* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
Survey
Document related concepts
Immune system wikipedia , lookup
DNA vaccination wikipedia , lookup
Adaptive immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Innate immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Transcript
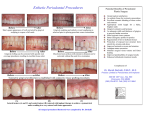
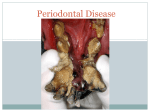
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA ANNEXURE II PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION 1 NAME OF THE CANDIDATE DR. VIJAYALAXMI M. KOKATNUR P.M.N.M. AND ADDRESS DENTAL COLLEGE AND HOSPITAL, BAGALKOT – 587101 KARNATAKA 2 NAME OF THE INSTITUTION P.M.N.M. DENTAL COLLEGE AND HOSPITAL, BAGALKOT – 587101 KARNATAKA 3 COURSE OF THE AND SUBJECT 4 STUDY M.D.S. (MASTER OF DENTAL SURGERY) PERIODONTICS DATE OF ADMISSION TO 31st MAY 2010 THE COURSE 5 TITLE OF THE TOPIC IN VIVO EXPRESSION OF TOLL-LIKE RECEPTOR PROTEIN RP105 IN CHRONIC AND AGGRESSIVE PERIODONTITIS BRIEF RESUME OF THE INTENDED WORK 6.1 Need for study Periodontal disease initiation and progression occurs as a consequence of the host immune inflammatory response to oral pathogens. Many of the microbial surface protein and lipopolysaccharide molecules are responsible for eliciting a host immune response, resulting in local tissue inflammation. The inflammatory infiltrate from the gingival tissue can initiate tissue and alveolar bone destruction through the activation of several pro-inflammatory cytokines, including interleukin-1β, tumor necrosis factor-α and interleukin-6.1 Host parasite reactions can be divided into innate immunity and adaptive immunity. Innate immunity is non-specific. It includes inflammatory response and do not involve immunologic response.6 The adaptive immune system is composed of highly specialized, systemic cells and processes that eliminate or prevent pathogenic challenges. The adaptive immune response provides the vertebrate immune system with the ability to recognize and remember specific pathogens, and to mount stronger attacks each time the pathogen is encountered. The recognition of pathogens is mediated by a set of germ-line-encoded receptors that are referred to as Pattern-recognition receptors. These receptors recognize conserved molecular patterns or PAMPs (pathogen-associated molecular patterns) shared by large groups of microorganisms. This recognition system is not only responsible for the first-line microbial clearance but also plays an instructive role in the adaptive immune response through the release of inflammatory cytokines and expression of co-stimulatory molecules by APCs (antigen presenting cells). The family of Toll-like receptors (TLRs) has been found to function as PatternRecognition receptors.3 Recently, 10 human Toll-like receptors (TLRs) have been identified, and the TLRs have been shown to play an essential role in response to bacterial cell surface components including lipopolysaccharide.4 Toll-like receptor 2 recognizes peptidoglycan, Toll-like receptor 3 recognizes viral double-stranded RNA, Toll-like receptor 4 recognizes lipopolysaccharide, Tolllike receptor 5 recognizes viral single-stranded RNA, and Toll-like receptor 9 recognizes bacterial DNA.5 RP105 is a B-cell surface molecule that has been recently assigned as CD180.8 They are associated with small molecules called MD-2 and MD-1,respectively ,to form heterodimers (TLR4/MD-2 and RP105/MD-1) and function as recognition/signaling molecules of lipopolysaccharide(LPS), a member component of Gram-negative bacteria. The B-cell activation pathway using RP105 is conserved in humans.6 Moreover, the anti-RP105 MoAb activates B-cell, leading to increase in cell size, expression of co Stimulatory molecule CD80 and DNA synthesis. Earlier reported studies have shown that RP105, a homolog whose expression mirrors that of TLR4 on antigen presenting cells, is a negative regulator of TLR4 signaling.6 Although the activation of proinflammatory responses through TLRs is critical for host defense, excessive inappropriate inflammation can itself be maladaptive. RP105 joins a growing group of molecules that can inhibit TLR signaling. Regulation of TLR expression provides one point of control, as does the complex phenomenon of endotoxin tolerance. Several direct, negative regulators of TLR signaling have been found, including MyD88s, IRAK-M, Etc. Among these,RP105 stands out for its apparent specificity for the inhibition of TLR4 signaling.7TLR4 may also stand out among the TLRs for its ability to signal in response to a variety of endogenous `danger signals’.9 The ability of TLR4 to recognize endogenous heat-shock proteins and extracellular matrix components `unmasked’ by tissue injury suggests the possibility that RP105 may well be of special importance in down modulation of the injurious inflammatory responses noted in the systemic inflammatory responses and in autoimmune disease. Hence, the purpose of the present study is to quantifying the expression of RP105 in gingival tissues of chronic and aggressive periodontitis patients using Immunohistochemistry technique. 