* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Antidepressants and neuroleptic
Nicotinic agonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Toxicodynamics wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Prescription costs wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Chlorpromazine wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Antipsychotic wikipedia , lookup
Neuropharmacology wikipedia , lookup
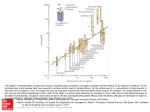
Psychotropic drugs Prof elham aljammas Sept 2015 objectives Identify general pharmacologic strategies Discuss antidepressants including indications for use and side effects Describe mood stabilizers including indications for use and side effects Review antipsychotics including how to choose an antipsychotic and side effects Identify anxiolytic classes and indications for use Management strategies -Adjust dosage for optimum benefit, safety and compliance. -Use adjunctive and combination therapies if needed however always strive for the simplest regimen. -Keep your therapeutic endpoint in mind. Psychotropic drugs Treat mood, cognition, and behavioral disturbances associated with psychological disorders Most are not used recreationally or abused Benzodiazepines are the exception General classes of disorders Mood Anxiety Psychotic Other Disorders Attention Deficit Disorder Depression Depression is a serious disorder that afflicts approximately 14 million adults in the United States each year. The lifetime prevalence rate of depression in the United States has been estimated to include 16 percent of adults (21 percent of women, 13 percent of men), or more than 32 million people Antidepressants Indications: Unipolar and bipolar depression, organic mood disorders, schizoaffective disorder, anxiety disorders including OCD, panic, social phobia, PTSD, premenstrual dysphoric disorder and impulsivity associated with personality disorders. General guidelines Antidepressant efficacy is similar so selection is based on past history of a response, side effect profile and coexisting medical conditions. There is a delay typically of 3-6 weeks after a therapeutic dose is achieved before symptoms improve. If no improvement is seen after a trial of adequate length (at least 2 months) and adequate dose, either switch to another antidepressant or augment with another agent. Mood disorders/Antidepressants MAO Inhibitors Tricyclics Selective Serotonin Reuptake Inhibitors Dual Action Antidepressants Selective Norepinephrine Reuptake Inhibitors Atypical antidepressant Mood Stabilizers (Antimanic Agents) LithiumCarbonate Valproic Acid Carbamazepine Lamotragine Topirimate MAOI Use in late 1950s & ended in early 1960s use ended due to side effect (death) MAO breaks down many chemicals including tyramine Tyramine is present in cheeses, red wines, alcohol, smoked fish MAO in liver breaks down tyramine Causes a hypertensive crisis "cheese syndrome" increased blood pressure ➔ stroke ➔ death increased heart rate ➔ heart attack ➔ death MAOI Bind irreversibly to monoamine oxidase thereby preventing inactivation of biogenic amines such as norepinephrine, dopamine and serotonin leading to increased synaptic levels. Are very effective for depression Side effects include orthostatic hypotension, weight gain, dry mouth, sedation, sexual dysfunction and sleep disturbance Hypertensive crisis can develop when MAOI’s are taken with tyramine-rich foods or sympathomimetics. MAOI Serotonin Syndrome can develop if take MAOI with meds that increase serotonin or have sympathomimetic actions. Serotonin syndrome sx include abdominal pain, diarrhea, sweats, tachycardia, HTN, myoclonus, irritability, delirium. Can lead to hyperpyrexia, cardiovascular shock and death. To avoid need to wait 2 weeks before switching from an SSRI to an MAOI. The exception of fluoxetine where need to wait 5 weeks because of long half-life. SSRI s Tricyclic antidepressants Act as agonists to catecholamines No "cheese syndrome" Side effects are the major problem Cardiotoxic Sedative action Block acetylcholine system, especially muscarinic receptors blurred