* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pericardial Effusion
Survey
Document related concepts
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Transcript
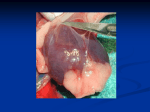
Infective Endocarditis Acute Bacterial Endocarditis (ABE) Etiology ● ● ● ● ● ● Staphylococcus aureus—most common. Group A, B, C, and G streptococci. Haemophilus influenzae. Streptococcus pneumoniae. Neisseria gonorrhea. Enterococcus. Subacute Bacterial Endocarditis (SBE) Etiology ● Streptococcus viridans and S. bovis—most common. ● Streptococcus fecalis and S. faecium (i.e., enterococci). ● S. aureus. HACEK organisms (Haemophilus, Actinobacillus, Cardio-bacterium, Eikenella, Kingella).ENDOCARDITIS WITH IV DRUG ABUSE ● S. aureus—frequently methicillin-resistant S. aureus. ● Pseudomonas aeruginosa and P. cepacia. ● Enterococcus. ● Candida fungal species. Prosthetic Valve Endocarditis Etiology ● S. aureus. ● Staphylococcus epidermidis. ● Candida and Aspergillus fungal species. ● S. viridans. ● Enterococcus. HACEK organisms (Haemophilus, Actinobacillus, Cardio-bacterium, Eikenella, Kingella).ENDOCARDITIS WITH IV DRUG ABUSE ● S. aureus—frequently methicillin-resistant S. aureus. ● Pseudomonas aeruginosa and P. cepacia. ● Enterococcus. ● Candida fungal species. Pathology ● Infection with inflammation affecting valvular endocardium and occasionally mural endocardium. May lead to vegetations, valve destruction, systemic embolization. ● Can be classfied into ABE, SBE, endocarditis with IV drug abuse, and early (within 60 days of implantation) or late (60 days or longer after implantation) prosthetic valve endocarditis. ABE is caused by virulent organisms and has an aggressive course. SBE usually occurs in patients with preexisting VHD and has a slower, more indolent course. Endocarditis in IV drug abusers has predilection for tricuspid valve. Risk Factors ● Prosthetic cardiac valves. ● Congenital cardiac anomalies. ● Previous IE. ● Rheumatic heart disease. ● ● ● ● ● Any VHD, including MVP when with MR. Hypertrophic cardiomyopathy. Indwelling intravascular devices. Dental or surgical procedures that cause transient bacteremia. IV drug abuse. Clinical Features ● Classic triad—fever, heart murmur, positive blood culture; however, all of these do not have to be present. History ● ● ● ● ● ● ● ● ● ● Fever. Anorexia and weight loss. Night sweats. Fatigue. Arthralgias, myalgias. Cephalgia. Delirium. Muscle weakness, paralysis. Cold painful extremity with embolism. Gross hematuria. Physical Exam Findings ● Murmurs—mostly mitral and aortic involvement, but tricuspid lesions seen in IV drug abuse. ● Fever (ABE—102° to 105° F; SBE—99° to 100° F). ● Conjunctival hemorrhage. ● Petechiae (particularly oropharynx, lower extremity). ● Splinter hemorrhages (on nail beds). ● Osler nodes (subcutaneous nodules of fingers). ● Janeway lesions (small non-painful hemorrhagic patches on palms, soles of feet). ● Roth spots (oval white areas surrounded by hemorrhage) on funduscopy. ● Pericardial friction rub. ● JVD, rales, gallops with HF. ● Cold, pale extremity with absent pulse in septic emboli. ● Focal neurologic signs in septic emboli. Diagnostic Studies ● Positive blood cultures (multiple 2 to 3; 2 by Duke criteria) for typical organisms. ● Echo disclosing vegetations; TEE may be especially sensitive. ● Leukocytosis. ● Elevated ESR or C-reactive protein. ● Microscopic hematuria on UA.