* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Basics Pharmacology Review
Survey
Document related concepts
Orphan drug wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Pharmacognosy wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Theralizumab wikipedia , lookup
Transcript
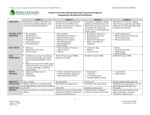
Back to Basics Practical Pharmacology Dr. Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Assistant Professor, Dept of Family Medicine, University of Ottawa Clinical Pharmacist, Bruyere Academic Family Health Team March 2013 [email protected] (Partially adapted from slides by Marc Riachi, R.Ph.) Objectives • Review all pharmacology in an abnormally short amount of time in preparation for LMCC • List the four steps of rational prescribing • Understand the pharmacological classes, generic examples and mechanisms of action of important tools in the practice of medicine. • Understand how the kinetics and dynamics of these agents can affect their use • Highlight clinical pearls in the proper use of these agents in practice. Topics to be covered • • • • • • • • • • • • • • • Antibacterials Antimycobacterials Antifungals Narcotic analgesics Autonomic nervous system Anti seizure drugs Migraines Antidepressants Antianxiety agents Agents for insomnia Antidiabetics Antilipemics Antihypertensives Diuretics Nitrates Ref: Marc Riachi, RPh • • • • • • • • • • • • • • Antiplatelets and anticoagulants Antiasthmatics BPH Erectile dysfunction Dementia Parkinson’s disease and schizophrenia Dyspepsia, GERD and PUD Antiemetics IBD IBS Osteoporosis Gout OTC drugs Appendix I & II Topics to be covered in this lecture • • • • • • • • • • • • • • • Antibacterials Antimycobacterials Antifungals Narcotic analgesics Autonomic nervous system Anti seizure drugs Migraines Antidepressants Antianxiety agents Agents for insomnia Antidiabetics Antilipemics Antihypertensives Diuretics Nitrates • • • • • • • • • • • • • • Antiplatelets and anticoagulants Antiasthmatics BPH Erectile dysfunction Dementia Parkinson’s disease and schizophrenia Dyspepsia, GERD and PUD Antiemetics IBD IBS Osteoporosis Gout OTC drugs Appendix I & II A Process for Rational Prescribing (your new best friend) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • To promote an efficient process for selecting optimal drug therapy for patients • To promote a process for applying population level evidence based medicine to individual patients. A Structure Requires Process To prescribe or not to prescribe? That is the question… • Rational prescribing requires a process for selecting therapy: (in order) 1. 2. 3. 4. Efficacy Toxicity Cost Convenience 1. Efficacy – Ask About… 1. Which HARD Outcomes a) Mortality benefit? b) Morbidity benefit? 2. Which SURROGATE Outcomes • Clinically relevant? 3. THEN “What is the quality of the evidence to prove this?” • • • • Meta-analysis? Randomized Controlled Trial? Case series? Anecdotal evidence? Efficacy • If there is no efficacy, why waste your time on the potential toxicity, cost and inconvenience of a drug? • If there is proven efficacy at the population level, then balance this against the potential toxicity to the individual. 2. Toxicity – Ask About… Bothersome Severe Common Rare Not legal Who cares • Age? • • Newer agents Older agents = = Less Safety Data More Safety Data 3. Cost – Ask About… • Patient cost vs Societal cost • Covered under provincial formulary? – Covered under private plans? 4. Convenience – Ask About… • What is the likelihood of compliance? 1. Frequency of administration? – Daily vs QID? 2. Special restrictions? (eg. bisphosphonates) – PO vs IV? – Home vs Office vs Hospital therapy? 3. Many interactions? 4. Special monitoring requirements? A simple example: Metformin Januvia® VS Why is Metformin first line therapy? Efficacy 1. HARD Outcomes – Mortality benefit » Metformin – reduction in CV events (UKPDS-34 trial) – Morbidity benefit » Metformin – reduction in microvascular complications 2. SURROGATE Outcomes a) Hgb-A1c reduction a) Metformin ~ 1% - 2% b) Januvia® ~ 0.5% - 0.8% b) Insulin Sparing Effects a) Metformin Toxicity • Metformin – Very rare risk of lactic acidosis? • 0.03 cases / 1000 pt-yrs (~ 50% fatal) • Never clearly implicated – GI upset / diarrhea • Start low, go slow! – B12 / folate deficiency / anemia (6 - 8/100) • Reduced absorption – easy to supplement – Anorexia • usually transient • Januvia® – ?Unknown - too new • ?Pancreatitis – Too few patients examined – GI upset – edema – ?elevated risk of infection? Cost & Convenience • Metformin • Januvia® – Ontario Drug Benefit: – Ontario Drug Benefit: • $ 0.0587 / tab • Covered by ODB • $ 2.8050 / tab • Covered by ODB – Rxfiles 2012: • ~ $33 / 100 days – QD to TID po – Rxfiles 2012: • ~ $315 / 100 days – Once daily po Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Antibiotic Review (80% of the knowledge, 80% of the time) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • Review clinically relevant pathogens in human disease in an ambulatory care setting • Review antibiotic classes and spectra of activity – Focus on bread and butter examples of each • Review treatment recommendations for common infections in primary care Process 1. Map the Bugs – “Know your enemy” 2. Map the Drugs – “Save your ammo” 3. Map the Battlefield Part 1 - Map the (Clinically Important) Bugs “Know your enemy” Gram Negative Aerobic β-Lactamase Negative Cocci (spheres) Bacilli (rods) Gram Positive Anaerobic β-Lactamase Positive Map the Bugs Aerobes Anaerobes Gram Positive Gram Negative Gram Positive Gram Negative Cocci Bacilli Cocci Bacilli Cocci Bacilli Cocci Bacilli b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] b-L[+] b-L[-] 5 6 7 8 b-L[+] b-L[-] b-L[+] b-L[-] b-L[+] b-L[-] b-L[+] b-L[-] 9 10 11 12 13 14 15 16 Anaerobes Above & below the diaphragm Oral • Simple organisms • Easily handled by penicillins (beta-lactams) – Eg. Actinomyces Bifidobacterium Fusobacterium Lactobacillus Peptococcus Peptostreptococcus Propionibacterium etc Gut • Approx the same, except: • Human pathogens: • Bacteroides fragilis (B.frag) • Clostridium difficile (C.diff) – More virulent bugs requiring ‘bigger guns’… Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Above & Below diaphragm Bacilli B.Frag C.Diff b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] 5 6 b-L[+] b-L[-] 7 8 9 . Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Below diaphragm Bacilli B.Frag C.Diff b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] 5 6 b-L[+] b-L[-] 7 8 9 . Gram[+] Bacilli • Not usually pathogenic – Major Exception: Listeria monocytogenes • Listeriosis – enteritis, sepsis, meningitis +/- encephalitis Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Below diaphragm Bacilli B.Frag C.Diff (Listeria) β-L[+] β-L[-] 1 2 b-L[+] b-L[-] 3 4 β-L[+] β-L[-] 5 6 7 . Gm[-] Cocci • Not usually pathogenic – Major Exceptions: • Neisseria gonorrhea • Neisseria meningitidis and • Moraxella catarrhalis – (formerly thought to be a type of Neisseria) Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci (Neisseria & Moraxella) β-L[+] β-L[-] 1 2 Bacilli (Listeria) Below diaphragm Bacilli B.Frag C.Diff β-L[+] 3 β-L[-] 4 5 . β-Lactamase Enzymes • First penicillinase described in 1940’s even before penicillin was clinically available. • Most bugs produce some type of β-lactamase enzyme that destroys β-lactam antibiotics (pen’s, ceph’s, carbapenems) – Gm[+] cocci & β-lactamase [-]: only Group A strep give Penicillin Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci (Neisseria & Moraxella) Bacilli (Listeria) β-L[+] β-L[-] 1 (GrpAStrep) Below diaphragm Bacilli B.Frag C.Diff β-L[+] 2 β-L[-] 3 4 . Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Below diaphragm Bacilli B.Frag C.Diff β-L[+] 1 both β-L[+]&[-] 2 3 . Map the Clinically Important Bugs Atypicals Aerobes Gram [+] Gram [-] Cocci Bacilli 1 2 1. Legionella pneumonia 2. Chlamydia pneumonia 3. Mycoplasma pneumonia 3 . Anaerobes (esp. Gut organisms) Eg. C-Diff & B-frag 4 . 1 - Gram [+] Cocci Staphylococcus • S. aureus – Methicillin resistant (MRSA) – Methicillin sensitive (MSSA) • S. epidermidis – Methicillin resistant (MRSE) – Methicillin sensitive (MSSE) – Skin commensal – Rarely pathogenic Streptococcus • Group A (pyogenes) (β-Lact[-]) • Group B (agalactiae) • Neonates, v. elderly, obstetrics • S. pneumonia etc. etc. Enterococcus • (Formerly thought to be ‘Strep D’) • E. faecalis • E. faecium 2 - Gram [-] Bacilli • • • • • • Easy to Kill Proteus mirabilis Escherichia coli Klebsiella pneumonia Salmonella Shigella Haemophilus influenza • • • • • Hard to Kill Serratia Pseudomonas Acinetobacter Citrobacter Enterobacter – (Moraxella catarrhalis) (actually a Gm[-] coccus) PEcKSS-HiM SPACE bugs Gram Negative vs Gram Positive Gm[-]: red on stain. (ie. Don’t retain stain) Gm[+]: blue-purple on stain; Gm[-]: must pass through pores Gm[+]: molecules < 100kDa pass easily. Gm[-]: b-lactamases concentrated in periplasmic space Gm[+]: b-lactamases diffuse outside cell; Atypicals: • Mycoplasma pneumo • Chlamydia pneumo • Legionella pneumo Map the Bugs • Gram positive aerobes: – Cocci Summary Anaerobes: • Oral • Gut – Bfrag & Cdiff • Gram negative aerobes: – Bacilli • Staph – Aureus » MRSA (~8-10%) » MSSA – Epiderimidis » MRSE (~65%) » MSSE • Easy to Kill – PEcKSS (Proteus, Ecoli, Klebsiella, Salmonella, Shigella) – HiM (H.flu and Moraxella (actually a Gm[-]coccus)) • Hard to Kill – SPACE bugs (Serratia, Pseudomonas, Acinetobacter, Citrobacter, Enterobacter) • Strep – – – – Group A strep (pyogenes) Group B strep (agalactiae) Strep Viridans Strep pneumo etc. • Enterococcus – Faecalis – Faecium – Bacilli • Listeria – Cocci • Neisseria – gonorrhaea – meningitidis • Moraxella catarhallis Part 2 - Map the Drugs (Save your Ammo) Map the Drugs • Arms race! – Remember: “Bigger guns breed higher walls” • Older drugs tend to be simpler drugs – More narrow spectrum – Broad spectrum drugs breed resistance – Superbugs develop • MRSA, VRE, ESBL, etc • Older drugs have more safety data – Tend to be less toxic – Learn their history – Learn their pharmacology Part 2 - Map the Drugs “Save your Ammo” Fluoroquinolones Penicillins Tetracyclines Aminoglycosides Vancomycin Macrolides Carbapenems Cephalosporins Clindamycin Metronidazole Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Beta-Lactams - Penicillins Penicillin Anti-Staph Anti-Strep Amoxicillin / Ampicillin (po) (iv) Amox + Clavulanic acid Cloxacillin / Methicillin (clinic) (lab) Beta-Lactams - Cephalosporins – Cephalexin (Keflex™)(or Cefadroxil) (po) – Cefazolin (Ancef™) (iv) • 2nd Generation – Cefuroxime (po & iv) • 3rd Generation – Ceftriaxone, Cefotaxime, Ceftazidime (iv) – Cefixime (Suprax™) (po) • 4th Generation – Cefepime (iv) Increasing Gram[-] coverage • 1st Generation Beta-Lactams – Other (FYI) (IV only, inpatient use only) • Piperacillin (plus tazobactam) – big gun, tazo = suicide substrate, like clavulanic acid • Carbapenems – Meropenem – Imipenem – Ertapenem • Monobactams – Aztreonam Broad spectrum, big gun antibiotics that cover Gm[+], both easy and hard to kill Gm[-] bugs, even some anaerobes. Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Fluoroquinolones • 2nd generation – Ofloxacin – Ciprofloxacin – Norfloxacin • 3rd generation – Levofloxacin • 4th generation – Moxifloxacin • Covers: strep & Gm[-]’s – PEcKSS-HiM & SPACE bugs • Ofloxacin • Ciprofloxacin – Anti-pseudomonal – the only PO option! – Norfloxacin • Same spectrum as Cipro (even anti-Pseudomonal) – but only for cystitis UTI. • Concentrates in the G.U. system only • N.B. Not good enough for pyelonephritis or systemic infection Fluoroquinolones • The “Respiratory FQs” – Concentrate in alveolar macrophages – Greater than serum concn 1. Levofloxacin – the more active Lenantiomer of Ofloxacin – Renal clearance 2. Moxifloxacin – Hepatic clearance • Enhanced coverage of: 1. Strep pneumo 2. Oral Anaerobes 3. Atypicals – N.B. only Moxi cover B.frag – Neither covers C.diff • (Both will cover Clostrium non-difficile strains) • Both have 100% oral bioavailability – Therefore PO = IV dose Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Macrolides • Coverage of: – Atypicals, Strep pneumo, & Hi.M. (Hflu & Mcat) • So, good for respiratory infections! – N.B. But doesn’t cover PEcKSS or SPACE bugs • Erythromycin – Efficacy: Poorer coverage of H.flu, MSSA – Toxicity: • Prokinetic – diarrhea! • Worse for QTc prolongation – Convenience: QID dosing • Clarithromycin – Better Hflu &MSSA coverage – Less QTc prolongation vs E – Shorter half-life vs Azithro • BID dosing x 7-10days • New daily ‘XL’ formulation • Azithromycin – An azalide, (not a macrolide) • Same spectrum of activity • Less QTc prolongation vs E & C! – Long t1/2 – QD dosing x 5d • BUT can breed resistant S.pneumo (since below [MIC] for long periods of time) Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Aminoglycosides 1. Gentamicin 2. Tobramycin – Reserved for Pseudomonas aeruginosa 3. Amikacin • Efficacy: excellent Gm[-] • Toxicity: – Nephrotoxicity – Ototoxicity – Less now with daily dosing • Cost: • All excellent Gram[-] coverage: – PEcKSS-HiM and SPACE bugs – Cheap, old meds • Convenience – Now Once daily IV/IM Pharmacodynamics Relationship between Abx Concentration & Effect Concentration Dependent Killing • Higher the peak, better the kill • i.e. Ratio of peak drug concentration and M.I.C. determines rate of kill. • Eg. FQs, AGs Log [Conc] Time Dependent Killing • Time over MIC matters • i.e. Independent of peak concentration. Determined by length of time over MIC • Eg. B-lactams (Pen, Ceph etc) Log [Conc] Peak MIC MIC Time (h) Time (h) Pharmacodynamics