrepancies in the data from these investigation . • If a preventive regimen rather than merely a reparative regimen is to established then consideration must be taken of preventive techniques and the need to emphasize oral hygiene measures .The American Dental Association Council on Dental Materials (1976) states that fissure sealants from an acceptable part of proven effective preventive measures, but treated surfaces should be examined at least every 6 months. . Evaluation of dental health education also show that oral hygiene instruction must be reinforced regularly in order to be effective ( Mcallan et al 1976).Therefore , restorative programmes and preventive regimens for children must be based on frequent recall examinations of not more than 6 –monthly intervals . The worldwide prevalence of dental caries and periodontal disease is well recognized. The incidence and prevalence of each may vary from one community to another, and all age groups may be affected, but dental caries tends to be more prevalent in the young while periodontal disease more commonly affects the adult population. Though both are chronic destructive disease, dental caries destroy the hard tissues of the teeth, whereas periodontal disease destroy the supporting structures and tissues. Both disease may cause pain, infection, disfigurement, interference with function, and emotional problems. In the light of present knowledge, the prevention of both these disease requires education in three main areas: 1. Adoption and continuing regular application of prescribed oral hygiene and nutritional practices Periodic dental care .2 1-The early treatment of disease 2-the application of specific preventive measure for dental caries prevention A- topical application of fluorides teeth to prevent periodontal disease. B-professional cleaning of the 3. Application of community wide measure such as fluoridation of water supplies. For example, socio-cultural, situational, and economic factors may interfere with nutritional intake and with the frequency and correctness of tooth treatment services may be blocked by a number of social, economic, psychological, and environmental factors. are of crucial significance to the Since dental caries and periodontal disease should be given of dental health throughout the world, they improvement .education programmes top priority in dental health It is possible that teeth and periodontium can serve as a reservoir for respiratory infection , oral bacteria can be released from the dental plaque into the salivary secretions which are then aspirated into the lower respiratory tracts to cause pneumonia and that sever anerobic lung infections can occur following aspiration of salivary secretions, especially in patients with periodontal disease and (30-40%) of all cases of aspiration pneumonia , necrotizing pneumonia or lung abscess involve anerobic bacteria (Brook, 1993; Levison, 1994). The Mortality of Permanent Teeth The mortality of teeth is usually expressed as the mean number of • extracted teeth per person. When all teeth have erupted this is proportional to the percentage number of erupted teeth which have been extracted, although this presumes that all missing teeth were at one time present .Whichever way it is expressed , mortality figures are a crude but useful measure of the dental status within a community . From the data obtained in the epidemiological studies reported by Jackson ( 1961 ) it was possible to calculate the percentage number of extracted permanent teeth in children and adults . Data were calculated for 12- year – old children and for age groups 15 to 19 years, 20 to 24 years, and for each succeeding group of five years up to 60 to 64 years When the mortality of teeth is plotted against age ,there appears to be three phases of loss ,namely up to the mean age of years ,between the mean ages of 22 and 47 years and from the mean age of 47 years onwards .It is note that the second phase of loss is largely coincident with a relatively quiescent period in caries attack ,and that the third phase is associated with a slight increase in the rate of caries attack (Jackson 1961 ). In view of the fact that the first and second permanent molars have similar susceptibilities to caries attack at least on occlusal surfaces, but there is a difference in the mortality curves of these teeth The main value of mortality figures lies in their ability to give a broad indication of the dental status of a community , in which dental treatment is provided . They depend , in the main ,on disease incidence , demand for treatment and the success of conservative treatment in its broadest sense . L5 Primary Health Care: In 20th century, there is ↑ in amount of treatment provided by dental professional in most part of the world. → Improvement in methods of cutting teeth. → Improvement in giving analgesia. → Improvement in dental material. → Improvement in dental personal. → ↑ in dental caries and periodontal disease. Prevalent of dental caries: Most effective method in reduce dental caries is 1- Water fluoridation: which is adjustment of conc. of fluoride of water supply to 1 ppm which recommended by WHO ↑ the resistant of enamel to dental caries. Fluoride incorporate with enamel to form hydroxyfluoroapatite crystals. Naturally fluoridated water supply if fluoride more than 1 ppm → enamel hypoplasia or mottled enamel → Defluoridation Advantages of water fluoridation: Easiest way to ↓ prevalence of dental caries. 