* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Infectious Diseases and Obstetrics: Then and Now
Survey
Document related concepts
Neglected tropical diseases wikipedia , lookup
Common cold wikipedia , lookup
Germ theory of disease wikipedia , lookup
Urinary tract infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis C wikipedia , lookup
Globalization and disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Infection control wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Transcript
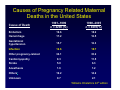
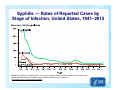
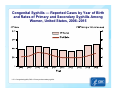
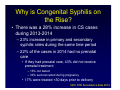
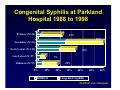
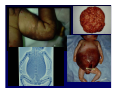
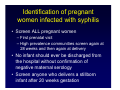
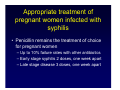
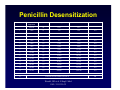
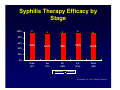
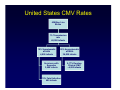
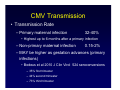
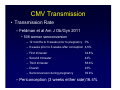
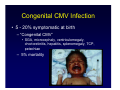
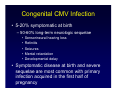
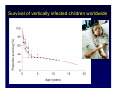
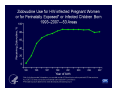
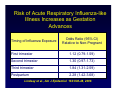
Infectious Diseases and Obstetrics: Then and Now How Microbes have Shaped Obstetrics Jeanne S. Sheffield, MD Maternal-Fetal Medicine Johns Hopkins Medicine I have no financial disclosures Infectious Diseases in Obstetrics • The single most common medical condition encountered by the obstetrician • The obligatory immunologic changes that allow for diminished inflammatory response and fetal tolerance increases many infection related complications Data from Berg 2010 Causes of Pregnancy Related Maternal Deaths in the United States 1991–1999 n = 4200 (%) 1998–2005 n = 4693(%) Embolism 19.6 10.2 Hemorrhage 17.2 12.5 Gestational hypertension 15.7 12.3 Infection 12.6 10.7 Other pregnancy-related 34.1 33.2 Cardiomyopathy 8.3 11.5 Stroke 5.0 6.3 Anesthesia 1.6 1.2 Otherse 19.2 14.2 Unknown 0.7 2.1 Cause of Death Williams Obstetrics 24th edition Ignaz Semmelweis 1818-1865 • Hungarian physician considered the “Saviour of Mothers” • Handwashing with chlorinated lime solutions – Decreased fatal puerperal fever from 10% to 1-2% • The Etiology, Concept and Prophylaxis of Childbed Fever 1861 Ignaz Semmelweis 1818-1865 • Ridiculed and dismissed from the Vienna hospital where he practiced – 1865 committed to an asylum and died 15 days later • His work however has saved millions of women over the last 2 centuries Louis Pasteur 1822-1895 • French Chemist and microbiologist • Developed the germ theory of disease and vindicated Semmelweis • Father of microbiology and developed some of the earliest vaccines e.g.anthrax and chicken cholera Intrauterine Infection and Obstetric Outcomes Cause or Consequence? • Bradford Hill Criteria – Biologic sense – Specificity of the association – Temporal relationship – Consistency of the association – Strength of the association – Dose-response curve – Human experimentation History of the Preterm Birth and Infection Association • It has been known for over a century that certain infections are associated with stillbirth and PTL • 1943 Zahal et al – Injected Salmonella and Shigella endotoxin into pregnant animals, resulting in abortion and PTL • Multiple animal studies since that time have shown similar findings – 1990 Dombroski et al Ascending uterine infection model • Focus in the last century has been on the specific organisms • There are so many organisms that have shaped obstetrical practice. To name just a few…. – – – – – – – – Syphilis Bacterial vaginosis Group B streptococcus Malaria HIV Influenza Tuberculosis Viral and parasitic infections The “TORCH” infections “He who knows Syphilis, knows Medicine” Sir William Osler(1849-1919) Ricard Tennant Cooper (1912) Wellcome Library, London The History of Syphilis • First reported as a venereal disease in the 15th century in Italy – Spanish exploration and colonization of the American continent – There is evidence of treponemal infections among natives in the pre-Columbian period • Rapidly reached epidemic proportions in the early 16th century “The Great Pox”, spreading to all parts of the globe • 19th century 10-20% of the population thought to be infected Radolf and Lekehart Pathogenic Treponema The History of Syphilis • Syphilis initially was devastating disease • First World War an arsenic compound (salvarsan) was used for treatment and for the first time saw a decrease in prevalence • The wonder drug penicillin was discovered in the 1940s • We have intermittent increases over the last few decades associated often with drug issues but overall a significant decrease. • Prenatal screening has played a significant part in decreasing vertical and heterosexual transmission Syphilis — Rates of Reported Cases by Stage of Infection, United States, 1941–2015 NOTE: Data collection for syphilis began in 1941; however, syphilis became nationally notifiable in 1944. Refer to the National Notifiable Disease Surveillance System (NNDSS) website for more information: https://wwwn.cdc.gov/nndss/conditions/syphilis/. Primary and Secondary Syphilis — Rates of Reported Cases by Sex and Male-to-Female Rate Ratios, United States, 1990–2015 Primary and Secondary Syphilis — Rates of Reported Cases Among Women Aged 15–44 Years by Age Group, United States, 2006–2015 Congenital Syphilis — Reported Cases by Year of Birth and Rates of Primary and Secondary Syphilis Among Women, United States, 2006–2015 * CS = Congenital syphilis; P&S = Primary and secondary syphilis. Why is Congenital Syphilis on the Rise? • There was a 28% increase in CS cases during 2013-2014 – 23% increase in primary and secondary syphilis rates during the same time period – 22% of the cases in 2014 had no prenatal care • If they had prenatal care, 43% did not receive prenatal treatment – 16% not tested – 39% seroconverted during pregnancy • 17% were treated <30 days prior to delivery CDC STD Surveillance data 2014 Congenital Syphilis at Parkland Hospital 1988 to 1998 Primary (N=26) 23% 60% Secondary (N=53) Early Latent (N=145) 36% Late Latent (N=27) 7% 20% Unknown (N=97) 0% 10% Stillbirth 20% 30% 40% 50% 60% Congenital Syphilis Sheffield and colleagues The only way to prevent congenital syphilis is to prevent or at least treat maternal syphilis Identification of pregnant women infected with syphilis • Screen ALL pregnant women – First prenatal visit – High prevalence communities screen again at 28 weeks and then again at delivery • No infant should ever be discharged from the hospital without confirmation of negative maternal serology • Screen anyone who delivers a stillborn infant after 20 weeks gestation Appropriate treatment of pregnant women infected with syphilis • Penicillin remains the treatment of choice for pregnant women – Up to 10% failure rates with other antibiotics – Early stage syphilis 2 doses, one week apart – Late stage disease 3 doses, one week apart Penicillin Desensitization Dose Penicillin V Suspension Amount Penicillin V Suspension Cumulative Dose Route Units/mL mL Units Units 1 1,000 0.1 100 100 P.O. 2 1,000 0.2 200 300 P.O. 3 1,000 0.4 400 700 P.O. 4 1,000 0.8 800 1,500 P.O. 5 1,000 1.6 1,600 3,100 P.O. 6 1,000 3.2 3,200 6,300 P.O. 7 1,000 6.4 6,400 12,700 P.O. 8 10,000 1.2 12,000 24,700 P.O. 9 10,000 2.4 24,000 48,700 P.O. 10 10,000 4.8 48,000 96,700 P.O. 11 80,000 1.0 80,000 176,700 P.O. 12 80,000 2.0 160,000 336,700 P.O. 13 80,000 4.0 320,000 656,700 P.O. 14 80,000 8.0 640,000 1,296,700 P.O. Wait 30 minutes 15 2,400,000 Units Benzathine Penicillin G Wendel, GD et al. N Engl J Med 1985: 312:1229-32 I.M. Syphilis Therapy Efficacy by Stage 100% 0 4 2 0 6 100% 94.7% 98% 100% 98.2% Prim (27) Sec (75) EL (102) LL (136) Total (340) 80% 60% 40% 20% 0% Success Failure Alexander JA, et al. Obstet Gynecol “He who knows Syphilis, knows Medicine” Sir William Osler(1849-1919) Ricard Tennant Cooper (1912) Wellcome Library, London Cytomegalovirus • Most common congenital viral infection in the United States – 0.2-2.5% incidence of congenital infection • Herpesvirus family – Ubiquitous dsDNA virus – Latent phase with sporadic reactivation • Preexisting maternal CMV decreases but does not eliminate fetal infection (partial protection) Cytomegalovirus • Overall 58% of women aged 15-44 years are seropositive (US based study) – Up to 85% of women from lower socioeconomic backgrounds are seropositive. – 50-60% of women from higher income groups are seropositive. • Transmission may occur to a fetus of an immune mother secondary to reactivation or from re-infection with a new serotype. – Non-primary infections more common in low SEC compared to high SEC (3.6 vs. 1.7%) United States CMV Rates 4 Million Live Births 1% Transmission rate 40,000 infants 10% Symptomatic at birth 4,000 infants 90% Asymptomatic at Birth 36,000 infants Survivors