Relationship between Abx Concentration & Effect Concentration Dependent Killing • With renal impairment: – Maintain the peak, lengthen the interval – This ensures good rate of killing while allowing enough time to eliminate the drug and avoid toxicities – For eg: • Higher the peak, better the kill • i.e. Ratio of peak drug concentration and M.I.C. determines rate of kill. • Eg. FQs, AGs Log [Conc] Peak Log [Conc] Peak MIC Time (h) MIC Time (h) • If CrCL = 90mL/min Levofloxacin 750mg q24h po • If CrCL = 30mL/min – Levofloxacin 750mg q48h po Pharmacodymamics Bactericidal vs Bacteriostatic • Bactericidal Abx – – – – – – B-lactams (Pen, Ceph) Aminoglycosides (AGs) Fluoroquinolones (FQs) Rifampin Metronidazole Vancomycin • Bacteriostatic Abx – – – – Tetracyclines Macrolides Clindamycin Chloramphenicol Rarely a clinically important characteristic, unless the patient is immunocompromised or the risk of death with delayed/incorrect therapy is high. Combination Therapy • Why? – Broaden spectrum • (eg. Mixed infection) – Synergistic activity for hard to kill bugs • (eg. Enterococcus or pseudomonas) – Prevent resistance • (eg. TB) – Reduce dose and side effects Map the Drugs Pharmacology Summary • Many antibiotic classes – Beta-lactams generally safest agents. • Even at high doses – Some have overlapping mechanisms of action – Avoid combining similar mechanisms of action • Competing effects may reduce effectiveness of one agent • Eg. Penicillins + vancomycin – cell wall synthesis inhibitors • Eg. Tetracyclines + aminoglycosides –protein synthesis inhibitors via 30-S subunit of the ribosome Map the Drugs – Summary For: TB, MRSA For: skin, dental infx (staph, strep, & anaerobes) From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Part 3 – Map the Battlefield Map the Battlefield Rational Prescribing Individual Population 1. Efficacy 1. Efficacy – Could be reduced, BUT: – Empiric tx still effective if it is well chosen – Maintained long term with lower resistance rates 2. Toxicity • (Lower risk infections, properly dosed, clinically stable, true indication etc.) – Reduced since lifespan of older drugs is maintained 3. Cost 2. Toxicity – Reduced with narrow spectrum tx 3. Cost – Reduced with older tx 4. Convenience – Usually less convenient VS. – Reduced insurance costs, economic losses, hospital costs dealing with superbugs 4. Convenience Map the Battlefield Map the Battlefield Otitis media: S.pneumo, Hi,M Conjunctivitis: viral – no tx (Amox +/- Clav, Cef2, Septra) Sinusitis: viral – no tx AECOPD: S.pneumo, Hi,M Oral anaerobes: abscess drainage – no tx (Amox +/- Clav, Cef2, Septra) (Amox 2g – pre dental sx?) C.A.P: S.pneumo, atypicals – (Amox, Macrolides (Clarithro/Azithro)) CAP+comorb./risk factors, or NHAP: also HiM bugs (Combine AmoxClav or Cef2 + Macrolide (or use FQ)) Cellulitis: MSSA, S.pneumo – (Clox, Cef1, Clinda) Pyelonephritis: PEcK – (Septra, Amox/Clav, FQ (not Norflox) UTI (Cystitis): PEcK – (Septra, Macrobid, Amox, Norflox) Pharyngitis: viral – no tx (Group A Strep – Pen VK) Bronchitis: viral – no tx Skin abscess: drainage – no tx H.pylori: triple po tx PPI + (Clarithro +/Amox +/- Metro) Cdiff / Bfrag: Metro / po Traveller’s Diarrhea: (80% bacterial): EcSS, Vanco (camphlyobacter) - Septra, FQ, (Azithro) Map the Battlefield Penicillin (Group A Strep, oral anaerobes, Neisseria) Amoxicillin / Ampicillin (Strep & Enterococcus plus Easy-to-Kill Gm[-](ie. PEcKSS)) Cloxacillin (Staph aureus, Staph epi) Amox/Clav (Vancomycin) (for Strep & Entero & PEcKSS-HiM) (H.flu & Moraxella can be ~35% amox resistant) (for MRSA / MRSE) (~8-10% / ~ 65% resistant) Beta-Lactams - Cephalosporins – Cephalexin (Keflex™) or Cefadroxil (po) – Cefazolin (Ancef™) (iv) • 2nd Generation – Cefuroxime (po & iv) • 3rd Generation To boost: for PEcKSS-HiM (same as Amox/Clav) SPACE bugs: The Big Guns – Ceftriaxone, Cefotaxime, Ceftazidime (iv) – Cefixime (Suprax™) (po) • 4th Generation – Cefipime (iv) Increasing Gram[-] coverage • 1st Generation MSSA and Strep & PEcKSS (same as Amox) N.B. never Enterococcus! SPACE bugs • The Big Guns: – 3rd and 4th generation Cephalosporins – Carbapenems (Meropenem) – Piperacillin/Tazobactam – Aminoglycosides (Gentamicin, Tobramicin) – Fluoroquinolones (Levofloxacin, Moxi, Cipro) Reserved for Pseudomonas • Ciprofloxacin (FQ) – The only PO agent! – (Use Norfloxacin for UTI if a FQ is needed) • • • • • Ceftazidime (Cef3) Cefipime (Cef4) Tobramycin (AG) Piperacillin/Tazobactam Meropenem Need for Bigger guns • There is a higher risk of Gram negative SPACE bugs with: – More risk factors / comorbidities – COPD, HIV, Diabetes, CKD etc – More institutionalized settings • Community Retirement Home Nursing Home Hospital ward ICU ventilated pt in ICU. Map the Battlefield • PEN – for Group A Strep, oral anaerobes, Neisseria • ?What to do for Strep/Entero? – Amox po / Amp iv (also good for PEcKSS) – How to boost? Amox/clav (for HiM-PEcKSS) • ?What to do for Staph? – Clox (MSSA, MSSE); Else Vanco (MRSA, MRSE) • What about Cef1? (cephalexin / cefadroxil po or cefazolin iv) – Maps to Amox/Amp for PEcKSS and strep • N.B. NOT Enterococcus (Cef’s never cover enterococcus!) – How to boost? Cef2 (cefuroxime) for HiM-PEcKSS • What about SPACE bugs? – FQs, AGs, Cef3, Cef4, Pip/Tazo, Meropenem) – Reserved for Ps aureginosa:(cipro, tobra, ceftazidime, cefipime, pip/tazo, meropenem) • What about gut anaerobes? (Metro/PO Vanco) • What about atypicals? (Macrolides, Tetracyclines (doxy)) • Where does Septra fit? (with Amox/Clav and Cef2) Antibiotics contraindicated in pregnancy (category X) • • • • • • • • • Tetracyclines (also in children < 9 y.o.): are incorporated into fetal skeleton/unerupted teeth Fluoroquinolones Erythromycin estolate (may cause toxic liver reaction), clarithromycin TMP: in 1st trimester because it is a folate antagonist Sulfonamides: last trimester or if delivery is imminent because they interfere with the bile conjugating mechanism of the neonate and may displace bilirubin bound to albumin which may lead to jaundice and kernicterus Nitrofurantoin (during labor and delivery only): can affect glutathione reductase activity and hence can cause hemolytic anemia (analogous to the problems it causes in patients with glucose-6-phosphate dehydrogenase deficiency) and hemolytic crises have been documented in newborns and fetuses Aminoglycosides: nephrotoxic and ototoxic to the fetus High (>2 grams) single dose metronidazole Chloramphenicol (at term or during labour): limited glucuronidating capacity of the newborn’s liver Ref: Marc Riachi, RPh Antibiotics Preferred in Pregnancy • Penicillins • • • • • • Including those in combination with ß-lactamase inhibitors (clavulanic acid, sulbactam, and tazobactam) Cephalosporins Erythromycin base Azithromycin Clindamycin Metronidazole • Ref: Marc Riachi, RPh (regular