* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Prescribing and Therapeutics
Survey
Document related concepts
Transcript
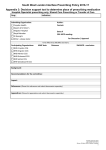
Prescribing and Therapeutics Dr L Varadhan C2017 Meeting – Doctor as Practitioner 1st June 2016 Agenda • Current teaching offered year-wise in hospitals • What is expected at the end of academic years • Broad overview of changes needed Y3 – What is being done • Introductory prescribing session – induction • Y3 pharmacology sessions – Increased familiarity with drugs in relation to clinical scenarios • • • • Block-based teaching Wrap-up session – include 10 drugs Sign off – 18 classes of drugs Handbook changes Y3 Handbook MISTIME Categories Explanation Mode of action Broadly what class Indications Common clinical indications, drug of choice, contraindications Side-effects Common expected side effects; major adverse reactions Therapeutic evaluation In context of the medical issue (stop/start/ withhold/ reduce/ continue), renal and hepatic function, planning for pregnancy, etc. Interactions With other used drugs, affect on metabolism Monitoring If required; and how; for drug levels; for side effects Education Patient information, timing, dietary changes, monitoring, alcohol Y3 Handbook Y3 Handbook Expectations - At end of Y3 • Familiarity with common classes of drugs – basic pharmacology profile: name and class of drug, mechanism of action, indication and contraindications • Taking a good and comprehensive drug history – Including alternative and OTC medications • Approach a drug chart and able to identify the drugs, indications, side effects (MISTIME) • Good familiarity with BNF Y3 – What needs to be done • Gap between Y2 and Y5 with respect to drugs and prescribing • Pharmacology/therapeutics teaching to be spread across the year – CBL tutor training • CBL – to include discussion on drugs • Continued familiarity with drugs – all tutors • Others – Classes of drugs aligned to BNF criteria – Consolidation prescribing session as part of Keele Spine – Antibiotic prescribing session • SCRIPT access and PSA introduction Y4 • Y4 prescribing workshops • Y4 pharmacology session – Reduce number of cases of therapeutic evaluation – Slide presentation to give more direction and structure • Block-specific teaching – ID team: lecture at Keele Spine on TB and HIV drugs – O&G: Contraception • Sign-offs on the log books Y4 Handbook Y4 handbook Expectations at end of Y4 • Familiarity with most of the drugs – Understand monitoring for effect and side-effect – Able to identify a wrongly written drug • Understand interactions of drugs • Therapeutic evaluation of a drug chart – Tailored to patient clinical condition Y4- what needs to be done • Y5 content to be started in Y4 • CIL presentations to include drug lists – Tutor and student notes to include this • Prescribing and therapeutics teaching should be embedded across the year – Block Leads and Firm tutors • Introduction to SCRIPT access • Limited SOP for Y4 prescribing in hospitals • Introduction to PSA and Mock exam Y5 Prescribing • SOP – Hospital prescribing – ‘Purple pen’ prescribing – Student assistantship programme • SCRIPT access and usage • Assistantship – Constituting and administration of drugs Y5 • • • • • Session 1: Prescribing skills Session 2: Diabetes cases Session 3: Therapeutic evaluation Session 4: Delivered in GP Pharmacist and diabetes nurses involved Y5 • Induction day at RSUH/SaTH safe prescribing lecture • GP away day – Day 1:Death certification & PSA exam – Day 2: IV fluid prescribing & prescribing – renal and gentamicin prescribing • EOL prescribing – Delivered at hospice – Orientation to PRN/syringe driver prescribing of EOL meds Y5 – Pharmacist teaching • Session 1: Prescribing safety ( at beginning of the block) • Session 2: (mid) – TTO and discharge letters • Session 3: (mid) – Heparin/ warfarin and NOAC therapy Expectations at Y5 completion • Being a safe and effective prescriber • Feeling confident to start prescribing as F1 • Broad knowledge of various drugs, therapeutic issues, guidelines and evidence base – Assess risk vs benefit • Pass the PSA exam/summative assessment Y5 -What needs to be done • SCRIPT – increase uptake – Changes to induction session – ?make mandatory • PSA in January/February – Completion of teaching for GP and Hospital Block by then – Changes to the presentation materials – Renal prescribing, therapeutic evaluation, TTO • Assistantship – Continued emphasis on drug review and prescribing – Few sessions with the pharmacist on ward round? • Uniformity at SaTH and UHNM General issues • • • • • RIME model Cross delivery across various sites - hospitals/GPs Tutor awareness Signposting of pharmacology and therapeutics Y3 gap in pharmacology – Vertical integration in Y3 curriculum • Y5 duration before PSA