vision, dry mouth, urinary retention, constipation, mental confusion Block histamine receptors - sedation prescaution Very effective but potentially unacceptable side effect profile i.e. antihistaminic, anticholinergic, antiadrenergic Lethal in overdose (even a one week supply can be lethal!) Can cause QT lengthening even at a therapeutic serum level TCA Have tertiary amine side chains Side chains are prone to cross react with other types of receptors which leads to more side effects including antihistaminic (sedation and weight gain), anticholinergic (dry mouth, dry eyes, constipation, memory deficits and potentially delirium), antiadrenergic (orthostatic hypotension, sedation, sexual dysfunction) Act predominantly on serotonin receptors Examples:Imipramine, amitriptyline, doxepin, clomipramine SSRI Selectively block re-uptake of 5-HT Work on DA and NE as well but very little Eliminate ACh and antihistamine effects No more effective than MAOIs or tricyclics Better because there are fewer side effects On market since late 1980s & early 1990s Fluoxetine – Prozac Sertraline - Zoloft Paroxetine - Paxil Fluvoxamine - Luvo Citalopram - Celexa Escitalopram - Lexapro SSRI Selectively block re-uptake of 5-HT Work on DA and NE as well but very little Eliminate ACh and antihistamine effects No more effective than MAOIs or tricyclics Better because there are fewer side effects On market since late 1980s & early 1990s Fluoxetine – Prozac Sertraline - Zoloft Paroxetine - Paxil Fluvoxamine - Luvo Citalopram - Celexa Escitalopram - Lexapro Selective serotonin reuptake inhibitors Block the presynaptic serotonin reuptake Treat both anxiety and depressive Most common side effects include GI upset, sexual dysfunction (30%+!), anxiety, restlessness, nervousness, insomnia, fatigue or sedation, dizziness Very little risk of cardiotoxicity in overdose Can develop a discontinuation syndrome with agitation, nausea, disequilibrium and dysphoria SNRI Selectively inhibits NE transporter. Blocks re-uptake. Atomoxetine (Strattera) Reboxetine (Edronax,Vestra) Dual action AD Affinity for both 5-HT and NE. Block re-uptake for both In this sense, like TCAs Duloxetine - Cymbalta Atypical Antidepressants The atypical antidepressants are a mixed group of agents that have actions at several different sites. This group includes bupropion , mirtazapine ,nefazodone], and trazodone atypical antidepressants Bupropion (Wellbutrin) No effect on either 5-HT or NE Effective at blocking DA reuptake May be similar action to cocaine Lowers seizure threshold Venlafaxine (Effexor) 5-HT, DA and NE reuptake blocker Drugs for bipolar Treat the manic phases of Bipolar Disorder Lithium Valproic Acid Carbamazepine/Oxcarbazepine Lamotragine Topirimate Symbyax – Combo of olanzepine and fluoxetine (Zyprexa & Prozac) Mood Stabilizers Indications: Bipolar, cyclothymia, schizoaffective, impulse control and intermittent explosive disorders. Classes: Lithium, anticonvulsants, antipsychotics Which you select depends on what you are treating and again the side effect profile. lithium Only medication to reduce suicide rate. Rate of completed suicide in BAD ~15% Effective in long-term prophylaxis of both mania and depressive episodes in 70+% of BAD I pts Factors predicting positive response to lithium Prior long-term response or family member with good response Classic pure mania Mania is followed by depression LITHIUM Before starting :Get baseline creatinine, TSH and CBC. In women check a pregnancy testduring the first trimester is associated with Ebstein’s anomaly 1/1000 (20X greater risk than the general population) Monitoring: Steady state achieved after 5 days- check 12 hours after last dose. Once stable check q 3 months and TSH and creatinine q 6 months. Goal: blood level between 0.6-1.2mmol /lit Lithium side effects Most common are GI distress including reduced appetite, nausea/vomiting, diarrhea Thyroid abnormalities Non significant leukocytosis Polyuria/polydypsia secondary to ADH antagonism. In a small number of patients can cause interstitial renal fibrosis. Hair loss, acne Reduces seizure threshold, cognitive slowing, intention tremor Lithium toxicity Mild- levels 1.5-2.0 see vomiting, diarrhea, ataxia, dizziness, slurred speech, nystagmus. Moderate-2.0-2.5 nausea, vomiting, anorexia, blurred vision, clonic limb movements, convulsions, delirium, syncope Severe- >2.5 generalized convulsions, oliguria and renal failure Study Questions Choose the ONE best answer. 