* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Microbial physiology
Survey
Document related concepts
Bacterial cell structure wikipedia , lookup
Infection control wikipedia , lookup
Gastroenteritis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Disinfectant wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Neonatal infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Transcript
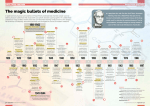
Antibiotics 楊倍昌 Antibiotics and vaccines are among the biggest medical advances since 1000. (Culver Pictures) A brief history of antibiotics • • • • • • • • • • • 1495, mercury to treat syphilis. 1630, quinine (cinchona tree) for malarial fever by South American Indians. 1889, Buillemin defined antibiosis. 1910, Paul Ehrlich developed arsenical compound (Salvarsan) for syphilis, term: the chemical knife. 1929, Alexander Fleming found penicillin. 1935, Gerhard Domagk showed the value of sulfonamides. 1940, Ernst Chain and Howard Flory demonstrated the effect of penicillin. 1940-1970, then searching for new antibiotics ~ recent year: modifying old drugs, finding new discipline in antibacterial combats Early time in war: thanks penicillin, we can go home now Now a day……….Oh eh?! Thanks to work by Alexander Fleming (1881-1955), Howard Florey ( 1898-1968) and Ernst Chain (1906-1979), penicillin was first produced on a large scale for human use in 1943. At this time, the development of a pill that could reliably kill bacteria was a remarkable development and many lives were saved during World War II because this medication was available. A. Fleming E. Chain H. Florey A tale by A. Fleming • He took a sample of the mold from the contaminated plate. He found that it was from the penicillium family, later specified as Penicillium notatum. Fleming presented his findings in 1929, but they raised little interest. He published a report on penicillin and its potential uses in the British Journal of Experimental Pathology. Scenario of penicillin action on E. coli 1 2 3 6 5 4 1: ordinary appearance 2-4: globular extrusions emerge 5: rabbit-ear forms 6: Ghost form Natural products, including: toxins, antibiotics (about 70% of all known antibiotics) , antifungals, etc, have historically been isolated and characterized from heterotrophic bacteria (e.g. Streptomyces). This was primarily due to the ease with which these organisms can be grown and manipulated in the laboratory. Evaluation by BUSINESS COMMUNICATIONS COMPANY, INC., year By 2001, in developed countries, as many as 60% of hospital-acquired infections are caused by drug-resistant microbes. These infections are no longer found only in hospital or nursing home wards but are active in the community at large. An ideal antibiotics • Broad-spectrum • Did not induce resistance • Selective toxicity, low side effects • Preserve normal microbial flora Susceptibility test • Tube dilution method • • Minimal inhibitory concentration (MIC): the smallest amount of chemotherapeutic agent required to inhibit the growth of organism in vitro Disk diffusion method • Zone of inhibition (ZOI): the correlation of ZOI and MIC has been established by FAD ETest. This commerciallyprepared strip creates a gradient of antibiotic concentration when placed on an agar plate Guidance of antimicrobial therapy • Minimum inhibitory concentration: lowest concentration of antibiotic that inhibits visible growth (難用) • Minimum bactericidal concentration: lowest concentration of antibiotic that kills 99.9% of the inoculum • Serum bactericidal title: dilution of serum that kills 99.9% of the inoculum • Synergy test: synergistic activity of multiple antibiotics In vitro: Factors for optimal antibiotic action • pH of environment: • Nitrofurantoin is more active in acid pH; sulfonamides and aminoglycoside are more active in alkaline pH. • Components of medium: • Anionic detergents inhibit aminoglycosides, serum proteins bind to penicillin in varying degrees. • Stability of drug: • • Aminoglycosides and chloramphenicol are stable for long period in vivo. Size of inoculums: • The larger the bacterial inoculum, the greater the chance for resistant mutant to emerge. • Metabolic activity of microorganisms: • Actively and rapidly growing organisms are more susceptible to drug action Affecting factors in vivo • Abscess: circulation is blocked off. • Foreign bodies: obstruction of the urinary, biliary or respiratory tracts etc. • Immunity. Diagrammatic representation of the results of treatment related to specific chemotherapy Patients with normal immunity and uncomplicated mild to moderate infections Patients with serious lifethreatening infections Sites of action For lecture only BC Yang Modes of action (1) • Penicillins, cephalosporin, bacitracin, carbapenems and vancomycin. vancomycin • • Tetracyclines Inhibitors of Cell Membrane. Polyenes - Amphotericin B, nystatin, and condicidin. Imidazole - Miconazole, ketoconazole and clotrimazole. Polymixin E and B. Amphotericin Aminoglycosides