● Anemia (normocytic) in SBE on CBC. ● Positive rheumatoid factor in SBE. ● Circulating immune complexes, decreased C3 and C4. ● CXR—infiltrates, pleural effusion. Management ● IV antibiotics for 4 to 6 weeks; penicillin G for penicillin-susceptible S. viridans, and others as indi-cated by culture and sensitivity results. ● Surgical consultation for valve replacement should be considered in complicated cases (e.g., with HF, emboli, dehiscence of prosthetic valve, or resistance to antibiotics). Prophylaxis —In 2007 the AHA, in conjunction with the professional organizations representing dentistry (ADA), infectious disease (IDSA), and pediatrics (AAP), published updated recommendations for the prevention of IE. The new guidelines recommend that antibiotic prophylaxis be administered only to patients undergoing dental procedures who are at the highest risk of adverse outcomes from IE (see X.G. below). They no longer recommend prophylaxis for lower-risk patients (such as those with most types of VHD including MVP), or for patients undergoing genitourinary or gastrointestinal (GI) procedures. Patients at highest risk should receive antibiotic prophylaxis— amoxicillin 2 g PO 30 to 60 minutes prior to the procedure (cephalexin, clindamycin, azithromycin, or clarithromycin may be used for penicillin-allergic patients.) Cardiac Conditions Requiring IE Prophylaxis: ● Prosthetic cardiac valves. ● Previous IE ● Cardiac transplantation recipients who develop VHD. ● Congenital Heart Disease: Unrepaired cyanotic CHD, including palliative shunts and conduits. Completely repaired CHD defects with prosthetic material or device during the first 6 months after the procedure. Repaired CHD with residual defects at the site or adjacent to the site of the patch or device. Pericarditis Etiology ● Idiopathic. ● Viral—coxsackie virus, echovirus, HIV, adenovirus, Epstein-Barr virus, mumps virus. ● Bacterial—Staphylococcus, Pneumococcus, Mycoplasma, tuberculosis. ● Fungal. ● Lyme disease. ● Parasites. ● Collagen vascular diseases—rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), scleroderma. ● AMI. ● Cardiac surgery. ● Uremia. ● Neoplasm (lung, lymphoma, mesothelioma). ● Trauma. ● Radiation. ● Myxedema. ● Sarcoidosis. ●Pancreatitis. ● Inflammatory bowel disease. ● Aortic dissection. Drugs—procainamide, hydralazine, minoxidil, bleomycin, phenytoin, mesalamine. Pathology ● Inflammation of pericardial sac can cause effusion. When effusion is large enough to decrease cardiac output, it is called cardiac tamponade and is a medical emergency. Constrictive pericarditis—caused by chronic pericardial inflammation leading to fibrosis, scarring, and calcfication. Demographics ● Men > women. Clinical Features History ● Sharp retrosternal chest pain with radiation to back and shoulder, intensifies with inspiration and lying supine, relieved by sitting up and leaning forward. ● Odynophagia. ● Anorexia. ● Anxiety. ● Myalgia. Physical Exam Findings ● Fever. ● Splinted breathing. ● Pericardial friction rub (three components— systolic, early diastolic, late diastolic). ● Dysrhythmias—SVT. ● Tachypnea. Pericardial Tamponade History ● Dyspnea. ● Tachycardia. Physcial Exam Findings ● Cyanosis. ● JVD. ● Hypotension. ● Pulsus paradoxus. ● Muffled heart tones. Constrictive Pericarditis ● Can be asymptomatic early in course. ● Dyspnea. ● Fatigue. ● JVD. ● Peripheral edema. ● Hepatomegaly, ascites. Diagnostic Studies ● ECG—acute phase with concave-up ST elevation in precordial leads, especially with absence of reciprocal ST depression seen in AMI. Intermediate phase ST segment returns to baseline and T waves invert. In late phase, ECG can return to normal. In constrictive pericarditis and cardiac tamponade, ECG may disclose low QRS voltage. In cardiac tamponade, electrical alternans may be seen. ● Echo to detect pericardial effusion. ● Leukocytosis. ● Elevated ESR. ● CXR may show large effusion, but not nearly as sensitive or specfic as Echo. ● May see mildly elevated cardiac enzymes, especially CK-MB. ● Viral titers, antinuclear antibody, rheumatoid factor, purified protein derivative, antistreptolysin O (ASO) titers, BUN, creatinine, and blood cultures may be helpful in elucidating the cause. ● Cardiac catheterization should be considered in constrictive pericarditis. Management Uncomplicated Acute Pericarditis ● Acetylsalicylic acid (ASA), NSAIDs, or prednisone. ● Analgesia (e.g., codeine). ● Rest. ● Observation for signs/symptoms of evolving tamponade. ● Treat underlying etiology. Chronic Constrictive Pericarditis ● Cardiothoracic surgery referral for possible stripping. Cardiac Tamponade ● Immediate pericardiocentesis. ● Cardiothoracic surgery referral for pericardial window drainage, if recurrent. Pericardial Effusion Key Features Can develop from any form of pericarditis Slow development of large effusions may produce no hemodynamic effects Rapid appearance of smaller effusions can cause cardiac tamponade (elevated intrapericardial pressure that restricts venous return and ventricular filling), leading to shock and death Clinical Findings Pain in acute inflammatory pericarditis; neoplastic and uremic effusions are often painless Dyspnea and cough, especially with tamponade Other symptoms reflect primary disease Pericardial friction rub may be present (even with large effusions) Pulsus paradoxus (> 10 mm Hg decline in systolic pressure during inspiration) is common Characteristic features of tamponade o Tachycardia o Tachypnea o Narrow pulse pressure o Preserved systolic pressure Elevation of central venous pressure, edema, or ascites in chronic processes Hypotension, paradoxical pulse and an elevated jugular venous pressure all important signs Diagnosis • • ECG – Often reveals nonspecific T wave changes and reduced QRS voltage – Electrical alternans is pathognomonic Chest radiograph: normal or enlarged cardiac silhouette with a globular configuration Treatment Echocardiography is primary mode of diagnosis Diagnostic pericardiocentesis or biopsy is often indicated for microbiologic and cytologic studies Yield of diagnostic pericardial tap is low Small effusions can be followed clinically and by echocardiogram Urgent pericardiocentesis is required for tamponade Partial pericardiectomy may be required for recurrent effusion in neoplastic disease and uremia, either by video-assisted thoracic surgery (VATS) or thoracotomy Additional therapy (eg, dialysis) for the primary disease Rheumatic Fever and Heart Disease Etiology ● Group A—b-hemolytic streptococcal pharyngitis. Pathology ● An inflammatory immunologic response to strepto-coccal infection affecting the heart (endocardium and valves, myocardium, pericardium), skin, joints, and central nervous system (CNS); recurrences are common. Demographics ● Children of ages 5 to 15. ● Incidence in United States dropping. Clinical Features ● Symptoms of rheumatic fever commonly occur 1 to 3 weeks after pharyngitis episode. ● Symptoms of VHD from childhood infection can be delayed until third or fourth decade. Modified Jones Criteria For Diagnosis Of Initial Attack ● With documented preceding group A streptococcal infection (throat culture, throat rapid antigen detection test, elevated or rising strep antibody titers), two major manifestations or one major and two minor manifestations. Major Manifestations ● Carditis (pericarditis, myocarditis, VHD that can affect any valve, but mitral and aortic lesions are most common). ● Polyarthritis (medium to large joints; knees, ankles, wrists). Migratory and disappear within 3 to 4 weeks. ● Chorea (late finding). ● Erythema marginatum. ● Subcutaneous nodules (painless over bony prominences). Minor Manifestations ● Arthralgia (this cannot be used as minor criterion a part of the Modified Jones Criteria if polyarthritis is used as a major criterion). ● Fever (101° to 104° F). ● Prolonged PR interval. ● Elevated acute phase reactants. Other Manifestations Outside Of Jones Criteria ● Abdominal pain. ● Facial tics or grimace. ● Epistaxis. Diagnostic Studies ● Acute phase reactants (e.g., ESR, C-reactive protein) elevated. ● Antistreptolysin O (ASO), antideoxyribonuclease B (DNase), rapid strep antigen test, or throat culture bacteriologic or serologic evidence group A strep infection. ● ECG—prolonged PR interval. ● Echo—pericardial effusion or valvular lesions (cannot use as a sole diagnostic method). ● CBC—anemia. Management ● Penicillin to treat streptococcal infection. ● Prednisone for carditis with cardiomegaly. ● Aspirin if no cardiomegaly. ● Haloperidol to treat chorea.