* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Document
Hookworm infection wikipedia , lookup
West Nile fever wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Trichinosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Neonatal infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Schistosomiasis wikipedia , lookup
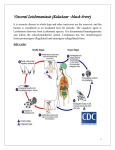
Hospital-acquired infection wikipedia , lookup
Case presentation Case 15 Reporter: I2 姚信宇 Date: 94/11/14 Chief complaint, present illness, & personal/past/family history A 24-year-old male Pakistani medical resident was seen in the emergency department at midnight; he was acutely ill with weakness, fever, abdominal pain, and diarrhea. He had visited relatives in Pakistan several months earlier. He had recently lost 20 lb inexplicably. Physical examination Physical examination revealed hepatomegaly, splenomegaly, and lymphadenopathy. The patient had darkened areas of skin on his forehead and around his mouth. Laboratory tests Anemic, with a hemoglobin level of 10 g/dl. Leukopenia and thrombocytopenia. Liver enzyme levels were slightly elevated. Giemsa-stained buffy coat smears: a few macrophages containing oval, nonflagellated protozoan forms, about 2 to 3 μm long(Fig.15.1). A large nucleus, a small kinetoplast, and an axoneme were visible in several parasites. Fig.15.1 Leishmaniasis (利什曼原蟲病) Intracellular amastigotes in macrophages of humans and other mammalian hosts . Extracellular promastigotes in the gut of sandfly vectors. Leishmaniasis (利什曼原蟲病) In humans and other susceptible mammals: in cells of reticuloendothelial origin as intracellular amastigotes, which are 2 to 3 m in length, oval or round, and lack an flagellum. Leishmaniasis (利什曼原蟲病) In Wright- and Giemsa-stain: the cytoplasm appears blue. the nucleus is relatively large, eccentrically located, and red. the distinct, rod-shaped, red-staining kinetoplast (a specialized mitochondrial structure) contains extranuclear DNA arranged as catenated minicircles and maxicircles. 1. Amastigotes in a bone marrow specimen from a patient with visceral leishmaniasis. 2. Each amastigote has a nucleus and kinetoplast. 3. Visualization of the kinetoplast is essential in differentiating leishmaniasis from diseases such as histoplasmosis. Leishmaniasis (利什曼原蟲病) Anti-leishmanial antibodies and complement are deposited on the parasite surface. Promastigotes are phagocytosed by macrophages. Promastigotes convert within them to amastigotes. Amastigotes are released and infect other mononuclear phagocytes. Cell-mediated immune response (predominant Th1 response). Visceral Leishmaniasis (內臟型利什曼原蟲 病) Etiology: Typical: L. donovani (Indian subcontinent, northern and eastern China, Pakistan, Nepal, eastern Africa), L. infantum(Middle East, Mediterranean littoral, Balkans, central and southwestern Asia, northern and western China, North and sub-Saharan Africa), and L. chagasi (Latin America) Atypical: L. amazonensis (Latin America) or L. tropica (Middle East or Africa). Visceral Leishmaniasis (內臟型利什曼原蟲 病) The incubation period: usually 3 to 8 months. Symptoms/Signs: fever, weight loss, discoloration of skin (hands, feet, abdomen, or face), anemia, hepatosplenomegaly, leukopenia, and hypergammaglobulinemia. The condition is known as kala-azar (黑熱病). Question 1 Which infection does this patient have? What is the name of the hemoflagellate? Which is causing his infection? Answer 1 Due to the patient’s symptoms & signs, visceral leishmaniasis causes the patient’s infection. Question 2 Name the three species belonging to this complex. In which parts of the world are these species located? Answer 2 L. donovani: Indian subcontinent, northern and eastern China, Pakistan, Nepal, eastern Africa. L. infantum: Middle East, Mediterranean littoral, Balkans, central and southwestern Asia, northern and western China, North and sub-Saharan Africa. L. chagasi: Latin America Question 3 Which vectors are responsible for the transmission of this infection? Answer 3 Transmission is by Phlebotomus argentipes and other anthropophilic Phlebotomus spp. (白蛉). Question 4 List four forms of infection caused by this genus of hemoflagellates. How does this patient's infection differ from the other three? Answer 4 Cutaneous leishmaniasis: typically there is, first, a papule, which enlarges, becomes crusted, and then ulcerates. Ulcers have a diameter of about 2 cm and an indurated border. regional lymphadenopathy is common. patients usually have no fever, 1. Ulcerative skin lesions with raised outer borders on the arm of a patient with New World (American) cutaneous leishmaniasis acquired in Costa Rica. Diffuse cutaneous leishmaniasis: observed in Ethiopia, Venezuela, Brazil, and the Dominican Republic. the lesions are widespread and typically remain as macules or papules without ulceration. the mucous membranes may be involved, but not the viscera. lesions contain sparse lymphocytes, and there is cutaneous anergy to leishmanial antigens. Mucocutaneous leishmaniasis (espundia): caused by L. braziliensis and is especially prevalent in Brazil south of the Amazon. in patients with cutaneous lesions the likelihood of subsequent mucous membrane involvement is about 80%. more than 90% of patients with espundia have scars of previous cutaneous involvement. nasal lesions tend to destroy the cartilage of the septum and spread to the buccal mucosa, pharynx, and larynx. Question 5 How is the diagnosis of this infection made? Answer 5 Definitive diagnosis: amastigotes in tissue or the isolation of promastigotes in culture. Antileishmanial antibodies: high titer in immunocompetent patients with visceral leishmaniasis. ELISA (recombinant L. chagasi antigen rk39): highly sensitive and specific in detecting visceral leishmaniasis in immunocompetent persons. The leishmanin (Montenegro) skin test: negative results in patients with progressive visceral leishmaniasis. the result becomes positive in the majority of persons in whom infection spontaneously resolves and in those who have undergone successful chemotherapy. Differential diagnosis Acute stage: malaria, typhoid fever, typhus, acute Chagas' disease, schistosomiasis, miliary tuberculosis, or amebic liver abscess. Subacute or chronic stages: brucellosis, Salmonella bacteremia, histoplasmosis, infectious mononucleosis, hepatosplenic schistosomiasis, and splenomegaly due to chronic malaria. Question 6 What is the significance of the time of day (midnight) at which the patient was seen in the emergency department? Answer 6 The incubation period is usually in the range of 3 to 8 months. Question 7 What causes the enlargement of the liver and spleen? Answer 7 Large numbers of amastigote-infected mononuclear phagocytes in the liver and spleen result in progressive hypertrophy. The spleen: massively enlarged as splenic lymphoid follicles are replaced by parasitized mononuclear cells. The liver: marked increase in the number and size of Kupffer cells, many of which contain amastigotes. Question 8 What causes the anemia and leukopenia characteristic of this infection? Answer 8 Anemia: severe; normocytic and normochromic. hemolysis, marrow replacement with leishmaniainfected macrophages, hemorrhage, splenic sequestration of erythrocytes, hemodilution, and effects of cytokines such as TNF-alpha. Leukopenia: increased margination, splenic sequestration, or an autoimmune process. Question 9 Which complication may occur in this infection? Answer 9 Post-kala-azar dermal leishmaniasis: follows the treatment of visceral leishmaniasis in a subset of persons in Africa and India. the skin lesions vary from hyperpigmented macules to frank nodules. they are found on the face, trunk, extremities, oral mucous membranes, and occasionally, on the genitals. Question 10 How is this infection treated? Answer 10 References Harrison's Principles of Internal Medicine - 16th Ed. (2005) Internal Medicine, Stein - 5th Ed. (1998) Schlossberg: Current Therapy of Infectious Disease