Inhibitors of cell wall synthesis. Inhibitors of Protein Synthesis. Aminoglycosides - Streptomycin, gentamicin, neomycin and kanamycin. Tetracyclines - Chlortetracycline, oxytetracycline, doxycycline and minocycline. Erythromycin, lincomycin, chloramphenicol and clindamycin. Modes of action (2) • Inhibitors of metabolites (Antimetabolites). Sulfonamides - Sulfanilamide, sulfadiazine silver and sulfamethoxazole. Trimethoprim, ethambutol, isoniazid. • Inhibitors of nucleic acids (DNA/RNA polymerase). Quinolones - Nalidixic acid, norfloxacin and ciprofloxacin. Rifamycin and flucytosine. rifamycin Penicillin: an extensively studied example Action mechanism of penicillin • Action target: cell wall • on penicillin binding proteins (PBPs) • Transpeptidases (form cross-links in peptidoglycan) • Beta-lactam ring attached to 5-membered thiazolidine ring • Accessibility of PBPs differ in gram+ and gram- bacteria • Amino acyl side chain groups determine spectrum, adsorption, susceptibility to lactamase • Bactericidal inhibitors Pharmacokinetics of penicillin • Adsorption: can be oral • Stability in acid condition: • Amoxicillin (yes) • PenG (no) • Nafcillin (yes) • Pen V (yes) • Piperacillin (no) • Ampicillin (yes) • Distribution: to most body sites; not in CSF unless inflamed meninges Excretion: rapid eliminated by renal secretion • Clinical status of Penicillins (empirical) • Pen G (Pen V): natural • • Nafcillin: penicillinase-resistant • • Staphylococci epidemic; bacteremia, septiemia Ampicillin: • • Common strptococci (S. pneumoniae; S. pyrogenes); URTI, pneumonia meningitis, prophylaxis of rheumatic fever Gram- spectrum: E. coli; H. influenzae;Salmonella, shigella pharngitis, otitis media, UTI, gastroenteritis Peperacillin: • Expanded spectrum/antipsuedomonal, enteric bacilli; Systemic infection in hospitalized patients (gram-, P aeruginoma) Combinations with b-lactamase inhibitors: URTI, pneumonias, meningitis, bacteremia Resistance • • • • Failure to bind to PBPs Cannot penetrate porins (gram-) Production of lactamase (penicillinase) Lack autolytic enzyme • B-lactamase • Types: • • • • Different substrate specificity Penicillinases cephalosporinases Metallo-b-Lactamase Location: • • Gram+: extracellularly Gram-: periplasmic space Serine-b-Lactamase By Dr. Osnat Herzberg University of Maryland Biotechnology Institute (UMBI) Adverse effects • Thrombophlebitis • Allergic reactions • Superinfections (diarrhea) • Seizures (rare) Wickens K, Pearce N, Crane J, Beasley R. Antibiotic use in early childhood and the development of asthma. Clin Exp Allergy 1999;29:766-771. Before on antibiotics: – Antibiotics act as powerful selective factors in the emergence and spread of resistant microorganisms. In Rwanda 聯合報 八十五年 四月十三日 頭版新聞 Resistances • • Natural (inherent) resistance • Structural barrel • Lack of target • Transport system Acquired resistance • Mutation • Gene exchange (conjugation in most) Transferable antibiotic resistance in bacteria • Reduced uptake into cell (chloramphenicol) • Active efflux from cell (tetracycline) • Modification of antibiotic targets (b-lactam, erythromycin) • inactivation of antibiotic by enzyme modification: hydrolysis (b-lactam, erythromycin); derivatization (aminoglycosides) • Sequestration of antibiotic by protein binding (b-lactam) • Metabolic bypass (sulfonamides) • Overproduction of antibiotic target (titration: sulfonamides) Use of antibiotics; is it properly applied? • Acute infections in outpatients • Acute infections in hospitalized patients • Chronic infection (tuberculosis, AIDS) • Agriculture/veterinary medicine Some probable overuse/misuse of antibiotics • • • • • • Prophylactic use before surgery Empiric use (blinded use) Increased use of broad spectrum agents Pediatric use for viral infections Patients who do not complete course (chronic disease, e.g. TB, AIDS) Antibiotics in animal feeds Policy to deal drug resistance (1) • Ideally, bacteriological management of clinical infection should involve: • Identification of causative organism • Sensitivity test • Follow-up the drug effect • Monitor antibiotic level to avoid toxicity. • In reality, most patients requiring antimicrobial therapy are treated empirically. In serious infections immediate chemotherapy may be life-saving. Policy to deal drug resistance (2) • Periodic changes of antibiotics used might change selective pressure and thus avoid the emergence of resistance and retain the therapeutic value of antibiotics over a longer period. • The unnecessary prophylactic or animal feeds use should be discouraged. • Distribution of information on current/updated infectious microbes (consult microbiologists): use more targeted antibiotics • Patient education (不隨便吃藥, 停藥) New antibiotics development • Pharmaceutical industry putting resources back into discovery • Liaisons with university researches • Discoveries in microbial physiology and genetics offering new targets, new disciplines • Combinational chemistry (mass screening)