* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PATHOPHYSIOLOGY OF CONGENITAL HEART DISEASE
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Heart failure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Aortic stenosis wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Congenital heart defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
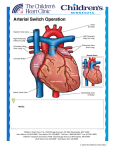
Dextro-Transposition of the great arteries wikipedia , lookup
PATHOPHYSIOLOGY OF CONGENITAL HEART DISEASE OBJECTIVES: At the end of the lecture students will be able to understand and describe the Pathophysiology of: Congenital heart defects Acyanotic heart diseases Cyanotic heart diseases Left to right shunts Right to left shunts CONGENITAL HEART DEFECTS Faulty embryogenesis (week 3-8)þ Usually MONO-morphic (i.e., SINGLE lesion) (ASD, VSD, hypoRV, hypo-LV) May not be evident until adult life (Coarctation, ASD) Overall incidence 1% of USA births INCREASED simple early detection via non invasive methods, e.g., US, MRI, CT, etc. Incidence per Million Live Births % 4482 42 Atrial septal defect Pulmonary stenosis 1043 10 836 8 Patent ductus arteriosus 781 7 Tetralogy of Fallot 577 5 Coarctation of aorta 492 5 Atrioventricular septal defect Aortic stenosis 396 4 388 4 Transposition of great arteries Truncus arteriosus Total anomalous pulmonary venous connection Tricuspid atresia 388 4 136 1 120 1 MALFORMATION Ventricular septal defect GENETICS Gene abnormalities in only 10% of CHD Trisomies 21, 13, 15, 18, XO Mutations of genes which encode for transcription factorsTBX5ASD,VSD NKX2.5ASD Region of chromosome 22 important in heart development, 22q11.2 deletionconotruncus, branchial arch, face ENVIRONMENT RUBELLA TERATOGENS CONGENITAL HEART DISEASE Congenital heart disease is often divided into two types: Cyanotic (blue discoloration caused by a relative lack of oxygen) non-cyanotic LR SHUNTS: all “D’s” in their names NO cyanosis Pulmonary hypertension SIGNIFICANT pulmonary hypertension is IRREVERSIBLE RL SHUNTS: all “T’s” in their names CYANOSIS (i,.e., “blue” babies) VENOUS EMBOLI become SYSTEMIC OBSTRUCTIONS LR ASD VSD ASVD PDA CONGENITAL HEART DISEASE Non-cyanotic: (left to right shunt) Ventricular septal defect (VSD) Atrial septal defect (ASD) Patent ductus arteriosus (PDA) Aortic stenosis Pulmonic stenosis Coarctation of aorta Atrioventricular canal (endocardial cushion defect) ASD NOT patent foramen ovale Usually asymptomatic until adulthood SECUNDUM (90%): Defective fossa ovalis PRIMUM (5%): Next to AV valves, mitral cleft SINUS VENOSUS (5%): Next to SVC with anomalous pulmonary veins draining to SVC or RA Sinus venosus defect: high in the septum. Ostium secundum defect: midseptum. Ostium primum defect: low in the septum. Pathophysiology: L-R shunt-increased flow across Rt heart-RV & PA enlargement. Clinical features: asymptomatic, slow wt gain, Diagnosis: Rt ventricular heave, systolic murmur, fixed wide split S2. ATRIAL SEPTAL DEFECT ATRIAL SEPTAL DEFECT VSD By far, most common CHD defect Only 30% are isolated Often with TETRALOGY of FALLOT 90% involve the membranous septum If muscular septum is involved, likely to have multiple holes SMALL ones often close spontaneously LARGE ones progress to pulmonary hypertension. VENTRICULAR SEPTAL DEFECT Most common CHD (26%),may be single or multiple Pathophysiology: Lt-Rt shunt as long as pulmonary vascular resistance is lower than systemic resistance, if reverse shunt reverses Large defects lead to pul. hypertension-Eissenmenger syndrome. Clinical features: depend on size, asymptomatic, growth failure, recurrent LRTI, congestive heart failure, Diagnosis: pansystolic murmur, Asymptomatic if defect is small. Heart failure with dyspnea, frequent respiratory infections, and poor growth if defect is large. Pansystolic murmur maximal at the left sternal border. PDA 90% isolated HARSH, machinery-like murmur LR, possibly RL as pulmonary hypertension approaches systemic pressure Closing the