* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ethics and Human Subject Issues in Research: Informed Consent
Survey
Document related concepts
Transcript
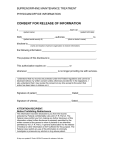
Human Subject Issues in Research: Informed Consent Jill M. Baren, MD What is Ethics? The study of standards and conducts and moral judgment The system or code of morals of a particular person, religion, group, or profession Identifying Ethical Issues Write down 2 ethical issues, problems or questions that you have encountered since becoming an academic associate How were they resolved? Did you feel the resolution was satisfactory? INFORMED CONSENT What is it? Why do we need it? From whom do we get it? How do we get it? How can we be sure we’re doing it right? Informed Consent What it’s not A legal document A risk management tool for an investigator or an institution A formality What it is A Process Acknowledging respect for persons (Autonomy) Goal “The goal of the informed consent process is to provide people with sufficient information so they can make informed choices about whether to begin or continue participation in clinical research.” The process “…involves a dynamic and continuing exchange of information between the research team and participant throughout the research experience…” The document “…a starting point for the necessary exchange of information between investigator and potential participant.” “…the foundation not the entirety…” Why do we need it? Respect for persons Respect for autonomy of decision making True limit on investigative authority Sense of formality Historical Perspective Research ethics policies From singular events and the reactions to them Rarely proactive Sentinel events Nazi war crimes Human radiation experiments, etc. Tuskegee Syphilis study Nuremberg trial (1948) Declaration of Helsinki (1963) National Commission Belmont Report (1977) Nuremberg, Germany December 9, 1946 to August 20, 1947 Required voluntary consent prior to participation Investigator responsibility to obtain consent Information gained by using human subjects would be unprocurable any other way Declaration of Helsinki (World Medical Association) Articulated ethical principles for use by physicians conducting human research Affirmed the autonomy of the individual Universally adopted to ensure the rights and welfare of human subjects of research Tuskegee Syphilis Study Post- Tuskegee Events National Research Act 1974 National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research Belmont Report Ethical foundation for US federal regulations on human subjects research Belmont Report 3 basic principles that should govern all research involving human subjects Respect for persons Beneficence (maximize benefits, minimize risks, avoid harm) Justice (benefits and burdens equally distributed) Federal regulations (DHHS) 1991 Federal Policy for Protection of Human Subjects (The Common Rule) Adopted by all agencies which conduct, supervise, regulate, fund or sponsor human research Two major requirements: Informed Consent IRB approval What does someone need to know? Disclosure (what’s going to happen) Risks Benefits Alternatives Confidentiality Compensation “It’s a very simple procedure. We slice off the top of your head, scoop out your innards with a spoon, and carve out your eyes and mouth.” Standards for Disclosure Subjective “The reasonable volunteer” Are we doing it right? Voluntariness: Freely coming to a decision Free from coercion or undue influence Assumes capacity Capacity Understand nature and ramifications Who is not able to do this? Vulnerable populations Children ? Prisoners? Mentally retarded individuals Dementia/Coma/Vegetative state Mental illness Pregnant women Emergency patients? (pain, fear, etc.) Vulnerable Populations: Children If child can understand (> age 6-8) We are obligated to obtain assent Can parents overrule? In studies with more than minimal risk and not without prospect of direct benefit Other vulnerable populations Research on individuals who lack capacity also requires prospect of benefit Not promulgated in federal regulations Family member can consent If consistent with state law How do we get informed consent? Will vary according to study design and nature of participation Verbal vs. Written Investigator vs. proxy Are we doing it right? Behaviors during informed consent (>1000 ED patients taking a survey) 41% did not read 57% who read spent < 60 seconds 22% asked questions 44% did not accept the form Informed consent behaviors No relationship with gender, education, marital status, or self-reported health status We need to do better to correct these behaviors Baren et al: AEM May 2000 Informed consent gone wrong? Jesse Gelsinger (gene transplant) James Quinn (artificial heart) Johns Hopkins (hexamethonium death) Gene therapy business: “The tragic case of Jesse Gelsinger” 18 year old with partial ornithine transcarbamylase deficiency Usually fatal in infancy The first person to die from gene therapy Reactions FDA suspended all gene therapy trials and other experiments Hearings on quality of oversight and safety President Clinton demanded improvements in consent and access to information about gene therapy research James “Butch" Quinn: Artificial Heart Recipient 52 year old who received the Abiomed heart Lived for 10 months with the device Sustained fatal stroke Reactions Lawsuit over consent process Recipient's widow says she and her husband were misinformed and misled on risks, benefits and the potential for pain and suffering “There was no quality of life. It was too painful. He said he wished he'd never done it." Was it wrong? 13-pages detailing "significant risks" stroke, brain and organ damage, discomfort and pain. “New and experimental operation” Complications could occur (previously unknown or unforeseen) Potential benefits “uncertain and not proven” Volunteer in Asthma Study Dies After Inhaling Drug 24 hours after inhaling hexamethonium reported dry cough, shortness of breath, muscular aches and fever 2 days later admitted with concern for possible reaction Died one month later Reactions Research suspended Federal government temporarily shut down most research involving human subjects at JHU Hexamethonium not approved by the FDA and IRB did not provide adequate oversight Healthy volunteers Volunteers may not stand to benefit directly, but could ultimately contribute to development of a new therapy that the participant might then use. Require particularly close monitoring, because they can pose a risk to a volunteer's health or life. Why do people participate in biomedical research? Altruism Free medical care and medications Trust Self-interest Attention Do we want to constrain people if they are doing things for the wrong reasons? “A motion has been made and seconded that we stick our heads in the sand.” Role of the IRB Protect the institution Can introduce complexity Responsibility of PI to terminate if they sense the patient is not really involved in the process No one knows how risk is really determined How can we make it better? Start with the document Finish with the process Discussion Current studies Ethical issues Your opinions?