1- Costless. 2- Saving the working time. 3- Saving the human suffering (toothache). 4- Saving physical and mental trauma. 5- Reduction 50-60 % in dental caries, when children drink fluoridated water during the total period of tooth calcification. 6- Both dentition are affected. 7- Benefits last throughout the life mainly effect on smooth surfaces of the teeth rather than pits and fissures, occlusal (least benefit) 2- School water fluoridation: Several studies show benefits specially in areas lack of public water supply fluoridation. In Iraq 0.03 Others 0.8- 1ppm Disadvantages: summer holiday students spend 5 days/ a week, students spend 6 hr./ a day . 3- Fluoridated salt: Salt as a vehicle for supplying fluoride in Switzerland and Hungarian. Conc. 200-300 mg/kg salt. 4- Fluoridated tablets: Daily administrated 0.25-1 mg fluoride depend on age of child Regime is difficult (every day). 5- Professional topical fluoride: Topical fluoride application by professional -- 2% NaF → stable -- Sn2F 2%, 4%, 8% and 10% → non AAstable -- Acidulated phosphate fluoride (APF) 1.23% is best Advantage of fluoridated gel : -- Adhere to the teeth -- Can apply it by tray -- Fluoridated mouth rinse: -- Supervised → in school, low cost 6- Toothpaste fluoride prophylactic pastes: -- Reduction 25 – 42% -- Used since 1942 -- NaF, Sn2F or APF -- In more than 75% of toothpaste a significant agent. 7- Fissure sealant: -- To prevent dental plaque accumulation in pit and fissure → dental caries -- Effective -- Costly -- Time taking procedure 8- Dental health education -- For parents specially pregnant women -- For children in kindergarten, primary school, secondary school. - In primary health clinic center. L6 Public Dental Care Programs: Programs for: 1- Handicapped. 2- School children. 3- Elderly people. 4- Mobile clinics General health care is important for all people, good oral hygiene is a vital aspect of health care, the private practice is notable to meet the dental demands of all people, so, a number of public dental health programs have, therefore, developed that aims to meet the needs of specific groups because even within communities that are well served by dentists, there are groups who are not regionally treated in private clinics, these groups are: This term for dentistry can be referring to patients whose oral health may be considered within normal range, but who have physical and/or mental or emotional condition which may prevent them from being treated routinely in dental situations, so, they can be classified into: mental, physical, medical and sensory handicapped. Also known as people with learning disability. They suffer from dental caries and periodontal diseases like the rest of population leading to tooth loss. Daily oral care to decrease plaque and dietary control of sugar should be a matter of routine, however, this group has poorer oral hygiene, there are barriers to dental care exist in this 1- Oral health may have a low priority in the family. 2- Dental care may be restricted by attitudes and access. 3- Treatments maybe difficult to provide because of fear and anxiety, lack of understanding & inability to cooperate. 4- Involuntary movements may restrict oral care of dental treatments. 5- Difficulty with communication complicate the situation. These groups have poor oral plaque control and more periodontal diseases. This is reported in studies of people learning disability in comparing with normal people and they have more teeth extracted example: for these groups are Down syndrome and cerebral palsy. B- Physical Disability: This condition may affect manual dexterity and arm control and mobility which may influence oral health and those include arthritis, osteogenesis imperfecta and rickets. C- Medical Handicapped: Children or persons with medical handicapped fall into two groups: were to develop dental 1- Those whose general health affected if they diseases. 2- Those whose need for dental care in itself, are at risk, example: persons with cardiovascular diseases and leukemia. D- Sensory Handicapped: are blind and deaf people. In communities each state or regions should have health center for handicapped persons, training programs for handicapped should be established by health center, dental school health departments and they select dentist or dentists to attend that health center for all handicapped groups programs ranging from oral hygiene programs. to preventive programs , involving application of fluoride topically, fluoride tablets for patients attending special school and organized brushing programs, also a systematic pattern of a preventive oral care should be established at birth to decrease the risk of caries and periodontal diseases and the need for active dental treatment, the dental treatment may also be involved in the construction of mouth health application which assist physical disability, also use chemical plaque contra. 