defect may be life saving Keeping it open may be life saving (Prostaglandin E1). Why? Ans: TGA, TA, TAPVC Connection between PA & descending aorta 10% of CHD Pathophysiology: Lt-Rt shunt, reverses if pulmonary resistance increases-RV enlargement. If PDA is large Eissenmenger syndrome can develop Clinical features: depend on size & direction of flow, slow growth Diagnosis: bounding pulse, continous murmur, loud S2 Murmur usually systolic, sometimes continuous, “machinery” Poor feeding, respiratory distress, and frequent respiratory infections in infants with heart failure Physical exam and echocardiography AVSD Associated with defective, inadequate AV valves Can be partial, or COMPLETE (ALL 4 CHAMBERS FREELY COMMUNICATE)þ COMPLETE ATRIOVENTRICULAR CANAL RL Tetralogy of Fallot Transposition of great arteries Truncus arteriosus Total anomalous pulmonary venous connection Tricuspid atresia CONGENITAL HEART DISEASE Cyanotic: (right to left shunt) Tetralogy of Fallot Transposition of the great vessels Tricuspid atresia Total anomolous pulmonary venous return Truncus arteriosus Hypoplastic left heart Pulmonary atresia Some forms of total anomalous pulmonary venous return Ebstein’s anomaly RL SHUNTS TETRALOGY of FALLOT most COMMON 1) VSD, large 2) OBSTRUCTION to RV flow 3) Aorta OVERRIDES the VSD 4) RVH SURVIVAL DEPENDS on SEVERITY of SUBPULMONIC STENOSIS Can be a “PINK” tetrology if pulmonic obstruction is small, but the greater the obstruction, the greater is the RL shunt TETRALOGY OF FALLOT Pulmonary stenosis VSD of the membranous portion Overriding aorta Right ventricular hypertrophy due to shunting of blood Addition of an atrial septal defect falls in the category of Pentalogy of Fallot. Hypoxic spells and squatting. Cyanosis and clubbing. Addition of an atrial septal defect falls in the category of Pentalogy of Fallot. Hypoxic spells and squatting. Cyanosis and clubbing. TGA (TRANSPOSITION of GREAT ARTERIES) NEEDS a SHUNT for survival, obviously PDA or PFO (65%), “unstable” shunt VSD (35%), “stable” shunt RV>LV in thickness Fatal in first few months Surgical “switching” Aorta from right ventricle, pulmonary artery from left ventricle Cyanosis from birth, hypoxic spells sometimes present Heart failure often present Cardiac enlargement and diminished pulmonary artery segment on x-ray Anatomic communication must exist between pulmonary and systemic circulation, VSD, ASD, or PDA. TRUNCUS ARTERIOSUS Single large vessel overrides the ventricular septum and distributes all the blood ejected from the heart. Large VSD is present. TRICUSPID ATRESIA Tricuspid valve is completely absent in about 2% of newborns with congenital heart disease. Blood flows from right atrium to left atrium through foramen ovale. Early cyanosis. Hypoplastic RV Needs a shunt, ASD, VSD, or PDA High mortality. Total Anomalous Pulmonary Venous Connection (TAPVC) PULMONARY VEINS do NOT go into LA, but into L. innominate v. or coronary sinus Needs a PFO or a VSD HYPOPLASTIC LA Pulmonary veins do not make a direct connection with the left atrium. Blood reaches the left atrium only through an atrial septal defect or patent foramen ovale. Pulmonary congestion, tachypnea, cardiac failure, and variable cyanosis. OBSTRUCTIVE CHD COARCTATION of aorta Pulmonary stenosis/atresia Aortic stenosis/atresia PULMONARY STENOSIS No symptoms in mild or moderately severe lesions. Cyanosis and right-sided heart failure in patients with severe lesions. High pitched systolic ejection murmur maximal in second left interspace. Ejection click often present. COARCTATION OF AORTA • • • • • M>F But XO’s frequently have it INFANTILE FORM (proximal to PDA) (SERIOUS) ADULT FORM (CLOSED DUCTUS, i.e., NO PDA) Bicuspid aortic valve 50% of the time AORTIC STENOSIS/ATRESIA VALVULAR If severe, hypoplastic LVfatal SUB-valvular (subaortic)þ Aortic wall THICK BELOW cusps SUPRA-valvular Aortic wall THICK ABOVE cusps in ascending aorta Asymmetric Septal Hypertrophy (Idiopathic Hypertrophic Subaortic Stenosis)