dose 250-500 mg BID) Summary • This is far from an exhaustive review • Some parts have been highly simplified for use in clinical practice • Some memorization is needed with regular review of the material to retain this knowledge • Doing so will allow you to choose empiric antibiotics with greater comfort in difficult situations and unfamiliar settings. Penicillin: BL-ve aer obic GPC oral anaer obes N.meni ngitidi s Lacking Activity Vs. Atypical Organis m s BL+ Ae robic GPC Ae robic GNB Gut anaerobe s (B. fragilis) 95% of Staph. specie s are BL +ve MRSA(7%)/ MRSE (>65%) MSSA/MSSE TMP/SM X Clindam ycin Easy to Kill GNB Macrolide s : Erythromycin Clarithromycin Azithromycin TMP/SM X Tetracyclines Res pirator y Fluor oquinolone s Gatif loxacin Levofloxacin Moxif loxacin Vancom ycin Rifam pin Fus idic Acid Line zolid Syner cid Me tronidazole Am picillin/Am oxicillin: HiPEELSS Isoxazoyl PCNs : e g. Cloxacillin, Nafcillin 1st Ge ne ration Cephs : (Cefazolin iv / Ce phalexin po) PEcKSS Second Gener ation Ce phs Am oxicillin/Clavulanic acid Am picillin/Sulbactam Ce furoxim e Ce furoxim e axetil Ce faclor B. fragi li s H. i nfluenza e Ce fote tan Ce foxitin Difficult to Kill GNB 3rd Gener ation Ce phs. Ce ftriaxone Ce fotaxim e Ce ftazidim e 4th Ge ne ration Cephs : Ce fe pim e No Ce phalos porin cover s: MRSA / MRSE enterococcus sp. Listeri a monocytogenes AM Gs: Ge ntam icin Tobram ycin Am ik acin Pipe racillin: (P.aerugi nosa , Enter obacter) Never Us e Alone ! Pipe racillin/Tazobactam Ticarcillin/Clavulanic Acid FQs : ciprofloxacin ofloxacin norf loxacin Carbape ne m s : Im ipenem Me rope ne m Adapted fr om : Wins lade N. On Continuing Practice 1990-1, volum es 17-18. Prepare d By: Sandr a A.N. Tailor, Pharm .D. Clinical Coor dinator - Infectious Dise as e s Sunnybrook Health Science Ce ntre Depar tm e nt of Pharm acy 11/11/02 Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD TB drugs Adapted from: Marc Riachi, RPh Mycobaterium tuberculosis The Consumption • Mostly latent, asymptomatic infection (90-95%) – – – – Activation risk ~ 10% Usually pulmonary; can occur anywhere Spreads via air droplet One third of world population infected! • Europe:, TB rates rose from 1600s to peak in the 1800s (caused ~25% of all deaths) • Organism has "waxy" hard to penetrate cell wall – Acid-fast bacilli – Combinations of drugs needed to treat • Slow growing – Therefore requires extended treatment period • Treatment: – Multiple side effects = reduced compliance by patient = further emergence of resistant strains – MDR, XDR strains Adapted from: Marc Riachi, RPh Available antimycobacterials • First-line: – Isoniazid (INH) – Rifampin (RIF) or Rifampicin (RMP) – Pyrazinamide (PZA) – Ethambutol (ETB) • Second-line: – Amikacin – FQs (Ciprofloxacin / Levofloxacin / Moxifloxacin) – Clarithromycin / Azithromycin Ref: Marc Riachi, RPh Treatment - Active Pulmonary TB • “4 drugs x 2 months, then 2 drugs x 4 mo” • (N.B. 2x/weekly dosing must be D.O.T.) Ref: PHAC. Canadian Tuberuclosis Standards, 6th Ed. 2007 p. 130 http://www.phac-aspc.gc.ca/tbpc-latb/pubs/pdf/tbstand07_e.pdf Access March 14, 2013. Treatment – Latent TB • INH – monitor LFTs – Hepatitis (rare < 20y.o.; >2% in >50y.o.) – Drug interactions! • RIF – GI toxicities, major drug interactions! – Huge inducer of cytochrome P450 Ref: PHAC. Canadian Tuberuclosis Standards, 6th Ed. 2007 p. 148 http://www.phac-aspc.gc.ca/tbpc-latb/pubs/pdf/tbstand07_e.pdf Access March 14, 2013. Which agents to use in active disease? • Pulmonary or extrapulmonary disease: – INH+RIF+PZA+ETB • If resistant to INH: – RIF+PZA+ETB (+FQ if severe) • If resistant to RIF: – INH+PZA+ETB+FQ • if resistant to INH and RIF: – PZA+ETB+FQ+amikacin • If resistant to INH, RIF and PZA or ETB – ETB (or PZA)+FQ+amikacin+two 2nd line agents Ref: Marc Riachi, RPh Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Anti-fungals Adapted from: Marc Riachi, RPh Drug info • • INH (inhibits formation of fatty acids found in the cell wall): – Bactericidal; penetrates cavitations – Hepatotoxicity (↑ with alcohol & rifampin) monitor LFTs – peripheral neuropathy (give vit B6) – GI symptoms, skin rash – ↑ phenytoin, carbamazepine & benzodiazepine blood levels RIF (inhibits mRNA synthesis): – Bactericidal; penetrates cavitations – Hepatotoxicity (↑ with alcohol) monitor LFTs – GI symptoms, skin rash – Pancytopenia – Colours urine, feces, saliva, tears orange may permanently stain contact lenses – Induces CYP450 Ref: Marc Riachi, RPh • • PZA (may inhibit mycobacterial metabolism): – Bactericidal in acid environment (in macrophages) – Hepatotoxicity (↑ with alcohol & rifampin) monitor LFTs – Hyperuricemia monitor uric acid – GI symptoms and arthralgias ETB (may inhibit cell wall synthesis): – Bacteriostatic – GI symptoms, hyperuricemia – Ocular toxicity and change in color perception monitor at high doses Antifungals • Topical • Oral – Azole anti-fungals • • • • • • Itra- (Sporanox), flu- (Diflucan), vori-, posaketoconazole (Nizoral) active vs. yeast and dermatophytes – Terbinafine (Lamisil) • active vs. yeast and dermatophytes – Nystatin • active vs. yeast only Ref: Marc Riachi, RPh – Ciclopirox • (cream, lacquer, shampoo), – nystatin • (cream, pv, oral suspension), – clotrimazole • (cream, pv), – miconazole • (cream, pv), – ketoconazole • (cream shampoo), – terbinafine • (cream, spray), – tolnaftate • (powder suitable for skin folds) • Injectables – usually require I.D. consult Which agents to use? • Onychomycosis: – oral terbinafine, oral itraconazole, ciclopirox lacquer (use lacquer only for mild distal form; expensive) • Fungal skin: – topical clotrimazole, topical miconazole, topical terbinafine, topical ketoconazole. Nystatin is ineffective vs. dermatophytes. Candidal skin infections respond to nystatin. Use topical azoles for tinea versicolor (not terbinafine). • Seborrheic dermatitis: – topical ciclopirox, ketoconazole • Oral candidiasis: – Oral nystatin swish and swallow (not absorbed from GI tract). Oral fluconazole. • Vulvovaginal candidiasis: – topical azoles, po fluconazole one dose (now available without a prescription), boric acid pv suppositories (very irritative) • Diaper rash: – Topical nystatin, clotrimazole, miconazole, or ketoconazole. Ref: Marc Riachi, RPh • • Drug info Terbinafine po: – Very active vs dermatophytes – headache, GI diarrhea, dyspepsia, abdominal pain – taste disturbance (may persist post treatment) – CYP2D6 inhibitor: • Decreases formation of active metabolites of tamoxifen • May ↓ breakdown of TCA’s, fluoxetine, paroxetine, fluvoxamine, sertraline, tamsulosin, mirtazapine, haloperidol, some beta blockers Azole antifungals po: – Itraconazole and ketoconazole particularly are strong inhibitors of CYP3A4 and so many drug interactions. Also hepatotoxic. Ketoconazole > itraconazole > terbinafine