12.1 A 55-year-old teacher began to experience changes in mood. He was losing interest in his work and lacked the desire to play his daily tennis match. He was preoccupied with feelings of guilt, worthlessness, and hopelessness. In addition to the psychiatric symptoms, the patient complained of muscle aches throughout his body. Physical and laboratory tests were unremarkable. After 6 weeks of therapy with fluoxetine, the patient's symptoms resolved. However, the patient complains of sexual dysfunction.Which of the following drugs might be useful in this patient? A. Fluvoxamine. B. Sertraline. C. Citalopram. D. Mirtazapine. E. Lithium. Correct answer = D. Sexual dysfunction commonly occurs with TCAs, SSRIs, and SNRIs. Mirtazapine is largely free from sexual side effects. A 25-year-old woman has a long history of depressive symptoms accompanied by body aches. Physical and laboratory tests are unremarkable. Which of the following drugs might be useful in this patient? A. Fluoxetine. B. Sertraline. C. Phenelzine. D. Mirtazapine. E. Duloxetine. Correct answer = E. Duloxetine is an SNRI that can be used for depression accompanied by neuropathic pain. MAOs and SSRIs have little activity against neuropathic pain A 51-year-old woman with symptoms of major depression also has narrow-angle glaucoma. Which of the following antidepressants should be avoided in this patient? A. Amitriptyline. B. Sertraline. C. Bupropion. D. Mirtazepine. E. Fluvoxamine. Correct answer = A. Because of its potent antimuscarinic activity, amitriptyline should not be given to patients with glaucoma because of the risk of acute increases in ocular pressure. The other antidepressants all lack antagonist activity at the muscarinic receptor. A 36-year-old man presents with symptoms of compulsive behavior. If anything is out of order, he feels that “work will not be accomplished effectively or efficiently.― He realizes that his behavior is interfering with his ability to accomplish his daily tasks but cannot seem to stop himself. Which of the following drugs would be most helpful to this patient? A. Imipramine. B. Fluvoxamine. C. Amitriptyline. D. Tranylcypromine. E. Lithium. Correct answer = B. Selective serotonin reuptake inhibitors are particularly effective in treating obsessivecompulsive disorder; flu vox amine is approved for this condition. The other drugs are ineffective in the treatment of obsessive-compulsive disorder. Neuroleptics prof Dr Elham Aljammas 23/10/2013 Antipsychotics used to treat schizophrenia. Schizophrenia is a severe chronic disorder Positive symptoms: hallucinations, and delusions Negative symptoms: amotivation, poverty of speech, flat affect Disorganized symptoms: speech, thought, and behavior Now being used to treat Bipolar as well Antipsychotics Indications for use: schizophrenia, schizoaffective disorder, bipolar disorder- for mood stabilization and/or when psychotic features are present, delirium, psychotic depression, dementia, trichotillomania, augmenting agent in treatment resistant anxiety disorders. Pathways affected by DA in the Brain Antagonize dopamine – block a specific receptor Typical Chlorpromazine Trifluperazine Thorazine Haloperidol – (Haldol) Atypical Risperdal - Risperidone Olanzepine - Zyprexia Quetiapine - Seroquel Ziprasidone – Geodon Aripiprazole – Abilify Paliperidone – Invega The Atypical Antipsychotics agents are serotonindopamine 2 antagonists (SDAs) They are considered atypical in the way they affect dopamine and serotonin neurotransmission in the four key dopamine pathways in the brain. - atypical Antipsychotics drugs (typical) group drug Usual dose phenothiazines chlorpromazine 100-1500mg daily butyrophenones haloperidol thioxanthenes flupentixol Diphenylbutylpiperidines