* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Previous ectopic pregnancy.
Survey
Document related concepts
Menstrual cycle wikipedia , lookup
Dental emergency wikipedia , lookup
Reproductive health wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Menstruation wikipedia , lookup
Maternal health wikipedia , lookup
Birth control wikipedia , lookup
HIV and pregnancy wikipedia , lookup
Prenatal testing wikipedia , lookup
Prenatal development wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Miscarriage wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
Transcript
)5( عدد االوراق
نسائية
)(سيمنار
2012/9/3
Ectopic pregnancy
objectives
-What is ectopic pregnancy?.
-The patho-physiology of the ectopic gestation.
-Discussion of the cases interdused and the choices of
treatment that we have.
-the sequel of ectopic pregnancy.
An ectopic pregnancy, is a complication of pregnancy in which
the fertilized ovum implants outside the uterine cavity.
Classification of the ectopic pregnancy:1-tubal pregnancy
2-non tubal pregnancy
3-heterotopic pregnancy
4-persistant pregnancy
1
Ectopic pregnancy percentages of occurrence by location
Ampulla ectopic
75%_90%
Isthmic ectopic
5%_15%
Cornual/interstitial
1%_2%
Cervical ectopic
1%
Abdominal ectopic
0.3%_1%
How does the ectopic pregnancy happen
The sperm after ejaculation from the male travel from the vagina
,through the cervix, uterus and fallopian tubes where the
fertilization takes place . The fertilized egg will travel back to
reach the uterus. Most commonly the fertilized egg stops in the
fallopian tube and implants there result in an ectopic pregnancy.
The most common risk factor are:• History of pelvic inflammatory disease (PID) and Sexuallytransmitted diseases such as chlamydia and gonorrhea.
• Use of an intrauterine device (IUD).
• Previous pelvic surgery.
• Previous ectopic pregnancy.
• Advanced age.
• Unsuccessful tubal ligation or coagulation and tubal ligation
reversal.
• Use of fertility drugs.
• Infertility treatments such as in vitro fertilization (IVF).
• Congenital abnormality of the fallopian tube.
• Pelvic adhesion and pelvic tumor.
Symptoms of ectopic pregnancy
• abnormal vaginal bleeding.
• Lower abdominal pain.
2
•
•
•
•
•
•
Sharp abdominal cramps.
Pain on one side of the body.
Symptoms of pregnancy.
Dizziness or weakness.
Pain in the shoulder or the neck.
If the fallopian tube ruptures, the pain and bleeding could
be severe enough to cause collapse.
Case No. 1#
An 18 years old G2 P1 presents with abdominal pain and vaginal
bleeding slight in amount containing no clots for the past day.
last mc was 7 weeks ago
• She confirms that she is pregnant as she did urine
pregnancy test 4 weeks ago
• How would you deal with this condition?
From History taking
• She use an intra uterine device as a method of
contraception
• She did not have any pelvic surgery before nor sterilization
• She did not use ovulation induction
• She did not have history of PID
From physical examination
• The vital signs: BP was 120/70ml/hg
pulse rate was 90
her Temperature was 37.3c
• The abdomen is mildly tender with rebound
• Cervical motion tenderness is not present
From investigations
3
• Laboratory assessment: beta HCG measurement was 2200
mlU/ml
• The trans_vaginal ultrasound reveals an empty uterine
cavity
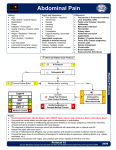
Diagnosing suspect ectopic after TVS
TVS
Trans vaginal
ultra sound
Ectopic pregnancy
Indeterminate u/s
No.
intrauterine
pregnancy
Measure beta HCG quantitative serum
level
1500mlU/ml or
greater
Less than
1500mlU/ml
Repeat after 48 hour
Consider surgical
consultation or diagnostic
uterine curettage
betaHCG not
increased at least
53%
4
Beta HCG
1500mlU/ml or
greater,patient is
stable
Active monitoring
• Done if there is:
1. Mild symptoms
2. Low level of beta HCG
3. Tubal location
4. Hemodynamically stable healthy woman
• Wait with follow up this is done by the B-HCG
in regular blood test and see if it is decline also monitor with the
U/S the ectopic pregnancy
The disadvantage: risk of tube rupture even if the B-HCG
shows low level
Methotrexate
• Done if the ectopic is less than 3.5cm
• Not suitable if there is:
1. Condition that decrease the immune system such as
diabetes
2. Blood disorder
3. Liver disease
4. Kidney disease
• The initial dose regimen(1mg/kg Im)
5
Monitor the B-HCG level, be aware of tube rupture
Follow up for 4_6 weeks
1. According to the dose as there is 2nd chance to develop
ectopic pregnancy
2. Avoid alcohol drinking.
Deferential diagnoses of abdominal pain in woman of
reproductive age are
• Pregnancy-related: Ectopic pregnancy, spontaneous abortion
• Gynecologic: Endometritis, pelvic inflammatory disease,
tuboovarian abscess, endometriosis, ovarian neoplasm,
ovarian torsion/rupture/hemorrhage, uterine fibroids.
• Non- Gynecologic : Appendicitis, bowel obstruction,
diverticulitis, IBD, UTI, pyelonephritis, nephrolithiasis.
Case No. 2#
• 38years old G10 P7 A2 at 8 weeks of gestation admitted to
the hospital with severe lower abdominal pain for 2 hours
and reports mild vaginal bleeding since 10 day ago
• Her BP was 90/65 ml/hg
• pulse rate was 106 b.p.m.
• Respiratory rate 20
6
• Temperature 37.4 c
Physical exam findings
• Enlarge uterus.
• Vaginal bleeding.
• Pelvic pain with manipulation of cervix.
• Palpable adnexal mass.
Rad flags for rupture ectopic pregnancy:
Significant abdominal tenderness , hypotension, Guarding and
rebound tenderness
• The first step we should do is to correct her vital signs by
establish an IV fluid for her
• Doing blood sample for investigation {CBC, cross
matching,CRP}
• Do TVS to determine the type of her pregnancy
Transvaginal gray-scale US image obtained along the longitudinal
axis shows an intrauterine pseudo–gestational sac (arrow); there
is no yolk sac or fetal pole. Free fluid is seen in the cul-de-sac (*).
Here the tube has been ruptured, and blood has collected in the
abdomen, then emergency surgery is needed. In these cases the
tube is often so badly damaged, that it has to be removed this is
done by salpingectomy
7
The sequel of ectopic pregnancy
1. In case of un rupture ectopic there is high risk of become
rupture and lead to deadly complication such as severe
bleeding.
2. 61% of cases with tubal pregnancy can conceive:
• 38% from them had at least one conception resulting in A
viable infant.
• 23% from them had recurrent Ectopic pregnancy.
3.Only 39% of cases become infertile especially after highly
damaged tube that it is one of the conditions that need (IVF).
What monitoring is needed in a second pregnancy
after ectopic pregnancy
• Any pregnancy after an ectopic needs to be carefully
monitored in the early stage to confirm the location
• After the missed menstrual period or positive pregnancy
test,blood HCG levels can be done to evaluate whether they
are rising at an appropriate rate
• By about 5_6 weeks of pregnancy TVS can be done to
confirm that there is gestational sac and yolk sac within the
uterine cavity
• If that is not seen by 6 weeks suspicion should be high for
another ectopic
Summary….
• Ectopic pregnancy incidence is about 1 every 60 population that
increase seriously with the risk factors.
• Ectopic pregnancy should take a good observation in order not
to develop any un wanted complication.
• Treatment of ectopic include active monitoring , medical (mtx)
and surgical that vary in uses according to the case present.
8
• Regular follow up after ectopic in the next pregnancy should
take place in order to
normal gestation.
diagnose early problem and ensure
Take home points
• The classic triad of ectopic pregnancy includes abdominal
pain , vaginal bleeding, and amenorrhea.
• Transvaginal ultrasound is the modality of choice when
diagnosing an ectopic pregnancy.
• With hCG level>1500mIU/mL and no IUP identified on
transvaginal ultrasound, this is high high-risk for ectopic
pregnancy.
• Transvaginal ultrasound is diagnostic if a true gestational
sac , yolk sac, embryo, or cardiac activity is found inside or
outside of the uterus
• Ectopic pregnancy is the leading cause of pregnancy related
death
References
• Bhatt, Shweta; Hamad Ghazale, Vikram S. Dogra.
Sonographic evaluation of ectopic pregnancy. Radiologic
clinics of North America. 45 (2007) 549-560.
• Derchi, Lorenzo E. et al. Ultrasound in gynecology. Eur
Radiol. (2001) 11:2137-2155.
• Doubilet, Peter M. & Carol B. Benson. Emergency Obstetrical
Ultrasonography. Seminars in Roentgenelogy, Vol XXXIII,
No 4(Oct), 1998: pp 339-343.
• Lozeau, M.D., M.S., Anne-Marie & Beth Potter, M.D.
Diagnosis and Management of Ectopic pregnancy. American
Family Physician. Volume 72, No 9; Nov. 2005.
• Nelson AL, DeUgarte CM, Gambone JC. Ectopic pregnancy.
In: Hacker NF, Moore JG, Gambone JC. Essentials of
obstetrics and gynecology, 4th ed. Philadelphia: Saunders,
2004: 325-333.
9
• Novelline, Robert A. Ultrasound imaging & Ectopic
pregnancy. Squire’s Fundamentals of Radiology. Sixth
edition. Pgs. 34-35 & 430-431.
• Toy, MD, Eugene C., Benton Baker, MD, MSC, Patti Jayne
Ross, MD, Larry C. Gilstrap, MD. Case Files: Obstetrics &
Gynecology. Pgs. 63-69, 211-218, 329-333.
• Yudin, MD, Mark H. MSc, FRCSC, & Harold C. Wiesenfeld,
MDCM. Current Diagnosis & Treatment of Sexually
Transmitted Diseases. Chapter 5: Lower Abdominal Pain in
Women.
10