* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download TOXIDROMES
Survey
Document related concepts
Pharmacogenomics wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Drug interaction wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Transcript
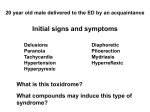
Toxidromes and Drug Ingestions Toxidromes What is a Toxidrome? A constellation of clinical signs that may suggest a particular type of ingestion Toxidromes may indicate what type of drugs a patient has taken if they are unable or unwilling to tell you Toxidromes The most common toxidromes seen are: Anticholingeric Cholinergic Sympathomimetic Sedative Hallucinogenic Serotonergic Anticholinergic Toxidromes Anticholinergic Toxidrome Due to drugs that block muscarinic and nicotine acetylcholine receptor Antihistamines (1st generation) Tricyclic antidepressants Antitussives (cough mixtures) Antipsychotics Anticonvulsants Antimuscularinic drugs Atropine Scopolamine Ipatroprium bromide Plants Mushrooms Datura Anticholinergic Toxidrome The anticholinergic toxidrome consists of: Delirium + peripheral antimuscarinic effects Mad as a hatter Red as a beet Mydriasis Hot as a hare Flushed skin Blind as a bat Confusion/hallucinations/seizure/coma Hyperthermia Dry as a bone Dry skin, urinary retention, ileus Cholinergic Toxidromes Cholinergic Toxidrome Due to drugs that activate acetylcholine receptor ie the opposite of anticholinegric toxidromes Cholinergic Toxidrome Caused by: Organophosphate insecticides Carbamate insecticides Chemical warfare agents eg Ricin, Tabun, Soman, VX Alzheimer's medication eg donepezil Agents used for myasthenia gravis Neostigmin Edrophonium Pilocarpine Phyostigmine Cholinergic Toxidrome The cholinergic toxidrome =“DUMBELS”: D U M B Miosis (or mydriasis) Emesis Lacrimation Salivation urination Bronchospasm Bronchorrhoea Bradycardia Diaphoresis Diarrhoea (and abdo cramps) E L S Sympathomimetic Toxidromes Sympathomimetic Toxidrome Act via stimulation of sympathetic nervous system Toxidrome – everything stimulated Hypertension Tachycardia Tachypnoea Hyperthermia Agitation Dilated pupils (usually) Diaphoresis/flushing c.f: anticholinergic – dry Sympathomimetic Toxidrome In New Zealand the most commonly seen sympathomimetic ingestion is methamphetamine Can also be seen with Alpha receptor agonists Beta receptor agonist Phenylephrine eg OTC cold preparations eg - coldrex Salbutamol Theophylline Caffeine Alpha and beta agonists Amphetamine Cocaine Pseudo/ephedrine MDMA (ecstasy) Sedative or Hypnotic Toxidromes Sedative or Hypnotic Toxidrome Caused by any medication that causes CNS depression, such as: Benzodiazepines Barbiturates Alcohols Opioids Anticonvulsants Antipsychotics Sedative or Hypnotic Toxidrome Toxidrome Decreased Level of consciousness Hypoventilation Hypotension Bradycardia Opioids + barbiturates also cause Miosis Hypothermia Hallucinogenic Toxidromes Hallucinogenic Toxidrome As it sounds, this is caused by drugs and agents that cause hallucinations Amphetamine Cannaboids Cocaine LSD PCP Magic mushrooms (Psilocybin spp.) Hallucinogenic Toxidrome Primarily presents with hallucination Also can present with: Frank psychosis Panic attacks and anxiety Sympathomimetic symptoms esp. tachycardia, hypertension and fever Serotonergic Toxidromes Serotonergic Toxidrome A collection of signs and symptoms produced by excess serotonin in the central, peripheral and autonomic nervous systems Serotonergic Toxidrome Multiple medications can cause serotonergic toxidrome (or serotonin syndrome) Most commonly occurs when ≥ 2 medications which affect either serotonin reuptake or metabolism are given, but can also occur with a single agent Serotonergic Toxidrome Associated with: Selective serotonin reuptake inhibitors (SSRI -antidepressants) Serotonin noradrenalin reuptake inhibitors (SNRI –antidressants) Eg metoclopramide, ondansteron Anticonvulsants Eg pethidine, tramadol, fentanyl Antiemetics Eg moclobmide Analgesic Eg venlafaxine, citaloprma Tricyclic antidepressants Monoamine oxidase iunhibitors (Block serotonin break down –used as antidepressants) Eg paroxtetine, fluoxetine Eg valproaic acid Dietary supplements Eg St johns wort, ginseng Serotonergic Toxidrome Produces wide variety of signs and symptoms due to CNS, peripheral and autonomic dysfunction Most commonly produces Tremor Hyperreflexia and muscle rigidity esp in the legs Clonus Fever Tachycardia and hypertension