Pimozide 5-30mg daily 50-100mg IMI monthly 5mg IMI orIVI on need 40-200mg fortnight Short & long acting 4-30mg daily Neuroleptics . The traditional or typicalneuroleptic drugs (also called conventional or first-generation antipsychotics) are competitive inhibitors at a variety of receptors, but their antipsychotic effects reflect competitive blocking of dopamine receptors. These drugs vary in potency. For example, chlorpromazine is a low-potency drug, and fluphenazine is a high-potency agent No one drug is clinically more effective than another. Atypical antipsychotic agent group drugs Usual dose dibenzodiazepine clozapine 25-900mg daily Bezisoxazole Quetiapine - Risperidone Seroquel 2-16mg daily 100-200mg/d thienobenzodiazepin olanzapine 5-20mg daily Atypical atypical agents are serotonindopamine 2 antagonists (SDAs) They are considered atypical in the way they affect dopamine and serotonin neurotransmission in the four key dopamine pathways in the brain. Mechanism of action Dopamine receptor blocking activity in the brain:. D1 and D5 receptors activate adenylyl cyclase, often exciting neurons, whereas D2, D3 and D4 receptors inhibit adenylyl cyclase, or mediate membrane K+ channel opening leading to neuronal hyperpolarization. The neuroleptic drugs bind to these receptors to varying degrees. However, the clinical efficacy of the typical neuroleptic drugs correlates closely with their relative ability to block D2 receptors in the mesolimbic system of the brain. atypical drug clozapine has higher affinity for the D4 receptor and lower affinity for the D2 receptor, which may partially explain its minimal ability to cause extrapyramidal side effects (EPS). Serotonin receptor blocking activity in the brain: Most of the newer atypical agents appear to exert part of their unique action through inhibition of serotonin receptors (5-HT), particularly 5-HT2A receptors. (clozapine ,olanzapine,aripiprazole , Quetiapine ). The undesirable side effects of these agents, however, are often a result of actions at these other receptors. Antipsychotic actions: All of the neuroleptic drugs can reduce the hallucinations and delusions associated with schizophrenia by blocking dopamine receptors in the mesolimbic system of the brain. The antipsychotic effects usually take several days to weeks to occur, suggesting that the therapeutic effects are related to secondary changes in the corticostriatal pathways. Extrapyramidal effects: Dystonias (sustained contraction of muscles leading to twisting distorted postures), parkinson-like symptoms, akathisia (motor restlessness), and tardive dyskinesia (involuntary movements of the tongue, lips, neck, trunk, and limbs) occur with chronic treatment. Blocking of dopamine receptors in the nigrostriatal pathway probably causes these unwanted movement symptoms. The atypical neuroleptics exhibit a lower incidence of these symptoms. Antiemetic effects: With the exceptions of aripiprazole and thioridazine , most of the neuroleptic drugs have antiemetic effects that are mediated by blocking D2-dopaminergic receptors of the chemoreceptor trigger zone of the medulla. Antimuscarinic effects: Some of the neuroleptics, particularly thioridazine, chlorpromazine, clozapine, and olanzapine ,produce anticholinergic effects, including blurred vision dry mouth (exception: clozapine increase salivation), confusion, and inhibition of gastrointestinal and urinary tract smooth muscle, leading to constipation and urinary retention. This anticholinergic property may actually assist in reducing the risk of EPS with these agents. Important side effects to be considered when choosing antipsychotic drugs ◦ 1-Extrapyramidial side effects: Atypical antipsychotic has less extrapyramidal effect. 2-hyperprolactinaemia: Lead to menstrual disturbances,increased risk of malignancy,increased galactorrhea,& increased osteoporosis. Prolactine sparingis aripiprazole 3-sedationIncreased sedation with high affinity to histamine& muscarinic receptors CPZ,olanzapine,clozapine Helpful in acute state 4-weight gain: Histamine & 5HT R block (>olanzapine)less with resperidone,amisulpride,&aripipraz 5.Type 11 DM >clozapine &olanzapine Should be monitored by Bd sugar,lipid profile& weight. 