2- School Children: Schools Dental Health Programs: Each school should have a dentist appointed as consultant or local health center and periodic dental examinations should be encouraged by school through programs of education for parents and children. The program should be based on preventive and long term of oral hygiene practice rather than an actual dental treatment in the school. Schools should be encouraged to eliminate sail of candies and sweeting beverage in a school dental society should be instrumented in the helping and establishing of school food and beverage. Schools Dental Health Programs: Programs that contributes to nutrition needs of child, water fluoridation of school water supply and fluoride tablets is applied, also tooth brushing. pro grams and dental inspection and referral programs, topical fluoride treatment within this school fluoride rinse program, also the school dental health programs should include teaching dental health in the classroom by the dentists or dental hygienist and this is has been shown to be available to assist motivating children to improve their dental health practice through periodic planned lectures or talk to school group. The criteria over preventive programs by fluoride application should be: 1- Therapeutic procedures, be effective and safe. 2- The program, be capable of reaching large number of children. 3- The procedure, be economical and relatively simple for require minimal use of professional manpower. 4- Program represents little interference as possible in the school curriculum. 5- The procedure provides benefits without any further action on the part of patients. 6- It must be accepted by the child. These programs may include: fluoridated mouth rinse applied weekly in school classroom or tooth brushing with a fluoridated tooth paste for 4 -6 min. under supervision. 3- Elderly people: Who may be suffering from illness or disability maintaining a healthy mouth may play a significant part in the process of rehabilitation and recovery. -The mouth and its associated structures play an important physiological role in mastication and nutrition, so, the systemic benefits of nourishing and well balanced diet contributes to general health and signs of mouth in both speech and appearance is neglected aspect in older people. The oral effects of aging; there are changes in oral tissues & surrounding structures which are associated with aging process, the degree of changes depending on a variety of individual factors which are genetic influence, experience of diseases, lifestyle, nutrition and habits. -Teeth: the structures of teeth undergo a number of changes like attrition, abrasion or erosion, gingival rescission and root caries, bone resorption. Barriers to dental care: 1- Mobility: increasing mobility problems with age restrict access to services, public transport maybe difficult to be used or inaccessible or unavailable. 2- Economic resistance: high-cost of dental treatment is the most common reason for not seeing the dentist. 3- Fear and anxiety: previous experience of dental treatment have a negative effect. 4- Believes: they believe that teeth lost with age, so. the health program for, this group if by dental team visiting homes and institutes of elderly people, diet control and mouth rehabilitation and fluoridated 4-Mobile Clinics: Mobile dental & portable equipment can be, effectively, utilized to provide services to scattered groups of people in rural area, public institutes & school, home bounded, disabled persons. The cost of operation & transportation & time is greater with mobile units comparing with fixed facilities. The mobile clinic is evaluated on patients needs & demand. The home visit & mobile clinic by dental authors is done by dental team consist of in addition to dentists, dental hygienist dental assistants, dental health educators & dental technicians. 4-Mobile Clinics: Mobile dental & portable equipment can be, effectively, utilized to provide services to scattered groups of people in rural area, public institutes & school, home bounded, disabled persons. The cost of operation & transportation & time is greater with mobile units comparing with fixed facilities. The mobile clinic is evaluated on patients needs & demand. The home visit & mobile clinic by dental authors is done by dental team consist of in addition to dentists, dental hygienist dental assistants, dental health educators & dental technicians. The major principles are: 1- No harm. 2- Do good (beneficence). 3- Autonomy. 4- Justice. 5- Truthfulness. 