6.2 Review of literature A study was done to show that human MD-1 is also associated with human RP105 and has an important role in cell surface expression of RP105 .The monoclonal antibody (MoAB) that recognizes human RP105 was also described. An immunohistochemical study was carried out where in the normal tonsil tissues were embedded in Tissue-Tek II OCT compound (Miles Inc, E1khart. IN), frozen in liquid nitrogen, and stored at -800C.Acetone-fixed cryostat sections of 4µm where incubated with the anti-RP105 MoAB MHR73. After washes, ENVISION+/HRP (DAKO Japan,, Inc, Tokyo, Japan)was added.RP105 was finally visualized with 3,3’diaminobenzidine.Histological studies showed that RP105 is expressed mainly on mature B cells in mantel zones. Germinal center cells are either dull or negative.RP105 is thus a novel B-cell marker that is preferentially expressed on mature B-cells. Moreover, pathway using RP105 is conserved in humans.6 RP105 was discovered originally in mouse B cells. In this quoted study ,an antibody raised against the surface of mature B cells was found to drive B cell proliferation and protection from subsequent radiation - or dexamethasone induced apoptosis. Cloning of human and mouse RP105 revealed a type 1 transmembrane protein structurally similar to TLRs, with an extracellular- rich repeat domain and the pattern of juxtamembrane cystein residues conserved among the TLRs. The analysis of mice homozygous for the null mutation in the RP105 gene revealed impaired proliferative and humeral immune responses of RP105deficient B cells to LPS. Using originally LPS-unresponsive Ba/F3 cells expressing exogenous TLR4 and RP105 in LPS – induced nuclear factor kB activation. These data suggest the existence of the TLR4-RP105 signaling module in the LPS- induced B cell activation.2 In a study, a negative regulation of Toll-like receptor 4 signaling by the Toll-like receptor homolog RP105 was shown in Human Embryonic Kidney cells (HEK 293 cells).The effects of RP105-MD-1 expression on LPS- driven TLR4 signaling was examined. Notably, RP105 expression inhibited TLR4-driven IL-8 production by HEK 293 cells in a dose–dependent manner. Furthermore, RP105-mediated inhibition of LPS-driven IL-8 production was associated with inhibition of LPS-driven transactivation factor NF-kB, suggesting that modulation of IL-8 production by RP105 was `upstream’ of NF-kB activation. Later the specificity of RP105mediated suppression of proinflammatory signaling was examined which showed that RP105 did not inhibit IL-1 or TLR2-driven IL-8 production, indeed, RP105 over expression led to variable augmentation of TLR2-mediated IL-8 production in some experiments. Thus, RP105- mediated suppression shows specificity among the TLR-IL-1 receptor family.7 In a study, the gene expression profile in human periodontal ligament cells (HPDLCs) in response to TLR4 ligands, LPS treatment was analyzed by microarray analysis. It was observed that LPS treatment could induce TLR4 activation, increase the gene expression of colony stimulation factor 2(CSF2), and decrease the gene expression of RP105/LY64 in vitro .These results suggests the possible involvement of RP105 in TLR4 mediated periodontal inflammation responses. A study was conducted to explore the in vivo expression of TLR-2, TLR-4, CSF2 and LY64 (Ly64 and LY64 are genes related to RP105) in chronic periodontitis patients, who are systemically healthy and non-smokers. RT-PCR was performed to determine the mRNA expression levels ofTLR2, TLR4, CSF2 and RP105 in gingival samples. In this study the gene expression levels of CSF2 increased whereas LY64 mRNA expression decreased. Further studies should be conducted to ascertain whether inflammation was the only reason for the decrease of LY64 expression in chronic periodontitis patients.1 A study was carried out to see the altered expression of TLR homolog RP105 on monocytes hypersensitivity to LPS in patients with primary biliary cirrhosis, wherein invitro responses to TLR ligand, LPS, using peripheral blood mononuclear cells and monocytes from 25 patients with PBC, 10 patients with chronic viral hepatitis(CVH), and 20 healthy individuals was investigated. After stimulation with LPS, the results significantly showed higher amounts of IL1β, IL-6, and IL-8 production in PBC patients. Through the TLR signaling pathway, activation of NF-kB and expression of MyD88 mRNA were significantly increased in PBC patients and the level of TLR4 expression was significantly increased on PBC monocytes as compared with CVH patients and controls. Of significance, the surface expression of RP105, which has recently been shown to be involved in negative regulation of TLR4 signaling, on PBC monocytes was significantly decreased in comparison with CVH patients and controls.11 6.3 Aims & Objective 1. To quantify the expression of RP105 in gingival tissues of subjects with healthy periodontium 2. To compare the expression levels of RP105 in gingival tissues of healthy controls and those with aggressive periodontitis. 