6-CV& cerbrovascular events , through their effect on the lipid profile ,Wt,& insulin resistance. Some produce prolonge QT interval. olanzapine& resperidone 7-postural hypotension 8-sexual dysfunction 9-photosensitivity 10-agranulocytosis 11-constipation 12-reduction of fit threshold Other effects: Blockade of -adrenergic receptors causes orthostatic hypotension and lightheadedness. The neuroleptics also alter temperature-regulating mechanisms and can produce poikilothermia (body temperature varies with the environment). In the pituitary, neuroleptics block D2 receptors, leading to an increase in prolactin release. Atypical neuroleptics are less likely to produce prolactin elevations. Sedation occurs with those drugs that are potent antagonists of the H1-histamine receptor, including chlorpromazine, olanzapine, quetiapine, and clozapine. Sexual dysfunction may also occur with the antipsychotics due to various receptor-binding characteristics. Therapeutic uses Treatment of schizophrenia: The neuroleptics are considered to be the only efficacious treatment for schizophrenia. Prevention of severe nausea and vomiting: The older neuroleptics (most commonly prochlorperazine) are useful in the treatment of drug-induced nausea Other uses: The neuroleptic drugs can be used as tranquilizers to manage agitated and disruptive behavior secondary to other disorders. Neuroleptics are used in combination with narcotic analgesics for treatment of chronic pain with severe anxiety . Chlorpromazine is used to treat intractable hiccups. Promethazine, this agent is used in treating pruritus . Pimozide is primarily indicated for treatment of the motor and phonic tics of Tourette's disorder. risperidone and haloperidol are also commonly prescribed for this tic disorder. Also, risperidone is now approved for the management of disruptive behavior and irritability secondary to autism Antipsychotic adverse effect Tardive Dyskinesia (TD)-involuntary muscle movements that may not resolve with drug discontinuation- risk approx. 5% per year Neuroleptic Malignant Syndrome (NMS): Characterized by severe muscle rigidity, fever, altered mental status, autonomic instability, elevated WBC, CPK and lfts. Potentially fatal. Extrapyramidal side effects (EPS): Acute dystonia, Parkinson syndrome, Akathisia Adverse effects . Parkinson-like symptoms of bradykinesia, rigidity, and tremor usually occur within weeks to months of initiating treatment. Clozapine can produce bone marrow suppression, seizures, and cardiovascular side effects. The risk of severe agranulocytosis necessitates frequent monitoring of white-blood-cell counts . The neuroleptics depress the hypothalamus, affecting thermoregulation, and causing amenorrhea, galactorrhea, gynecomastia, infertility, and impotence. Significant weight gain is often a reason for noncompliance. It is also recommended that glucose and lipid profiles be monitored in patients taking antipsychotics The choice of medication &dose :depend on 1-sevirety of the problems. 2-degree of sedation required. 3-side effect profile. 4-preferance of individual clinician. Study Questions Choose the ONE best answer. 13.1 An adolescent male is newly diagnosed with schizophrenia. Which of the following neuroleptic agents may improve his apathy and blunted affect? A. Chlorpromazine. B. Fluphenazine. C. Haloperidol. D. Risperidone. E. Thioridazine Correct answer = D. Risperidone is the only neuroleptic on the list that has some benefit in improving the negative symptoms of schizophrenia. All the agents have the potential to diminish the hallucinations and delusional thought processes. Which one of the following neuroleptics has been shown to be a partial agonist at the D2 receptor? A. Aripiprazole. B. Clozapine. C. Haloperidol. D. Risperidone. E. Thioridazine. Correct answer = A. Aripiprazole is the agent that acts as a partial agonist at D2 receptors. Theoretically, the drug would enhance action at these receptors when there is a low concentration