6- Confidentiality. No Harm (Non maleficent) To do no harm is generally attributed to Hippocrates & is considered to be the foundation of social morality. It is clear that although dental care professionals support this principle in theory they are at times guilty of transgressions. Iatrogenic disease is the name which give to doctor induce illness, & all of us in dental field have seen: Overhanging restorations → periodontal disease. Failure to sterilize instruments → infection. To do good (beneficence): a concept also traced to Hippocrates. It should be the rule of dentists to benefit patients as well as not to cause harm. The expectation of the patient is that the dentist will initiate beneficial action & that some thins good will occur. Example: refilling the tooth without need Means that dentist respect the patents right to make decisions concerning the treatment plan. Patient should not be by slanders in their .treatment but active participants. Informed consent both legal & ethical concept is an essential component of the patient's right to autonomy. This consent requires that the. following four elements to be present: 1- Disclosure of appropriate information including risks & benefits involved in the treatment, consequences of non treatment, & alternative treatments when applicable. 2- Ccmiprenension of the information by the patient. 3- Voluntary consent. 4- Competence to consent. Dentist some times attempt to direct the patient toward a particular mode of treatment by stressing certain advantages & mentioning the disadvantages. The dentist may believe that is in the best interest of the patient to have the treatment, but it is not ethical to mislead or misinform patients. The dentist must not with holding information, restricting choices, or making the choice for the patient. The example for that is the fluoridation of community water supply to protect people who might not have fluoride Tab or drops. This is in the public's interest, but in other side limits the rights of segment of the public because we judge that it is in their best interest. Justice: Is often described as fairness or equal treatment giving to each her or his right. In providing dental care it is difficult to distribute services to all who are in need, but it should be the concern of health care professionals to see that as even a distribution as possible occurs. Dentists can provide some free or discounted care in their offices to those who are truly needy, or they can work some times clinics of low-income patients. Some dentists complain that they can not treat low income patients because of fees too low, or can't treat mentally retarded because it takes too long time. So a question arise who will treat the poor in that only dental professional can provide dental care? So dentists, in serving the public, may exercise discretion in selection patients for their practices, dentists shall not refuse to accept patients in their practice or deny dental service to patient because of the patient's race, color, sex, or international origin A dentist has the general obligation to provide care to those in need. A decision not to provide treatment to an individual because the individual has AIDS or hepatitis B is unethical decision with regard to the type of dental treatment provided or referrals made or suggested in such instances should be made on the basis as they are made with other patients. Consultation with patient physicians must done to know if the health status of the patient is compromised by the dental treatment or not. Truthfulness: Is an ethical principle, that one would expect to go unquestioned, yet many truthful way, as example the dentist may feel that it will be better if the patient took a certain course of action & therefore manipulate the information that is given to the patient, whatever the reason, the relationship will ultimately suffer & the dentist will be guilty of transgressing a major ethical principle. Confidentiality: The patient has the right to expect that all communications & records pertaining to their care- will be treated as confidential. Examples: 1- When the students talk between them about their cases in the presence of other patients. 2- When the dentist make the previous patient as an example to the next patient. Dentists maintain patients records in a manner consists with the protection of the welfare of the patient. Upon request of a patient or another dental practitioner, dentist shall provide any information that will be beneficial for the future treatment of the patient Codes of Ethics: Fundamental requirements for the status of profession is a formal code of ethics. These codes provide a pattern of behavior- for how professional should behave toward other professional. Professional codes of ethics save as a useful purpose in that they assemble in a single document many of cultural norms of profession as well as promote some of the universally held principle of ethics. The professions must be careful continue to remember that a professional is one who places the interests of the patient above his or her own. Professions exist only at the pleasure of the society, if professions fail to promote the good of society they will cease to exist because society can regulate & this limit the autonomy of professions at will. Code 1: Service to the public & quality of care: the dentist primary professional obligation shall be service to public. A- Not refuse any patient because of patient's race color, sex or national origin. B- Protection of confidentiality of patient's records. C- Use their skill knowledge & experience to serve the community. D- Emergency service: do emergency service for his own patient & when consulted in an emergency case & if treatment is provided the dentist