* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Heel 2
Survey
Document related concepts
Discovery and development of proton pump inhibitors wikipedia , lookup
NMDA receptor wikipedia , lookup
Drug interaction wikipedia , lookup
Toxicodynamics wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
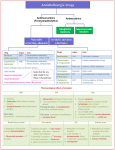
Cholinergic receptors: Acetylcholine acts on two types of receptors: Nicotinic Site Muscarinic -All autonomic ganglia(NN) -All organs supplied by -Adrenal medulla (NN) parasympathetic fibers. Neuro-muscular junction(NM) -Sweat glands supplied by sympathetic fibers. NN: Ganglion blockers e.g. Blocker hexamethonium Atropine NM: Neuromuscular blockers e.g. Curare. N.B. Endothelium of most blood vessels releases EDRF (Endothelium Derived Relaxing Factor) =nitric oxide (NO) inducing VD through non-innervated muscarinic receptors. *Muscarinic receptors are subdivided into M1- M5 M1 Site Effect M2 -Exocrine glands. Heart M3 -Exocrine glands. -Parietal cells of -Smooth muscles. stomach. -Vascular -CNS. endothelium. -Exocrine gland HR and AV -Exocrine secretion. conduction -HCl secretion. gland excretion. -Smooth muscle contraction. -Hypotension. Selective Pirenzipine -Gallamine antagonist The exact role of M4 and M5 are not yet identified. 9 Darifenacin Removal of Acetyl choline: Rapidly hydrolyzed by acetylcholinesterase enzyme (2 types): *True: found at all sites of A Ch release. *Pseudo: found in plasma and liver. PARASYMPATHOMIMETICS Drugs which stimulate muscarinic receptors (muscarinic agonists) with or without nicotinic action. They are classified into: A- Directly Acting: 1- Choline esters: A.Ch. (Natural), Methacholine, Carbachol and Bethanecol (Synthetic) 2- Cholinomimetic Alkaloids: Pilocarpine and muscarine. B- Indirectly Acting (Anticholinesterases): anticholinesterase accumulation of endogenous A.Ch infront of cholinergic receptors(Muscarinic & Nicotinic) effects that mimic the parasympathetic nervous system. They are subdivided into: *Reversible as physostigmine, Neostigmine, Edrophonium. *Irreversible as organophosphorous compounds. I. Choline Esters They are quaternary amines, so can not pass to C.N.S. and are distributed extracellular. The following table shows the main pharmacological differences between different choline esters: 10 Acetylcholine Hydrolysis by True cholinesterase Methacholine and True only psuedo Nicotinic Carbachol Not Bethanechol hydrlysed by true or psuedo ++++ ++++ --- ++++ ++++ ++++ ++++ action Muscarinic action Non-specific Specificity of (Has the same muscarinic efficacy on M action CVS Eye , and receptors all over the body) Urinary bladder Not used due Peripheral Clinical uses GIT very 1- Glaucoma short vascular duration action (why?) 2- Paralytic ileus of diseases e.g. 3-Non-obstructive urine retention Raynaud’s disease. II- Cholinomimetics Alkaloids: Pilocarpine Actions: Act directly on muscarinic receptors with marked action on eye, exocrine glands and smooth muscles. Uses: -Eye drops in glaucoma. -Promotion of hair growth. Contraindications of directly acting parasympathomimitics: 1-Bronchial asthma. 2-Peptic ulcer. 3-Coronary insufficiency, hypotension and bradycardia. 5-Never given I.M. or I.V. (produce severe bradycardia and hypotension and Atropine is the antidote). 