3. To correlate the expression levels of RP105 with severity of periodontal diseases. MATERIALS AND METHODS 7.1 Source of data Sixty five patients will be selected from the outpatient Department of Periodontics, PMNM Dental College and Hospital, Bagalkot. 7.2 Methods of collection of data The study will be carried out on 15 subjects with healthy periodontium, 25 patients with chronic periodontitis and 25 patients with aggressive periodontitis. Gingival tissue samples from the selected subjects will be obtained for the analysis of RP105 expression. Samples are grouped as follows: Group I : 15 gingival tissue samples from subjects with healthy periodontium Group II: 25gingival tissue samples from patients with chronic periodontitis Group III: 25 gingival tissue samples from patients with aggressive periodontitis Gingival tissue specimens for group I will be obtained during tooth extraction due to orthodontic treatment purpose and during third molar extraction. For groups II and III, specimens will be obtained during periodontal surgery. Specimens obtained will be placed in buffer solution and will be sent to laboratory for quantification of RP105 by using immunohistochemistry method. INCLUSION CRITERIA 1) Group I: Healthy subjects showing absence of clinical manifestations of periodontal disease, at least 15 teeth and present no history of periodontal treatment for the past six months. 2) Group II: Chronic periodontitis patients with periodontal pockets >5mm. 3) Group III: Aggressive periodontitis patients. All the patients should be systemically healthy and none should have received periodontal treatment for at least 6 months prior to sampling and recording. EXCLUSION CRITERIA Smokers Systemic diseases like diabetes mellitus, hepatitis, and HIV infection known to influence the periodontal disease. Diseases of oral hard and soft tissue except caries and periodontitis. Chronic usage of antibiotics and analgesics within three months prior to study. Pregnant and lactating female. All potential participants were explained the need and design of the study. Only those subjects who gave consent for the study were included after obtaining an informed consent. CLINICAL EXAMINATION TO ASSESS THE PERIODONTAL CONDITION Gingival index(Loe & sillness) Probing pocket depths(using William’s graduated periodontal probe) Clinical attachment loss LABORATORY INVESTIGATIONS Gingival tissue specimens will be sent to the laboratory for quantification of RP105 using immunohistochemistry. Monoclonal anti-human RP105 antibody kit will be procured from Biolegend, USA STATISTICAL ANALYSIS The results will be statistically analyzed using the following methods. One way ANOVA- It is used to compare values among three groups. Mann-Whitney test or t-test - It is used to compare values among two groups. 7.3 DOES THE STUDY REQUIRE ANY INVESTIGATIONS OR INTERVENTIONS TO BE CONDUCTED IN THE PATIENTS? Yes. Gingival tissue samples have to be obtained from the patients. 7.4 HAS ETHICAL CLEARANCE BEEN OBTAINED FROM THE INSTITUTION? Yes. The copy of ethical clearance certificate is attached. REFERENCES 1. D-L Liu, Y Sun, M-Z Zhang, Q-M Guo, R Shu. In vivo expression of Toll-like receptor 2, Toll-like receptor 4, CSF2 and LY64 IN Chinese chronic periodontitis patients. Oral Diseases, 2010 (16): 343-50. 2. Hirotaka Ogata, I- hsin Su, Kensuke Miyake, Yoshinori Nagai, Sachiko Akashi, Alexander Taraskhovsky, et al. The Toll-like receptor protein RP105 regulates lipopolysaccharide signaling in B cells. J Exp Med, 2000 Jul 3; 192(1)23-30. 3. Kirkwood KL, Cirelli J A, Rogers JE, Giannobile WV. Novel host response therapeutic approaches to treat periodontal diseases. Periodontol 2000 2007; (43) 294315. 4. Medzhitov R, Preston- Hurlburt P, Janeway CA Jr. A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature 1997 ;( 388) 394-7. 5. Mahanonda R, Pichayangkul S. Toll-like receptors and their role in periodontal health and disease. Periodontol 2000 2007; (43) 41-55. 6. Miura Y, Shimazu R, Miyake K, Sachiko Akashi, Hirakata Ogata, Masao Kimoto. RP105 is associated with MD-1 and transmits an activation signal in human B cells. Blood 1998 ;( 92) 2815-22. 7. Senad Divanovic, Rajat Madan, Christopher L Karp, Aurelian Trompette, Sowsan F Atabani, Robert W Finberg, et al. Negative regulation of Toll-like receptor 4 signaling by the Toll-like receptor homologue RP105. Nature Immunol 2005 April 26; 6(6):571-4. 8. Nagai Y, Shimazu R, Ogata H, Akashi S, Sudo K, et al. Requirement for MD-1 in cell surface expression of RP105/CD180 and B-cell responsiveness to lipopolysaccharide. Blood 2002; 99(5):1699-170. 9. Takeda K, Kaisho T & Akira S. Toll-like receptors. Annu. Rev Immunol, (21)335-376. 10. Nagai Y, Kobayashi T, Motoi Y, Ishiguro, et al. The radiprotective 105/MD-1 complex links TLR2 and TLR4/MD-2 in antibody response to microbial membranes. J Immunol. (174):7043-49. 11.Yutaka Honda, Satoshi Yamagiwa, Yasunobu Matsuda, Masaaki Takamura, Tamaki Ichida, Yutaka Aoyagi. Altered expression of TLR homolog RP105 on monocytes hypersensitive to LPS in patients with primary bilary cirrhosis. J Hepatol, 2010 June 10; 47(3):404-11