is obliged to return the patient to his or her regular dentist. E- Dentist obliged to seek consultation if possible whenever the welfare of patient will be needed, F- Dentist obliged to report instances of gross or continual faulty treatment by other dentists. G- Dentist shall not represent the care being rendered to their patient in a false or misleading manner. Code 2: Education: all dentists have the obligation of keeping their knowledge & skill current. Code 3: Research & development: all dentists have the obligation of making the results & benefits of their investigation available to all when they are useful in promotion of health of the public. Code 4: Professional Announcement: dentists should not misrepresent themselves in a manner that would be false or misleading. Forensic Dentistry Forensic Odontology: is the branch of odontology which deals with the proper handling & examination of dental evidence & with proper evaluation & presentation of denial findings in the interest of justice. Interest in Forensic Odontology was introduced in the later part of 19 century. The first form instructional program was giving at the armed process institute of pathology in USA, since then the number of cases recorded are increased, the rule of Forensic Odontology in the last few decays. Keiser - Nielsen define three major fields of activity within Forensic Odontology, namely: 1- Examination & evaluation of injuries to teeth, jaws & oral tissues from various causes. 2- The examination of bite marks with a view to subsequent elimination or possible identification of a suspect as the originator. 3- The examination of dental remains (whether fragmentary or complete. & including all types of dental restoration) from unknown persons or bodies with a view to the "possible identification of the latter. The scope (purpose) of Forensic Odontology include the use of dental findings in identification procedures. Because of their high degree of mineralization, teeth are the most durable of human tissue & may be preserved. when much of the body has been destroyed by fire, chemicals or decomposition. Consequently the useful method of identification when other means have failed lies in the comparison of dentitions of human remains with ante- mortem dental records, the dentist & physician (pathologist) work together as a team & combine to observe, document & record ail the findings & ensure the retention of all specimens necessary to solutions of the case. Records dental features in the necessary degree of detail. Documentation may range from the simplest comments concerning the presence of plaque, calculus & overall condition to a full dental charting with taking of impression. Dental findings or identification: Dental identification- is based on the comparison of ante-mortem records with the completely charted records of post mortem remains. The following information is recorded: 1- Shape of teeth & number present. 2- Relationship of tooth to tooth in the arch. 3- Type of occlusion. 4- Presence of diastema. 5- Shape & number of roots. 6- Sites of fluorosis. 7- Sites of sub-surface decalcification of enamel. 8- Special peculiarities of jaw anatomy. 9- Shape & position of restorations & dentures & materials from which they are fabricated. 10- Carious lesions. 11- Unerupted & impacted teeth. 12- Retained root fragments. 13- Root fillings. 14- Congenital missing teeth, premolars removed for orthodontic treatment. Radiographs; may be used to locate mental foramen location. Cephalometric X-ray for all teeth & presence of restorations. Bite wing X-ray of post-mortem is compared to the ante-mortem records. Photographs; ante-mortem photographs will often demonstrate the teeth & facial structure with sufficient clarity & to help in dental identification & this is compared to postmortem examinations (diastema & crowding). Study casts; plaster casts is useful for comparison. Lip prints: is found on drinking glass or napkin, but it is not valid. Palate rugae; suggested as a means of personal identification. Estimation of age The most accurate method for age determination in the skull is the dentition analysis. Tooth development & eruption patterns are positive criteria for age determination from the pre-natal Period to maturity. Using standardized developmental charts. the broad range of dental age can be assayed from a bout 5 months. In uteri studies using vital staining & histological techniques show that the initial calcification of 1st primary, molars occurs. As early as 13 – 63week in uteri. Determination of age can be done by radiographic evidence of crown & root formation (resorption) & eruption times is considered. Sexual dimorphism for eruption time in the permanent dentition is well established. Girls tend to exhibit advanced development compared with boys, at all stages of permanent teeth development this includes teeth calcification and all stages of eruption. Sex differences are maximal in the mandibular dentition. A wide range of variation in eruption timing is present among different populations &/or countries. Eruptions seems to occur earlier in southern (warmer)in northern (cold) ones. Variations also exist in the