* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download NURSING PROCESS FOCUS Clients Receiving Conventional
Survey
Document related concepts
Psychedelic therapy wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Drug design wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Transcript
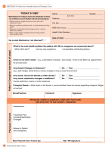
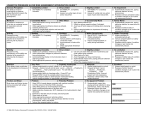
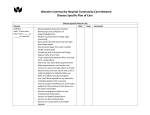
ADAMMC17_0131756656 2/20/07 9:59 PM Page 216 Team B 107:PEQY046:phada2:ch17: 216 Unit 3 The Nervous System NURSING PROCESS FOCUS Clients Receiving Conventional Antipsychotic Therapy Assessment Potential Nursing Diagnoses Prior to administration: Obtain a complete health history (medical and psychological) including allergies, drug history, and possible drug interactions. Obtain baseline lab studies (electrolytes, CBC, BUN, creatinine, WBC, liver enzymes, and drug screens). Assess for hallucinations, level of consciousness, and mental status. Assess client support system(s). ■ ■ ■ ■ ■ ■ ■ ■ ■ Therapeutic Regimen Management, Ineffective, related to noncompliance with medication regimen, presence of side effects, and need for long-term medication use Anxiety, related to symptoms of psychosis Injury, Risk for, related to side effects of medication Noncompliance, related to length of time before medication reaches therapeutic levels, desire to use alcohol or illegal drugs Knowledge, Deficient, related to unfamiliarity with medications and their effects Planning: Client Goals and Expected Outcomes The client will: Report a reduction of psychotic symptoms, including delusions, paranoia, irrational behavior, hallucinations. Demonstrate an understanding of the drug’s action by accurately describing drug side effects and precautions. Immediately report side effects or adverse reactions. Adhere to recommended treatment regimen. ■ ■ ■ ■ Implementation Interventions and (Rationales) ■ Monitor for decrease of psychotic symptoms. (If client continues to exhibit symptoms of psychosis, the drug or dose may not be effective.) Client Education/Discharge Planning Instruct client and caregiver to: Notice increases or decreases of symptoms of psychosis, including hallucinations, abnormal sleep patterns, social withdrawal, delusions, or paranoia. Contact physician if symptoms do not decrease over a 6-week period. ■ ■ ■ Monitor for side effects. (Problems with side effects may cause a decrease in compliance.) Instruct client and caregiver: About problems with drowsiness, dizziness, lethargy, headaches, blurred vision, skin rash, sweating, nausea/vomiting, lack of appetite, diarrhea, menstrual irregularities, depression, and blood pressure problems. That impotence, gynecomastia, amenorrhea, and enuresis may occur. ■ ■ ■ Monitor for anticholinergic side effects such as orthostatic hypotension, constipation, anorexia, GU problems, respiratory changes, and visual disturbances. (These side effects may need to be treated so the client can continue with the medication.) Instruct client to: Avoid abrupt changes in position. Avoid driving or performing hazardous activities until effects of the drug are known. Report vision changes. Increase dietary fiber, fluids, and exercise to prevent constipation. Relieve symptoms of dry mouth with sugar-free hard candy or gum and frequent drinks of water. Notify physician immediately if urinary retention occurs. ■ ■ ■ ■ ■ ■ ■ ■ ■ Monitor for EPS and NMS. (Presence of EPS may be sufficient reason for the client to discontinue the antipsychotic. NMS is life threatening and must be reported and treated immediately.) Monitor for alcohol/illegal drug use. (Used concurrently, these cause an increased CNS depressant effect.) Monitor caffeine use. (Use of caffeine-containing substances negates the effects of antipsychotics.) Instruct client and caregiver to: Recognize tardive dyskinesia, dystonia, akathisia, and pseudoparkinsonism. Immediately seek treatment for elevated temperature, unstable blood pressure, profuse sweating, dyspnea, muscle rigidity, or incontinence. ■ ■ ■ Instruct client to avoid alcohol and illegal drug use. Refer client to community support groups such as AA or NA as appropriate. Instruct client or caregiver about: Common caffeine-containing products. Acceptable substitutes, such as decaffeinated coffee and tea, and caffeinefree colas. ■ ■ ■ Monitor for cardiovascular changes, including hypotension, tachycardia, and ECG changes. (Haloperidol has fewer cardiotoxic effects than other antipsychotics, and may be preferred for clients with existing CV problems.) ■ Instruct client and caregiver that dizziness and falls, especially with sudden position changes, may indicate cardiovascular changes. Teach