11 Anticholinesterases -They inhibit cholinesterase enzyme so produce accumulation of ACh. at cholinergic sites (muscarinic and nicotinic). -ACh. Undergoes 2 steps hydrolysis 1st binds to the active site of the enzyme and is hydrolyzed into free choline and acetylated enzyme, the 2 nd step is splitting of acetylated enzyme to acetic acid and free enzyme which occurs in 150 microseconds: 1-Reversible anticholinesterases include: *Edrophonium: It binds to the active anionic site of the enzyme for 5 minutes and then excreted in urine unchanged so it is not substrate for the enzyme. Quaternary amine given I.V. Used for diagnosis of myasthenia gravis. *Carbamates (Physostigmine, Neostigmine) undergo 2 step hydrolysis as ACh., but the carbamylated enzyme is resistant to hydrolysis (prolonged to 0.5 - 6 hours). They are substerate for the enzyme. Physostigmine (Eserine) Neostigmine Source Natural Synthetic Chemistry Tertiary amine (-N-) i.e. Quaternary amine (-N-) non-ionized i.e. ionized Oral absorption Complete Incomplete Passage through Can pass Can’t pass BBB 12 Actions *Muscarinic: more on eye *Muscarinic: more on *Nicotinic. GIT *CNS stimulation *Nicotinic. *Direct skeletal muscle convulsions. stimulation. Uses 1-Glaucoma. 1-Diagnosis and 2-Antidote to atropine i.e. treatment of Myasthenia used in treatment of Gravis. atropine or atropine like 2-Antidote to curare. drugs e.g. TCAs poisoning. 3.post-operative urine retention and paralytic ileus. Neostigmine Substitutes: •Pyridostigmine: used in treatment of myasthenia gravis. •Demecarium: Local long acting miotic in glaucoma. •Tacrine has anticholinesterase activity and is used in treatment of Alzheimer's disease. It is hepato-toxic. •Donepezil, Galantamine and rivastagmine are more selective cholinesterase inhibitor in treatment of Alzheimer’s disease and are not hepatotoxic Myasthenia Gravis Disease of neuromuscular junction characterized by weakness on repetition of movement. It is an autoimmune process, which cause production of antibodies that decrease the number of functional nicotinic (NM) receptors on 13 the motor end plate. It is diagnosed by neostigmine or by edrophonium (muscle weekness is improved). It is treated by cholinesterase inhibitors as Neostigmine (give atropine before) or neostigmine substitutes (pyridostigmine), also immunosuppressants (cordcosteroids) may be tried and surgical removal of thymoma if present. 2- Irreversible anticholinesterases: They combine with the active site of the enzyme but the phosphorylated enzyme is stable (needs hundreds of hours for hydrolysis). This phosphorylated enzyme may undergoes aging process, which strengthens the bond, and induces complete and permanent enzyme inactivation and so they have long duration until new enzyme synthesis. Organo-Phosphorus Compounds They are non-competitive irreversible inhibitors for cholinesterase enzyme. Most of them are highly lipid soluble. They are used as: 1-Insecticides: Parathion and Malathion.. 2-War gas: Tabun, Sarin and Soman. Organophosphorus Poisoning: It is due to inhalation of sprays or dusts of insecticides or contamination of skin or food. It may be caused as a result for chemical wars. Death is due to respiratory failure (central or peripheral). * Treatment: 1-Care of respiration by artificial respiration and suction of secretions. 14 1-Atropine 2 mg. I.V. or I.M./10 minutes until pupil dilates and skin dries. It antagonizes the muscarinic effects central and peripheral. 2-Cholmesterases reactivators (oximes) as Pralidoxime (PAM), diacetyl monoxime (DAM). They combine with the poison in blood and may dephosphorylate the enzyme if given early before aging of the enzyme. They reverse muscle weakness and are used with atropine. PAM can not pas to C.N.S. but DAM. crosses blood brain barrier. 3-Symptomatic treatment e.g. anticonvulsants as diazepam. Muscarinic Receptor Antagonists (Parasympathetic depressants) They produce competitive reversible blockade of the actions of A.Ch. at muscarinic (M) receptors. They are classified into: I. Natural Belladonna alkaloids which include Atropine and Hyoscine. They are tertiary amine compounds. II. Synthetic derivatives. ATROPINE Actions: 1-Eye: Local atropine application lasts for 7-10 days. *Block of M receptors in constrictor pupillae muscle: Passive Mydriasis & Loss of reaction to light (-ve light reflex). *Block of M receptors in Cilliary muscle Relaxation of ciliary muscle (cycloplegia) loss of accommodation for near vision. Impair aqueous humor drainage IOP. * lacrimation. 15 2-Secretions: salivary, bronchial, gastric, and sweat secretion. 3-Bronchi: Bronchodilatation and dryness of secretions. 4-C.V.S:. *small doses I.V. initial bradycardia due to stimulation of C.I.C. (central effect) and blockade of presynaptic M receptors, followed by tachycardia due to block of M2 receptors. *large dose I.V. or orally it produce tachycardia from the start. *It A.V. conduction. *On blood vessels it has no effect in therapeutic doses as most of vessels have no parasympathetic supply (unninnervated M 3). However, toxic doses especially in children cause cutaneous V.D. especially in the face (Atropine flush). 5-GIT: Decrease motility and secretions. 6-Urinary tract: Relax wall and contract sphincters (urine retention). 7-C.N.S:. *Stimulate R.C. and C.I.C. *Inhibit vomiting centre and basal ganglia. *large doses on cortex produce excitation, agitation, hallucination and coma. Therapeutic Uses: a- Preanesthetic medication to: *Decrease salivary and bronchial secretions and prevent bronchospasm. *Antagonize respiratory center depressants. *Protect heart from bradycardia induced by some general anaesthetics. 16 *Prevent vomiting .But its disadvantages are urine retention and intestinal hypomotility following surgery. b- To measure errors of refraction in uncooperative patient (e.g. children). Also for fundus examination and to prevent formation of adhesions in iritis c- Heart block, marked bradycardia and carotid sinus syndrome. d- Bronchial asthma (but secretions become viscid so better use Ipratropium). e- Peptic ulcer, colics and gut hypermotility: In traveler's diarrhea, it is combined with diphenoxylate (opioid anti-diarrheal drug). f- Nocturnal enuresis and urinary urgency to reduce bladder motility. g. Parkinsonism. h. Motion sickness but hyoscine is better i- Hyperhidrosis (excessive sweating). j- Cholinergic poisoning to antagonize the muscarinic effects as in organophosphorus poisoning or physostigmine poisoning. Adverse Effects: Dry mouth, blurred vision, tachycardia, urine retention, glaucoma, flush and hyperthermia (especially in children). Contraindications: -Prostatic hypertrophy -Glaucoma. HYOSCINE = SCOPOLAMINE *It has a shorter duration with more potent effect on eye and secretions, but less effect on heart. *It is a tertiary amine as atropine, so stimulate R.C. and C.I.C. and inhibit vomiting centre and basal ganglia, also produces sedation & amnesia. 17 *Used as Atropine and preferred in preanesthetic medication of cardiac patients, in obstetric (with Meperidme to produce sedation and amnesia), in motion sickness, to abort vertigo in Meniere's disease, antispasmodic. Synthetic Atropine Substitutes 1-Mydriatic Group: Homatropine hydrobromide, Eucatropme, Cyclopentolate and Tropicamide. All of them produce cycloplegia except eucatropine. They are preferred over atropine in fundus examination and measuering errors of refraction. They are contraindicated in glaucoma. 2-Antisecretory Antispasmodic Group: They *Block M receptors especially on GIT. *They include: Probanthelene and Oxyphenonium and Hyoscine butyl bromide (Buscopan).They are used in peptic ulcer and colics. Pirenzepine and telenzepine are selective M1 blockers, used in peptic ulcer. *They are contraindicated in glaucoma and prostatic hypertrophy as Atropine. 3-Ipratropium and Tiotropium produce bronchodilatation without dryness of secretions. Given by inhalation in prophylaxis of bronchial asthma. 4-Anti-Parkinsonian group: Benzhexol= Trihexphenedyle, Benztropine and Caramiphen (which has also central antitussive action). 5-Emepronium: is similar to Probanthelene and used to reduce bladder motility in incontinence and nocturnal enuresis. * Tolterodine is M3 blockers for treatment of urinary incontinence. 18