calcification rates in warmer versus colder-climate Blood group determination The ABO system is the most important of the blood groups system used in medico-legal cases. Typing blood performed with fresh blood. In dried blood stains only A.B& H substances are preserved & these identified by modifications of standard techniques. Identification of blood substances secretions & tissues found at the scene of a crimes .more complex than it is with blood from blood samples & may be particularly valuable in the absence of blood. In saliva & soft tissues the ABH blood groups are presents & the saliva collected from the site of crime & blood group can be determined. Also blood group can be obtained from bone & teeth this, is done by using teeth powder. personal identification through dental evidence - teeth fragments to DNA: in cases when no ante-mortem information is available DNA technology that employ dental evidence to assist in resolving violent crime. The DNA analysis can be obtain from dental pulp & teeth fragment. The role of Forensic dentist in Mass Disasters Modern man exposed to many natural & accidental disasters & in recent years mass murders. Because of the very nature of mass disaster implies the presence of destructive force, the most durable structure of the human body are the teeth, so they may remain. The teeth when exposed to exposed to 400F may become brittle &. brake down to as hat 900 F, but they can be protected from such high heat by the insulation of soft tissue and bone, dental restorations an likely to withstand high temp. The collection of fragments of bone & teeth are collected together. The jaws are isolated & radiographed, charting of the findings is done then comparison between post-mortem / findinExamples: Moronic Disaster: 1949 ship-fire 118 people die. The bodies badly burned disfigured, so, they need dental identification. 59 cases were solved stock Port Disaster: aircraft crush 1967. 72 were killed. Some-fire destroy their limbs & bodies. Dental identifications was aid in determination age, charting the dental findings to compare with ante-mortem records gs & ante-mortem information. Professional responsibility final practice): When dentist undertake to treat a patient the law requires that certain disclosures to be made regarding the proposed the treatment. If dentist fails to inform the patient the patient may be entitled to recover damages for injuries done during treatment because he was not informed enough. Even if you do root canal treatment for a tooth instead of extraction & this procedure is very successful, no guarantee can be given, occasionally, a tooth, after root canal treatment may require terminal surgery or extraction. Negligence in diagnosis & failure to refer & this may lead patient to die Example (Cancer & extraction of teeth). A patient attended to a. dentist with painful tooth. The dentist suggested extraction of it. The patient returned with no socket healing. Then the dentist prescript a drug. After few days the patient returned -with.-no healing then the dentist sent, a specimens a histopathologist, the histopathologist asked for a biopsy, then the biopsy demonstrated a malignancy. & that was too late to be treated, so, the patient died, & the dentist mulcted complication of extraction: fracture of mandible in extraction, records of the patient must be kept for long period of time, so that the dentist can defend himself against any problems. Bite marks: It has been well documented that owing the factors such as size, shaggy wear, rotations, diastema, accidental fracture of teeth, not to sets of human teeth are exactly a like. If a good impression is taking; it could prove that teeth marks are unique. There are 4 factors that give the bite mark. Its characteristics are: 1- The teeth of the biter. 2- The action of the tongue, lip & cheeks of the biter at the time the bite was inflected. 3- The mental state of the biter at the time the bite was inflected 4- The portion of the body upon which the bite was inflected. Also size & shape of teeth is considered if the bite was done by a human being or animal. The serological evidence associated with the bite mark could be use because saliva left on the bite mark. The bite mark is legally accepted & admissible in a court of law. It is accented as a powerful tool in the investigative of the crime. Human bite marks are found mostly in cases of murder child abuse. Several methods are used to record characteristics - of size, shape & position of the teeth to generate -overlays computer based radiograph, xerographic hand trace method. The area of edges of anterior teeth & relative rotation of each anterior tooth measured and compared General appearance: 1- Dental condition, occlusion, restoration & open cavities. 2- Age 3rd molar = 18 years old person. 3- Sex & race. 4- Occupation: may be gained from teeth, example: loss of enamel in battery workers, lead poisoning in some workers. 5- Habits example: pipe smokers, abrasion of anterior centrals. 6- Socioeconomic Status: mouth care & type of restoration. 7- Country of origin, type of cavity preparation & bridge construction ( differ from different dental schools).