safety measures. ADAMMC17_0131756656 2/10/07 9:10 PM Page 217 Team B 107:PEQY046:phada2:ch17: Chapter 17 Drugs for Psychoses 217 NURSING PROCESS FOCUS Clients Receiving Conventional Antipsychotic Therapy (Continued) Implementation Interventions and (Rationales) ■ ■ Client Education/Discharge Planning Monitor for smoking. (Heavy smoking may decrease metabolism of haloperidol, leading to decreased efficacy.) Monitor elderly clients closely. (Elderly clients may need lower doses and a more gradual dosage increase. Elderly women are at greater risk for developing tardive dyskinesia.) ■ ■ ■ ■ ■ ■ ■ Monitor lab results, including RBC and WBC counts, and drug levels. (Use of some medications may cause changes in blood counts. Some medications can cause toxicity.) Monitor for use of medication. (All antipsychotics must be taken as ordered for therapeutic results to occur.) Monitor for seizures. (This drug may lower the seizure threshold.) Monitor client’s environment. (The drug may cause the client to perceive a brownish discoloration of objects or photophobia. It may also interfere with the ability to regulate body temperature.) ■ ■ ■ Instruct client to stop or decrease smoking. Refer client to smoking cessation programs, if indicated. Instruct caregiver to observe for and immediately report unusual reactions such as confusion, depression, and hallucinations, and for symptoms of tardive dyskinesia. Instruct elderly clients or caregivers how to counteract anticholinergic effects of medication while taking into account any other existing medical problems. Instruct client and caregiver to keep appointments for laboratory testing. Instruct client and caregiver to take medication as prescribed, even if no therapeutic benefits are felt, because it may take several months for full therapeutic benefits to occur. Instruct client and caregiver that seizures may occur and review appropriate safety precautions. Instruct client and caregiver to: Wear dark glasses to avoid discomfort from photophobia. Avoid temperature extremes. Be aware that perception of brownish discoloration of objects may appear, but it is not harmful. ■ ■ ■ Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that client goals and expected goals have been met (see “Planning”). The client and famly report a decrease in symptoms of psychosis including delusions, paranoia, and irrational behavior. The client demonstrates an understanding of the drug’s action by accurately describing side effects and precautions. The client immediately reports adverse reactions. The client adheres to the recommended treatment regimen. ■ ■ ■ ■ See Tables 17.1 and 17.3 for lists of drugs to which these nursing actions apply. extrapyramidal signs. Concurrent therapy with other CNS depressants must be carefully monitored, because of the potential additive effects. Drugs in the nonphenothiazine class have the same therapeutic effects and efficacy as the phenothiazines. They are also believed to act by the same mechanism as the phenothiazines, that is, by blocking postsynaptic D2 dopamine receptors. As a class, they offer no significant advantages over the phenothiazines in the treatment of schizophrenia. NURSING CONSIDERATIONS The role of the nurse in conventional nonphenothiazine therapy involves careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Because nonphenothiazines can also interact with many drugs, assess the client’s drug use history, including current and past medications, to establish any previous allergic reactions or adverse effects from these medications. Assess elderly clients more carefully than younger clients for unusual adverse reactions such as confusion, depression, and hallucinations that are drug induced. Perform a complete baseline assessment, including physical assessment, mental status (orientation, affect, cognition), vital signs, lab studies (CBC, liver and renal function tests), preexisting medical conditions (especially cardiac, kidney, and liver function), and vision screening. Assess the available support system, because many psychiatric clients are unable to self-manage their drug regimen. Contraindications for this class of drugs include Parkinson’s disease, CNS depression, alcoholism, seizure disorders, and age younger than 3 years. Inform the client and caregivers that sedation is a less severe side effect than with phenothiazines, but there is a greater incidence of EPS with nonphenothiazine antipsychotics. A possible life-threatening adverse effect of antipsychotic drugs is NMS. Because of the anticholinergic side effects of these drugs, monitor for dry mouth, urinary retention, constipation, and hypotension with resultant tachycardia. Compliance