of dopamine and would block the actions of high concentrations of dopamine. All the other drugs are only antagonistic at D2 receptors, with haloperidol being particularly potent. A 21-year-old male has recently begun pimozide therapy for Tourette's disorder. He is brought to the emergency department by his parents. They describe that he has been having “differentappearing tics― than before, such as prolonged contraction of the facial muscles. While being examined, he experiences opisthotonus (spasm of the body where the head and heels are bent backward and the body is bowed forward. A type of extrapyramidal effect). Which of the following drugs would be beneficial in reducing these symptoms? A. Benztropine. B. Bromocriptine. C. Lithium. D. Prochlorperazine. E. Risperidone Correct answer = A.The patient is experiencing extrapyramidal symptoms due to pimozide, and a muscarinic antagonist such as benztropine would be effective in reducing the symptoms.The other drugs would have no effect or, in the case of prochlorperazine, might increase the symptoms. A 28-year-old woman with schizoid affective disorder and difficulty sleeping would be most benefited by which of the following drugs? A. Aripiprazole. B. Chlorpromazine. C. Haloperidol. D. Risperidone. E. Ziprasidone. Correct answer = B. Chlorpromazine has significant sedative activity as well as antipsychotic properties. Of the choices, it is the drug most likely to alleviate this patient's major complaints, including her insomnia Anxiolytic Prof. Dr Elham Aljammas Anxiolytic Treat anxiety disorders Generalized Anxiety Disorder Panic Disorder PTSD OCD Social Anxiety Disorder (SAD) Anxiolytic Used to treat many diagnoses including panic disorder, generalized Anxiety disorder, substance-related disorders and their withdrawal, insomnias and parasomnias. In anxiety disorders often use anxiolytics in combination with SSRIS or SNRIs for treatment. Benzodiazepines Used to treat insomnia, parasomnias and anxiety disorders. Often used for CNS depressant withdrawal protocols ex. ETOH withdrawal. Side effects/cons Somnolence Cognitive deficits Amnesia Disinhibition Tolerance Dependence Dose Equivalency (mg) Drug Alprazolam (Xanax) 0.5 Peak Blood Level (hours) Elimination HalfLife1 (hours) 1-2 12-15 Rapid oral absorption 2-4 15-40 Active metabolites; erratic bioavailability from IM injection 1-4 18-50 Can have layering effect 1-2 20-80 Active metabolites; erratic bioavailability from IM injection 1-2 40-100 Active metabolites with long half-lives 1-6 10-20 No active metabolites 2-4 10-20 No active metabolites 2-3 10-40 Slow oral absorption Comments 10.0 Chlordiazepoxide (Librium) Clonazepam (Klonopin) 0.25 5.0 Diazepam (Valium) 30.0 Flurazepam (Dalmane) Lorazepam (Ativan) Oxazepam (Serax) Temazepam (Restoril) 1.0 15.0 30.0 0.25 Triazolam (Halcion) 1 2-3 Rapid onset; short duration of action Monitor for efficacy and tolerance and adjust as indicated. If the patient does not improve step back, rethink your diagnosis and treatment plan! Keep an eye on drug-drug interactions Benzodiazepines Facilitate GABA neurotransmission Bind to a particular site on the GABA receptor Xanax, Ativan, Valium, Serax, Librium Beta-Blockers Antagonize NE by blocking Beta receptor subtype SSRIs PTSD, OCD, SAD, and to some degree GAD Others Buspar Non-sedating Does not interact with alcohol Not highly effective ADD Methylphenidate – Ritalin DA reuptake inhibitor So slowly it enters the brain that it is not addictive like cocaine even though they have the same mechanism Concerta (Immediate release combined with time release) Adderal (mixed amphetamine salts) Has extended release Modafinil – Provigil Vyvanse An amphetamine pro-drug Less abusable Straterra Mixing Med. Although classified as a certain type of drug most psych meds used for many different disorders. Antipsychotics in Bipolar Disorder Abilify Zyprexa Mood stabilizers in alcoholism Topiramate Prescribing a medication for a disorder when it is known to work, but there is no formal FDA indication is called “off-label prescribing” It’s perfectly legal and quite common Thank You