with Sequelae 3,600 infants 10% Fatal Infection 400 infants 5-17% Develop Clinical CMV ~4,000 infants CMV Transmission • Transmission Route – Horizontal : saliva, urine and blood, STD – Vertical • Transplacental (infects the placenta) 95% – Placental cytotrophoblasts permissive to replication • Peripartum 5% – cervical shedding – breast milk • Ascending antepartum – Amniocentesis is not a risk factor Rare CMV Transmission • Transmission Rate – Primary maternal infection 32-40% • Highest up to 6 months after a primary infection – Non-primary maternal infection 0.15-2% – MAY be higher as gestation advances (primary infections) • Bodeus et al 2010 J Clin Virol 524 seroconversions – 35% first trimester – 44% second trimester – 73% third trimester CMV Transmission • Transmission Rate – Feldman et al Am J Ob/Gyn 2011 • 508 women seroconversion – 12 months to 8 weeks prior to pregnancy 0% – 8 weeks prior to 6 weeks after conception 4.6% – First trimester 34.8% – Second trimester 42% – Third trimester 58.6% – Overall 23% – Seroconversion during pregnancy 39.9% – Periconception (3 weeks either side)16.4% Epidemiology • Fetal Transmission – First and early second trimester exposure often associated with the most severe sequelae i.e. microcephaly – Late pregnancy exposure associated with functional sequelae i.e. thrombocytopenia and hepatitis Congenital CMV Infection • 5 - 20% symptomatic at birth – “Congenital CMV” • SGA, microcephaly, ventriculomegaly, chorioretinitis, hepatitis, splenomegaly, TCP, petechiae – 5% mortality Congenital CMV Infection • 5-20% symptomatic at birth – 50-60% long-term neurologic sequelae • • • • • Sensorineural hearing loss Retinitis Seizures Mental retardation Developmental delay • Symptomatic disease at birth and severe sequelae are most common with primary infection acquired in the first half of pregnancy Maternal screening not recommended • No vaccine available to prevent infection in seronegative women • Hard to tell timing, primary vs. non-primary so counseling difficult • No evidence that antiviral therapy prevents or mitigates disease in the fetus • Fetal infection can be detected but no way to determine sequelae risk Treatment and Prevention • No antepartum antiviral therapy recommended for the immunocompetent woman – No good data that is improves maternal outcome or decreases transmission to the fetus • CMV hyperimmune globulin may lower risk of congenital disease if given antepartum (Nigro 2005) – 157 women diagnosed with primary CMV • Therapy offered to women with evidence of AF infection by PCR or culture – high dose IVIg multiple doses if “needed” • If no amniocentesis, stratified into prevention group and got monthly lower dose IVIg Treatment and Prevention • CMV hyperimmune globulin may lower risk of congenital disease if given antepartum (Nigro 2005) – – – – – Therapy group, 1 of 31 women had infected infant No intervention group, 7 of 14 women had infected infant Prevention group, 6 of 37 women had infected infant No adverse events Subsequent case control of 64 additional kids noted a decrease in CMV sequelae in infants born to mothers receiving IVIg – CRAPPY study design – Network study in process Treatment Trials • Hyperimmunoglobulin – 3 prospective observational trials • IG given to pregnant women with primary CMV decreased transmission and disease severity – Congenital Human CMV Infection Prevention (CHIP) trial • 124 pregnant women 5-26 weeks gestation with recent primary CMV randomized to hyperimmunoglobulin or placebo every 4 weeks until 36 weeks or detection CMV in AF – Congenital infection the same (30 vs 44%) – Symptoms at bith also similar (30 vs 24%) – More complications in hyperimmunoglobulin group HIV and AIDS • 1970s reports of a “wasting disease” in Africa • 1981 the first cases were reported in California and New York among the MSM and then the injection drug use population • 1984 the HIV was identified (HTLV-III or LAV) • 1985 HIV test for blood supply screening Survival of vertically infected children worldwide Perinatal Transmission • Antiretroviral Therapy • 1994 076 Protocol – 24% to 8 % transmission rate – All CD4 counts > 200 – No prior therapy Antepartum Zidovudine 300 mg BID or 200 mg TID Intrapartum Zidovudine 2 mg/kg loading 1mg/kg/hr until delivery Neonatal Zidovudine 2 mg/kg every 6 hours for 6 weeks Malaria and Obstetrics • Global estimated malaria case incidence rate fell by 30% between 2000 and 2013 and mortality rates fell by 47% • 198 million cases (124-283 million) worldwide • Malaria remains an important direct cause of maternal and fetal complications – – – – – PTL Miscarriage Stillbirth and neonatal death Low birthweight Congenital infection Malaria and Obstetrics • Pregnant women are less likely to clear the parasites, leading to higher mortality and morbidity rates. – Pregnant women are 3 times more likely to develop severe disease • Malaria parasites sequester and replicate in the placenta Malaria and Obstetrics • Intermittent preventative treatment in pregnancy (IPTp) has been adopted in 34 of the 45 countries with ongoing transmission in Africa (sulfadoxinepyrimethamine at each of 4 antenatal visits) – 25% of pregnant women have acute infection in pregnancy • Uncomplicated malaria treatment in pregnancy – Chloroquine as per non-pregnancy guidelines • Can use hydroxychloroquine – If chloroquine-resistance, use mefloquine or a combination of quinine/clindamycin • Can also use atovaquone-proguanil or artemetherlumefantrine Influenza Virology – Type A • Subtyped based on surface glycoproteins – 16 hemagglutinin (HA) and 9 neuraminidase (NA) • Infects multiple other species and can jump between them – Birds, pigs, horses, seals, dogs – Host preference Birds reservoir for new subtypes Risk of Acute Respiratory Influenza-like Illness Increases as Gestation Advances Timing of Influenza Exposure Odds Ratio (95% CI) Relative to Non-Pregnant First trimester 1.12 (0.79-1.59) Second trimester 1.30 (0.97-1.73) Third trimester 1.84 (1.31-2.59) Postpartum 2.28 (1.42-3.68) Lindsay et al., Am J Epidemiol 163:838-48, 2006 Influenza and Pregnancy • Well established increase in morbidity and mortality with both seasonal and pandemic influenza strains • Vaccination is an effective was to decrease both maternal and neonatal morbidity – Immunization studies performed both in the United States and internationally • 1/3 of the world’s population infected with TB – 2011 9 million people developed tuberculosis – 1.4 million TB-related deaths TB and Pregnancy • Fetal effects if the mother has untreated TB – Low birth weight and congenital or neonatal TB – Significant issue worldwide though rare here in the United States • Much of the worldwide focus on decreasing maternal and neonatal mortality has focused on tuberculosis, helminths and malaria – These diseases are affecting global health policy with regards to the care of the pregnant woman Human Genomics and Infectious Diseases One of the greatest feats in medical history The mapping was completed in April, 2003 The Human Microbiome • As humans have evolved, so have the millions of microorganisms that populate the human body – Digestive and metabolic functions • 40% host’s energy intake – Development and adaptation of the host immune response • The human as a “superorganism”, combining our genome with the microbiome – In the future, this thinking will help guide therapeutic strategies, not just targeting the individual but also the microbiome Braundmeier and colleagues, 2015 The Microbiome and Pregnancy A New Paridigm • We are now characterizing the microbiome and how it changes in response to pregnancy (Human Microbiome and the MetaHIT Projects) – The vaginal and cervical microbiome shift during pregnancy • Reduction in microbial richness and diversity with a predominance of Lactobacillus species – Improve immune system function for protection of the fetus from the maternal immune response and to protect against pathogen invasion – The gut microbiome shifts, resulting in an impact on host metabolism Aagaard and colleagues 2012 The Microbiome and Pregnancy A New Paridigm • Placenta and amniotic fluid microbiomes, both in healthy and abnormal pregnancies – Bacterial species colonizing the placenta are involved in nutrition transport to the fetus e.g. metabolizes cofactors and vitamins • These microbes are transmitted to the fetus during gestation to populate the “naïve” fetal tissues – Affected by mode of delivery and breastfeeding – Aid in metabolism and immune protection at birth Braundmeier and colleagues, 2015 The Microbiome and Pregnancy Pathologic Implications • Bacterial vaginosis • Preterm birth with and without BV – Altered vaginal microbiome with racial differences • Failure of IVF • Early pregnancy loss • Pelvic inflammatory diseases and STDs This leaves the field wide open for new therapeutic approaches in obstetrics Braundmeier and colleagues, 2015