* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Orientation for the Nursing Student
Survey
Document related concepts
Transcript
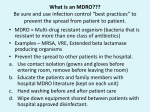
Self Orientation requires a review of the same information that all new Tenet employees review. You are responsible for reading all information contained on the CD (or in the binder). Please follow these instructions: Read through all sections on the CD (or in the orientation binder) and complete the quiz enclosed in the “Forms” folder. After completion, return to the Human Resource Department with all other forms. All employees will read and sign the “Confidentiality Statement” and “Statement of Responsibility” forms, Return with the completed quiz to the Human Resource Department. ID badges will be made in the HR department at the completion of the orientation. HIPPA Training • Click on the link below to complete the training. At the end of the video, complete the post test, print and turn in with other tests. • Tenethealth.com at: http://www.tenethealth.com/about/pages/Informati onPrivacySecurityandHIPAATraining.aspx CULTURAL APPRECIATION Cultural Competency in Healthcare Settings Topics to Be Covered • What is Diversity? • Our Business Case for Diversity • Values and Beliefs • Diversity Initiatives • Celebrate Diversity What is Diversity? • The differences that make each of us unique. • In the past, our country was the great melting pot; we were expected to blend together. • Today, we’re a mosaic- accepting each others differences • Culture- the values, beliefs and practices shared by a group. Our Business Case for Diversity • Awareness of cultural factors can improve patient and family education – one area of focus for the Joint Commission survey. • Meet our community needs. Our community is diverse. • Make sure patients get the best possible care. Take their cultural views on health into account; they will respond better to care. What does population change mean for us? • Make up of patients change. • Make up of workforce change. • Services rendered to patients change. Values and Beliefs Treat each patient as an individual: • Avoid stereotyping. • Consider other factors that may affect care such as age. • