* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immunizations for Kenya - Maseno Health Alliance
Survey
Document related concepts
Globalization and disease wikipedia , lookup
Poliomyelitis eradication wikipedia , lookup
Poliomyelitis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Plasmodium falciparum wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Mass drug administration wikipedia , lookup
Hepatitis B wikipedia , lookup
Vaccination policy wikipedia , lookup
Hepatitis C wikipedia , lookup
Typhoid fever wikipedia , lookup
Immunocontraception wikipedia , lookup
Whooping cough wikipedia , lookup
Polio vaccine wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Transcript
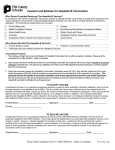
Immunizations Necessary for Travel to Kenya: ● ● ● ● ● ● ● ● Hepatitis A Hepatitis B Typhoid (oral) Malaria (oral prophylactic doses taken before, during, and after travel) Meningitis Tetanus Yellow Fever Polio booster (optional) Routine: Recommended if you are not up-to-date with routine shots such as, measles/mumps/rubella (MMR) vaccine, diphtheria/pertussis/tetanus (DPT) vaccine, poliovirus vaccine, etc. ● Tetanus booster needed every 10 years, a booster is required if you are unsure of last DPT vaccine Yellow Fever: CDC recommends yellow fever vaccination for all travelers ≥9 months of age. Kenya requires proof of yellow fever vaccination to enter the country. Vaccination should be given 10 days before travel and at 10-year intervals if there is ongoing risk. Most family practice healthcare clinics do not carry the yellow fever vaccine. Check with a travel health clinic or your doctor before scheduling your appointment. The CDC website also has lists of clinics providing the yellow fever vaccine. Hepatitis A and Hepatitis B: Recommended for all unvaccinated people traveling to or working in countries with an intermediate or high level of hepatitis A virus infection where exposure might occur through food or water. Hepatitis A can also be spread person-to-person. Vaccination Options: Combination Vaccine ● TWINRIX, manufactured by GlaxoSmithKline, is a combined hepatitis A and hepatitis B vaccine licensed for persons ≥18 years of age. ● Primary immunization consists of three doses, given on a 0, 1, and 6-month schedule, the same schedule as that commonly used for monovalent hepatitis B vaccine. ● An accelerated schedule of TWINRIX (i.e., doses at days 0, 7, and 21) for travelers has been approved by the FDA. A booster dose should be given at 1 year. Meningococcal (meningitis): Recommended if you plan to visit countries that experience epidemics of meningococcal disease. ○ Previous vaccine needed boosters every 5 years. ○ Menactra vaccine is good for a lifetime. Typhoid Recommended for all unvaccinated people traveling to or working in East Africa, especially if visiting smaller cities, villages, or rural areas and staying with friends or relatives where exposure might occur through food or water. Vaccination Options: ● Oral live vaccine-give in 4 doses, 48 hours apart. Vaccine taken 1-2 weeks prior to departure. Booster needed ever 5 years ● Intramuscular injections, 1 dose, booster needed every 2 years Polio (optional): Suggested for adult travelers who have received a primary series with either inactivated poliovirus vaccine (IPV) or oral polio vaccine (OPV). They should receive another dose of IPV before departure. Adults need only a single lifetime booster dose with IPV. Malaria: Antimalarial drugs are necessary for travel to Kenya. Talk with your doctor about which medication will be best for you. Some are taken as a daily dose, while others are on a weekly basis. Cost and side effects should be taken into consideration. Things to consider when choosing a drug for malaria prophylaxis: • Recommendations for drugs to prevent malaria differ by country and can be found on the CDC website. Note: Chloroquine is no longer effective in Kenya. • No antimalarial drug is 100% protective and must be combined with personal protective measures, (i.e., insect repellent, long sleeves, long pants, sleeping under a mosquito net). Anti-malarial drug options Atovaquone/Proguanil (Malarone) • Good for last minute travelers because the drug is started 1-2 days before traveling to an area where malaria transmission occurs • Taken daily • Good choice for shorter trips because you only have to take the medicine for 7 days after traveling rather than 4 weeks. • Very well tolerated medicine – side effects minimal • Cannot be used by women who are pregnant or breastfeeding a child less than 5 kg • Cannot be taken by people with severe renal impairment • Tends to be more expensive than some of the other options (especially for trips of long duration) Doxycycline • Taken daily • Good for last minute travelers because the drug is started 1-2 days before traveling, but it needs to be taken for 4 weeks after travel • Tends to be the least expensive antimalarial • If you are already taking doxycycline for a chronic infection (acne) you do not have to take an additional medicine. • Doxycycline also can prevent some additional infections (e.g., Rickettsiae and leptospirosis) and so it may be preferred by people planning to do lots of hiking, camping, wading and swimming in fresh water. • Cannot be used by pregnant women and children <8 years old • Women prone to getting vaginal yeast infections when taking antibiotics may prefer taking a different medicine • Persons planning on considerable sun exposure may want to avoid the increased risk of sun sensitivity • Most common side effect is stomach upset Mefloquine (Lariam) • Taken weekly, good choice for trips of longer duration • Not recommended for patients with certain psychiatric conditions or a history of depression • Not recommended for persons with cardiac conduction abnormalities • Not a good choice for last minute travelers because drug needs to be started at least 2 weeks prior to travel • Medication needs to be continued for 4 weeks after travel Primaquine • Good choice for shorter trips because you only have to take the medicine for 7 days after traveling rather than 4 weeks. • Good for last minute travelers because the drug is started 1-2 days before traveling to an area where malaria transmission occurs • Taken daily • Cannot be used in patients with glucose-6-phosphatase dehydrogenase (G6PD) deficiency • Cannot be used in patients who have not been tested for G6PD deficiency • There are costs and delays associated with getting a G6PD test done, however it only has to be done once. Once a normal G6PD level is verified and documented, the test does not have to be repeated the next time primaquine is considered. • Some people are concerned about the potential of getting an upset stomach from primaquine It is also recommended to get a prescription from your doctor for an antibiotic to treat traveler’s diarrhea, just in case. Typically ciprofloxacin or azithromycin are the best options, and are relatively inexpensive.