wrt hepatic toxicity. Itra may worsen heart failure symptoms. Ketoconazole is rarely used and is poorly tolerated; anorexia, nausea, vomiting high doses, and effects sexual function/sex hormones and steroidogenesis. – Fluconazole is considered a moderate inhibitor of CYP3A4 and so less clinically important drug interactions. Strong CYP2C9, 2C19 inhibitor. QT prolongation with amiodarone, clarithromycin, TCA’s. Bioavailability of PO similar to IV; use PO if possible. Ref: Marc Riachi, RPh Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Hypertension and BP Meds (The ABCD’s of HTN) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • List first line classes of medication for the treatment of essential hypertension • Explain how co-morbid indications may change your choice in therapy • Apply a rational approach in selecting therapy • Understand the dosing, monitoring and titration of key examples from each class of medication Rational Prescribing • Rational prescribing requires a process for selecting therapy: (in order) 1. 2. 3. 4. Efficacy Toxicity Cost Convenience A A B C D ARB ACEinh B-blockers CCB Diuretics (DHP-type) (Thiazide type) Angiotension Receptor Blocker Angiotensin Converting Enzyme Inhibitor Beta-Blocker Calcium Channel Blocker (dihydropyridine type) -sartan -pril -olol -dipine Losartan Valsartan Candesartan Etc Ramipril Enalapril Perindopril Etc Bisoprolol Metoprolol Atenolol Etc Amlodipine Nifedipine Felodipine Etc Chlorthalidone Hydrochlorothiazide Indapamide Etc Reduced sympathetic outflow, and heart rate Relaxation of coronary & peripheral arterial smooth muscle (not AV node!) Inhibits Na+ & Cl- reabsorption in the corticaldiluting segment of the ascending loop of Henle = diuresis. Reduction in systemic vascular resistance 1st line 1st line Blocks conversion of AT1 to ATII (ACEinh) or blocks ATII receptors (ARB) = Inhibition of vasoconstriction, aldosterone, catecholamine, and arginine vasopressin release, water intake, and hypertrophic responses (b1 receptor – in heart) (cardioselective ~ A-M) (b2 receptor – in lungs) (Non-selective ~ N-Z) (“one heart; two lungs”) Efficacy: 1st line 1st line 1st line (< 65y.o.) A A B C D Toxicity: Toxicity: Toxicity: Toxicity: Hypotension HyperK+ Acute renal failure (ARF) Angioedema Hypotension Bradycardia Bronchoconstric tion (in brittle asthmatics with noncardioselective bbl’s) Hypotension Edema Orthostatic hypotension Hypotension HypoNa+ HypoK+ ARF Monitor: SCr, K+, BP Monitor: BP, HR, RR Monitor: SCr, lytes, BP Cost: Generic - $$$ ODB covered Cost: Generic - $ ODB covered Cost: $ ODB covered Cost: Generic: $$$ ODB covered Cost: ¢ ODB covered Convenience: QD Losartan 25mg to 100mg Convenience: QD Ramipril 2.5mg to 10mg Convenience: QD Bisoprolol 2.5mg to 10mg Convenience: QD Amlodipine 2.5mg to 10mg Convenience: QAM Chlorthalidone 25mg Choosing Therapy • If efficacy (#1), cost (#3) and convenience (#4) are all more or less equivalent: – Choose based on potential Toxicities (#2) – Tailor the meds to the individual patient! • Evidence of efficacy is population based • Toxicities are individual. • Some combos are additive others synergistic BP lowering – Rarely clinically relevant – Can choose between groups A or B plus C or D (synergistic) • N.B. Choice will also be guided by various comorbidites Comorbidities Indication ARB ACEinh B C HTN (ALLHAT) MI (HOPE trial) CHF (CONSENSUS, SOLVD, ATLAS) DM2 (HOPE) (IDNT, IRMA-2, RENAAL) CVA (HOPE, PROGRESS) (LIFE, SCOPE, MOSES) PVD (HOPE) Afib D (VALIANT) (CAPRICORN, BHAT) (MERIT-HF, CIBIS II, COPERNICUS) (ALLHAT, PROGRESS) (Diltiazem) Second Line Therapy • What if you have used all available 1st line options? • 2nd line options: – – – – – – – Alpha blockers Spironolactone Hydralazine Nitrates Clonidine Beta-blockers (> 65 y.o.) etc. • ~ Equivalent efficacy – choose based on potential toxicity, cost or convenience factors. • Ensure that you balance these factors in their order of importance. Second Line Therapy • Alpha blockers – Eg. Terazosin, Prazosin, Doxazosin – Toxicity: Risk of orthostatic hypotension – Cost: cheap, generic – Convenience: only QD • Good 1st choice of 2nd line tx • Dual treatment of BPH & BP if also needed in male patients • Spironolactone – Efficacy: mortality benefit in late stage CHF (NYHA class III or IV) – Toxicity: risk of hyperK+ • esp with ARBs or ACEinh’s – Cost: cheap generic – Convenience: only QD • Hydralazine – MOA: direct vasodilation of arteries – Toxicity: orthostatic hypotension – Cost: cheap, generic – Convenience: QID dosing • Nitrates – eg. ISDN, ISMN, NTG – MOA: smooth muscle vasodilation of vasculature (veins > arteries); – Toxicity: headache, orthostatic hypotension, dizziness – Cost: cheap/ generic – Convenience: BID- QID dosing; Process 1. Start first drug 2. Increase to moderate dose 3. Monitor for efficacy (BP) and toxicity • If close to target: • Dose response curves – Flatten at top half – Less bang for your buck BP – increase dose • If far from target: – start new drug mg Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Oral Anti-hyperglycemics Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • List the classes of oral antihyperglycemic agents and understand their place in therapy. – Determine the relative efficacy, toxicity, cost and convenience of these agents before choosing therapy – Rationalize prescribing of oral hypoglycemics • Describe the current approach to pharmacologic management of type 2 diabetes. Diagnosis of IFG, IGT Category FPG 2-hour And/or after OGTT IFG 6.1-6.9 IFG (isolated) 6.1-6.9 IGT (Isolated) < 6.1 7.8-11.0 6.1-6.9 7.8-11.0 IFG and IGT N/A AND < 7.8 Can J Diabetes 2003;27(2);S11 Diabetes: complications MACROvascular Stroke Heart disease & hypertension MICROvascular Diabetic eye disease (retinopathy & cataracts) Nephropathy Peripheral vascular disease Neuropathy Foot problems Foot problems Kumamoto Study – HgbA1c & Complications Intensive vs. conventional insulin therapy (n=110) Median A1c - 7.1% vs. 9.4% 16 14 Retinopathy 16 14 12 Nephropathy 12 10 10 8 6 4 2 0 8 6 7% 5 6 7 7% 4 2 0 8 9 HbA1c (%) 10 11 5 6 7 8 9 HbA1c (%) 10 11 Prevention of Diabetes in IGT • Lifestyle modification – (see Finnish Diabetes Trial) – Moderate weight loss (5%) (esp. abd fat) – Regular physical activity • > 150 minutes per week – 58% RRR for type 2 Diabetes at four years • Pharmacotherapy – Multiple effective trials • Eg. LIFE trial - Losartan onset of new DM2 Can J Diabetes 2003;27(2);S12 Pharmacological Prevention Studies Study Drug DPP Metformin 850mg BID 2.8 31 STOPNIDDM Acarbose 100mg TID 3.3 30 DREAM Rosiglitazone 8mg daily 3.0 55 Orlistat 120mg TID 4.0 37 XENDOS Duration (years) RRR (%) Non-Pharmacologic Tx Mainstay of therapy! • Nutrition therapy – ↓ A1c 1-2% – CDA recommends counseling by a dietician for all type 2 diabetics – www.cvtoolbox.com diet for Type 2 diabetes Can J Diabetes 2003;27(2);S27 Pharmacotherapy Comparison of antihyperglycemics Drug Classes Sensitizers Secretagogues Other Drug Classes Sensitizers Secretagogues • Metformin • Glitazones • Sulfonylureas – Eg. Glyburide, Gliclazide • Meglitinides – Rosiglitazone (AVANDIA) – Pioglitazone (ACTOS) – Eg Repaglinide (GLUCONORM) Other • Alpha glucosidase inhibitors (Acarbose) • DPP4 inhibitors (Gliptins) • Sitagliptin (JANUVIA) • Saxagliptin (ONGLYZA) Incretin Analogues * Liraglutide (VICTOZA) (sc inj) * Exenatide (BYETTA) (sc inj) Drug Classes Sensitizers • Metformin • Glitazones – Rosiglitazone (AVANDIA) – Pioglitazone (ACTOS) • Sensitizers – reduce insulin resistance • Increase glucose uptake & utilization in muscle and adipose tissue • Reduce hepatic glucose output Drug Classes • ↑Basal & prandial insulin secretion, ↓hepatic gluconeogenesis • Doesn’t correct impaired 1st phase insulin secretion; primarily affects 2nd phase • Beta-cell sensitizer – primes glucose mediated insulin secretion (1st phase) Secretagogues • Sulfonylureas – Eg. Glyburide, Gliclazide • Meglitinides – Eg Repaglinide (GLUCONORM) Drug Classes Other • Alpha glucosidase inhibitors (Acarbose) • Competitive inhibitor of pancreatic α-amylase and intestinal brush border αglucosidases, resulting in delayed hydrolysis of ingested complex carbohydrates and disaccharides and absorption of glucose; • Dose-dependent reduction in postprandial serum insulin and glucose peaks; inhibits the metabolism of sucrose to glucose and fructose • DPP4 inhibitors (Gliptins) – (Sitagliptin (Januvia), Saxagliptin (Onglyza)) • Prolongs the action of endogenous incretin hormones by blocking their breakdown by the enzyme, dipeptidyl peptidase-4 (DPP-4). • This leads to more insulin release after eating. • Incretin Analogues – (Liraglutide (Victoza), Exenatide (Byetta)) (sc inj) • mimic endogenous incretin hormones Rational Prescribing • FOUR steps to Rational Prescribing: 1. EFFICACY 2. TOXICITY 3. COST 4. CONVENIENCE EFFICACY – Ask… 1. HARD Outcomes a) Any mortality benefit? b) Any morbidity benefit? Then, 2. SURROGATE Outcomes a) Clinically relevant? EFFICACY 1. HARD Outcomes – Mortality benefit » Metformin – UKPDS-34 trial – Morbidity 2. SURROGATE Outcomes a) Hgb-A1c • Blood glucose levels – Fasting or Prandial b) Insulin Sparing Effects Effect of Metformin on Event Rates in the UKPDS • Diabetes-related endpoint 32% p=0.002 • All-cause mortality 36% p=0.011 • MI / CVA • Diabetes-related death 42% p=0.017 – But.. When added early to sulfonylurea risk of DM-related death (?statistical anomaly?) EFFICACY A) Surrogate Outcome - Hgb-A1c – ~ 1% to 2% • • • • METFORMIN SULFONYLUREA’s REPAGLINIDE GLITAZONE’s (1% - 2%) (1% - 2%) (1% - 1.5%) (0.4% - 1.5%) – ~ 0.5% to 0.8% • • • ACARBOSE DPP4 inhibitors (‘GLIPTINS) NATEGLINIDE Nathan DM, et al. Diabetes Care 2008 (Dec);31:1-11. EFFICACY B) Surrogate Outcome - Insulin Sparing Effect – METFORMIN – ACARBOSE – GLITAZONE’s (Pioglitazone) – Gliptins (Sitagliptin, Saxagliptin) – Incretin Analogies (Liraglutide, Exenatide) = Weight neutral or weight negative = Reduction of hyperinsulinemia TOXICITY – Ask… 1. Serious / Fatal Side Effects 2. Bothersome / Common s.e. 3. Age? • • Newer agents = Less Safety Data Older agents = More Safety Data TOXICITY – Serious / Fatal • Glitazones • Secretatgogues – CHF – Fractures – M.I. (Sulfonylureas & Meglitinides) • (rosiglitazone) – Bladder Cancer • (pioglitazone) – Severe Hypoglycemia TOXICITY – Serious / Fatal • Metformin • ?Risk of Lactic Acidosis – 0.03 cases / 1000 pt-yrs – ~ 50% fatal – When implicated: • Metformin plasma levels are usually >5 μg/mL • Cases - primarily diabetics w/ significant renal insufficiency, both intrinsic renal disease and renal hypoperfusion, w/ multiple medical/surgical problems and multiple medications. Metformin Dosing • Dosing recommendations with renal insufficiency: – (CONTROVERSIAL) • CrCl 60ml/min→ – 1700 mg/day (Rxfiles) – 2.5g/day (Roland) • CrCl 30ml/min→ – 850mg/day (Rxfiles) – 2.5g/day (Roland) • CrCl < 30ml/min→ – Contraindicated (Rxfiles) – 1g/day (>20mL/min) (Roland) If NO other risk factors, else D/C. – Take home: assess OTHER RISK FACTORS for L.A. Risk Factors - Lactic Acidosis • Severe renal impairment – (caution if CrCl < 30ml/min) and • • • • • • • Hepatic disease alcoholism CHF COPD CRF Pneumonia Ongoing acidosis – Lactic, keto etc. TOXICITY - Bothersome 1) METFORMIN – GI upset / diarrhea – Start low, go slow! • Initial dose 250mg QDaily to BID – B12 / folate deficiency / anemia (6 - 8/100) • Reduced absorption – so, supplement – Anorexia – usually transient – Metallic taste TOXICITY - Bothersome 2) Sulfonylureas: – Sulfa skin reactions • Rash / photosensitivity ~1% – Weight gain (2-3kg) – Mild Hypoglycemia: • Most with glyburide. Least w/ glimepiride & gliclazide • Requires consistent food intake • Major episodes 1-2% (esp. in elderly) TOXICITY - Bothersome 3) Glitazones: – Edema 4) Meglitinides: – Hypoglycemia 5) Acarbose: – GI upset / diarrhea / bloating 6) Gliptins: • GI upset, edema, ?infection 7) Incretin analogues • N/V/D, ?infection Cost – Ask… • Patient cost vs societal cost • Rx cost? • ODB coverage? • Covered under other plans? Cost/tab – ODB covered? • Metformin • Glyburide • Gliclazide - $ 0.0587 - ODB - $ 0.0574 - ODB - $ 0.0931 - ODB – Gliclazide MR $ 0.1405 - ODB • • • • • Repaglinide Acarbose Sitagliptin Saxagliptin Pioglitazone - $ 0. - Section 8 (EAP) - $ 0.3584 - ODB - $ 2.8050 - ODB - No - $ 0. - Section 8 (EAP) Cost • From Rxfiles May 2010 • Cost per 100 days therapy (in Sask.) Convenience • PO vs IV? • QD vs QID? Convenience • • • • • • Gliptin’s - QD Glitazones - QD Sulfonylureas – QD to BID Metformin - QD to TID Meglitinides – QD to TID Acarbose – QD to TID with meals • 1st line – METFORMIN • 2nd line - SULFONYLUREA or INSULIN – Meglitinide – if poor CrCL or irregular eating • 3rd line - GLIPTINs or ACARBOSE if patients absolutely REFUSE insulin NEVER USE GLITAZONEs! Did I say, never? I meant NEVER! www.rxfiles.ca Individualization of Drug Therapy Patient Factor Consider→ Possibly preferred drugs Renal Failure Repaglinide (Gluconorm) Also: gliclazide, insulin Hepatic Disease Insulin, repaglinide, acarbose Caution: glyburide, metformin, glitazones Hyoglycemia Metformin, Acarbose Also, repaglinide, nateglinide, gliclazide, glimepiride; Obese Metformin, Acarbose Irregular Mealtimes Repaglinide (may be preferred over SU) PPBG >10mmol/L and FBG minimally ↑’d Repaglinide or Acarbose Insulin lispro (Humalog) if PPBG very high Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Insulins Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 New Drugs/Drug News vol 24 (3): May/June 2006 Insulins - Simplified • Long = Basal • Short = Prandial – NPH, (N) – Glargine (Lantus) – Detemir (Levemir) – Short • Regular (R) • Toronto – Rapid • Lispro (Humalog) • Aspart (NovoRapid) • Glulisine (Apidra) • Premixed • 30/70 (and 10/90, 20/80, 40/60, 50/50) • Humalog Mix-25, NovoMix-30 Which to choose? Basic Concepts • Hyperglycemia = Chronic Hypoglycemia = Acute – So, go after Hypo’s first! • Fed: 6h/24h = 25% • Fasting: 18h/24h = 75% – So, go after Fastings first! • AM affects PM & HS – So, go after AM first! 1. ?Any hypo’s?- fix ‘em! then, 2. FBS AM 3. FBS Noon 4. FBS PM 5. FBS HS then, 6. 2h PPG AM 7. 2h PPG Noon 8. 2h PPG PM Insulins • Long – Basal – NPH, (N) – Glargine (Lantus) – Detemir (Levemir) • Short – Prandial – Short • Regular (R) • Toronto – Rapid • Lispro (Humalog) • Aspart (NovoRapid) • Glulisine (Apidra) • Premixed • 30/70 (and 10/90, 20/80, 40/60, 50/50) • Humalog Mix-25, NovoMix-30 (R + NPH) (Rapid + NPH) Now, which to choose? Rational Prescribing • FOUR steps to Rational Prescribing: 1. EFFICACY 2. TOXICITY 3. COST 4. CONVENIENCE Long – Basal Insulins • Efficacy: – NPH = Lantus = Levemir = NPH – Equivalent • Morbidity benefits, A1c lowering effect – Despite the marketing: • Kinetics don’t affect overall efficacy: – Slowest absorption: Thigh (best for basal insulins) – Fastest absorption: Abdomen (best for prandial insulins) • Lots of Lantus is injected BID • NPH can be used QHS for some Long – Basal Insulins • Toxicity: – All: • Hypoglycemia – NPH: • Peak effect at ~ 8hrs (4-10hrs) – Risk of hypoglycemia (~ 5%? vs “peakless” insulins) – Lantus / Levemir: • Insulin analogues • Increased breast cancer risk? – more research needed Long – Basal Insulins • Cost: – All: covered under ODB • N.B. No Rx required for any insulins – all OTC – NPH: ~ $40 – Lantus: ~ $90 – Levemir: ~ $100 • Convenience: – All sc injections, via penfills – All QD – BID Bottom Line – Basal Insulins • All equivalent • Choose therapy based on cost (NPH) – For the very small proportion suffering from hypoglycemia due to the peak effect of NPH or lamenting BID dosing, consider Lantus or Levemir. Starting Basal Insulin • Fancy Way: – calculate unit/kg dose = 0.1 - 0.2u/kg/day sc • Risk hypoglycemia on first dose – lose your patient’s buy-in forever. • Primary Care Method: – Initiate 5u or 10u qhs sc – Titrate by 1-2u q3-4d until AM FBS = 4 - 7 mmol/L • 10% titrations – If dose = 30’s – increase by 3 units – If dose = 40’s – increase by 4 units – etc. etc. Rx 1. NPH – Sig: 5u qhs sc or ud – M: 1 box penfills – Repeat x 12 2. Needle tips – 28G - 6mm – Sig: ud – M: 1 box – r x 12 • N.B. (Please teach pt pen technique) Insulins • Long = Basal – NPH, (N) – Glargine (Lantus) – Detemir (Levemir) • Short = Prandial – Short • Regular (R) • Toronto – Rapid • Lispro (Humalog) • Aspart (NovoRapid) • Glulisine (Apidra) • Premixed • 30/70 (and 10/90, 20/80, 40/60, 50/50) • Humalog Mix-25, NovoMix-30 (R + NPH) (Rapid + NPH) Short – Prandial Insulins • Efficacy – Equivalent reduction in morbidity, HgbA1c Short – Prandial Insulins • Toxicity – Hypoglycemia – Rapid insulins better reflect physiological effect of pancreatic insulin (vs Regular insulin) • More important in CKD (=longer insulin t½ ) Short – Prandial Insulins • Cost – All covered under ODB • • • • Regular (R) / Toronto ~ $40 NovoRapid (aspart) ~ $56 Humalog (lispro) ~ $55 Apidra (glulisine) ~ $48 • Convenience – All injected with meals – Regular insulin injected 30-45 min before meal – Rapid insulin can be taken with meal • Reduced risk of hypo if pt injects, then forgets to eat Bottom Line – Prandial Insulins • All equivalent • Choose therapy based on cost / familiarity – Rapid insulins reflect pancreatic insulin release better than [R]/Toronto. – The worse the CrCL, the more important this fact becomes. Starting Prandial Insulin • Fancy Way: – Total dose: 0.5u/kg – 40% of total dose - basal insulin qHS – 20% of total dose TID with meals (60%) – prandial insulin 1530 min before meals • Eg. 80kg pt – 0.5u/kg = 16u basal (40%); 8u TID (20% x 3 = 60%) • Primary Care Method: – Start 5u sc with meals • Titrate AM to HS to target – Monitor 2h PPG • Start injection TID or only single meal as required – If poor control: inj TID sc; If mediocre control: inj qAM sc • Still aim for ~ 2/3rds split (40% basal / 60% prandial) Insulins • Long = Basal – NPH, (N) – Glargine (Lantus) – Detemir (Levemir) • Short = Prandial – Short • Regular (R) • Toronto – Rapid • Lispro (Humalog) • Aspart (NovoRapid) • Glulisine (Apidra) • Premixed • 30/70 (and 10/90, 20/80, 40/60, 50/50) (Reg + NPH) • Humalog Mix-25, NovoMix-30 (Rapid + NPH) Pre-mixed Insulins • NovoMix-30 = Humalog Mix25 (equivalent) • Efficacy – All ~ 30% short / 70% long • Toxicity – Hypoglycemia (less with Rapid vs Regular insulin) • Cost: ~$53 (Rapids) ~$40 (Regular 30/70) • Convenience ~ Rapids can be injected with meal Starting Pre-mixed Insulins • Fancy Way: – Estimate total starting daily dose • (0.3-0.6 units/kg) – Divide daily dose: • 2/3 before breakfast; 1/3 before supper • Primary Care Method: – From scratch: Start 5-10u QD-BID and titrate – From other insulins: Calculate approximate amount of basal and prandial units and divide 2/3rd - 1/3rd AM and PM Pearls • Insulin is 2nd line after metformin – No need to save it for last! • Better than adding a 3rd PO drug – Better efficacy, lower toxicity, better studied • Improve buy-in from patient: – “Natural” supplement – Only BID glucochecking at alternating times required: • • • • • • • FBS AM + PPG AM, then FBS AM + FBS noon, then FBS AM + PPG noon, then FBS AM + FBS PM, then FBS AM + PPG PM, then FBS AM + FBS HS repeat Pearls (cont’d) • D/C secretagogues after starting insulin to reduce risk of hypo’s. – Eg. Sulfonylureas, meglitinides – Black box warning against combo with glitizones! (Actos, Avandia) Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD Anti-Dyslipidemic Drugs (So simple it hurts) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • List the 4 steps in rationalizing drug therapy choices using evidence based medicine. • List the important parameters in choosing anti-dyslipidemia drugs in a clinical setting. • Identify clinically important differences in the efficacy, toxicity, cost and convenience of different anti-dyslipidemics. • Recognize the inherent weaknesses of current guidelines. Rational Prescribing Process • FOUR steps to Rational Prescribing: 1. EFFICACY 2. TOXICITY 3. COST 4. CONVENIENCE Choosing Anti-dyslipidemics • First, define your options: 1. Statins (HMG-CoA Reductase inhibitors) • Prava-, Fluva-, Simva-, Atorva-, Rosuva-statin 2. Fibrates • (The exact mechanism of action of gemfibrozil is unknown; Theories re: the VLDL effect; it can inhibit lipolysis and decrease subsequent hepatic fatty acid uptake as well as inhibit hepatic secretion of VLDL; together these actions decrease serum VLDL levels; increases HDL-cholesterol; the mechanism behind HDL elevation is currently unknown) • Feno-, Beza-, Clo-fibrate, & Gemfibrozil 3. Ezetimibe • (Inhibits absorption of cholesterol at the brush border of the small intestine via the sterol transporter, Niemann-Pick C1-Like1 (NPC1L1)). 4. Niacin 5. Cholestyramine • (Bile acid sequestrant) Efficacy – Endpoints? • Hard Endpoints – Reduction in mortality • Fatal MI, Fatal stroke – Reduction in morbidity • Non-fatal MI, non-fatal stroke, reduction in hospitalization • Soft Endpoints – Reduction in plaque size – Reduction in lipid panel values – etc Efficacy • Only statins have any proven reduction in hard endpoints. The End. Who cares about lipid panel numbers going up and down if they don’t affect morbidity or mortality? So….why bother with the Toxicity, Cost or Inconvenience of any others? Can J Cardiol Vol 25 No 10 October 2009 Cdn Dyslipidemia Guidelines 2009 Can J Cardiol Vol 25 No 10 October 2009 Cdn Dyslipidemia Guidelines 2009 Can J Cardiol Vol 25 No 10 October 2009 Pharmacotherapy • “The majority of patients will be able to achieve target LDL-C levels on statin monotherapy.” • “Clinical outcome data on the incremental benefit of combination therapy with statin plus ezetimibe, niacin or fibrate, versus statin monotherapy are lacking, although clinical trials are underway to examine this issue.” Can J Cardiol Vol 25 No 10 October 2009 Correlation versus Causation Why statins? • Lipid lowering effects vs • Pleiotrophic effects – Plaque stabilizing – Anti-inflammatory – Improved endothelial cell function – Inhibition of thrombogenic response Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol. 2005;45:89-118. see: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2694580/?tool=pubmed Accessed Apr 25/12. So? • So…. • If equivalent LDL lowering with non-statin drugs have no effect on morbidity or mortality then LDL may only be a surrogate marker of the pleiotrophic effects of statins. Bottom Line • Being on any statin at any dose is the most important thing. • Being on the highest dose of statin that a patient can tolerate is secondary. – Doubling the statin dose only lowers LDL by 6% – Pushing the statin dose to levels that result in side effects is just not worth it. Non-compliance will result. • The LDL target is just your guide. Exceptions • Gemfibrozil – Two trials that show reduction in CVD events • Helsinki Heart Study (HHS) • Veterans Administration HDL Intervention Trial (VA-HIT) – Never combine it with statins • Serious risk of rhabdomyolysis • N.B. Fenofibrate – No effect on CVD events • Fibrates for high TGs – reduce risk of pancreatitis • Fibrates for high TGs – treatment of gout Statin + Fibrate (ACCORD-Lipid Trial) • No difference in vascular (hard) outcomes. – Almost a difference in lipids values (ie. soft outcomes) – ?Possible vascular harm in women? [9.1% vs 6.6%] Rxfiles.ca ACCORD Lipid & BP Trial Overview Sept 2010. Accessed Apr 26/12. Statin + Ezetimibe (Lipid-ENHANCE Trial) • No hard endpoints reported. • Even intima-media thickness non-significant – IMPROVE-IT Trial still ongoing (expected 2013) – “Dr Steven Nissen (Cleveland Clinic, OH) questioned whether the trial would be completed because more than 5000 hard clinical end points are needed for the study to reach statistical significance, an unusually high number given that past studies required a few hundred events.” (see: http://www.theheart.org/article/1064755.do ) Rxfiles.ca. ENHANCE Trial Summary, June 2008. Accessed Apr 26/12. Statin + Niacin (AIM-HIGH Trial) • “ …stopped early for futility.” – 3414 patients • Earlier Statin + Niacin studies had only showed reduction in soft endpoints. – Eg. Regression of carotid atherosclerosis Rxfiles.ca. AIM-HIGH Trial Summary, Dec 2011. Accessed Apr 29/12. Michael O'Riordan. AIM-HIGH fell short, leaving experts looking for reasons in new review. Heart.org APR 19, 2012. Accessed Apr 25/12 Treatment Populations • Who gets statins? – Secondary prevention – Primary prevention? – Moderate risk?? – Put it in the water??? Secondary Prevention • Clear efficacy • Reduction of mortality • Reduction of morbidity • Benefit in as little as one year – (usually 4-5 years) Primary Prevention • Clear efficacy in High Risk Framingham • Reduction in morbidity • No effect on mortality Primary Prevention (never had an MI or Stroke) • High risk Framingham patients with history of: – Diabetes – CKD – CHF – Angina – PVD – CABG or PCI – Metabolic syndrome – Score > 20% Moderate Risk • Likely not worthwhile… • BUT, the JUPITER trial = reduction in hard endpoints! – Patients with low/normal cholesterol and high CRP – Relative Risk Reduction ~ 50%! – But the Absolute Risk Reduction was tiny! – hsCRP can differentiate between higher- and lowerrisk Moderate Category Framingham patients Ridker PM, et al. the JUPITER Study Group. Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. N Engl J Med. 2008 Nov 9. Rosuvastatin: 22/8901 (0.28%) of non-fatal MI JUPITER trial N Engl J Med 2008;359:2195-207. Placebo: 62/8901 (0.70%) of non-fatal MI Relative vs Absolute Risk Time to Benefit • How old is too old to start therapy? – Upper ages of trials ~ 80-83 yrs old. – …Add time to divergence of survival curves • ~ 4 to 6 years… plus • ?Prognosis • Older than 85y.o, don’t start? – Already on it, don’t stop, but don’t bother checking LDL either. Pharmacotherapy • “The majority of patients will be able to achieve target LDL-C levels on statin monotherapy.” • “Clinical outcome data on the incremental benefit of combination therapy with statin plus ezetimibe, niacin or fibrate, versus statin monotherapy are lacking, although clinical trials are underway to examine this issue.” Can J Cardiol Vol 25 No 10 October 2009 “…Trials (were) Underway…” • Statin + Niacin trials: • AIM-HIGH trial – Stopped early. No benefit from niacin in HDL raising. • See: http://www.theheart.org/article/1231453.do – Known risk of hepatotoxicty with Niacin and significant flushing. • HPS2-THRIVE trial (statin + ER Niacin/Laropiprant) – No benefit (n = 25673) • See: http://www.theheart.org/article/1515533.do Toxicity • Statin – Rare/Severe: • Myopathy, even Myositis/Rhabdomyolysis • Hepatotoxicty • Memory impairment • ?Diabetes?? – discuss – Common/Bothersome: • Myalgias • Fibrates – Same as above • Ezetimibe – Same as above • Niacin – +++ flushing – Hepatotoxicity (esp with long acting form – Niaspan) Cost • All statins covered under ODB • All statins are generic Convenience • Older statins require QHS dosing – Cholesterol synthesis mostly occurs late at night • New statins last long enough to be dosed daily at any time • Lacking grapefruit juice interaction: – Rosuvastatin, fluvastatin, pravastatin • (non 3A4 P450 metabolism) Comments, Questions & Requests? • [email protected] • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD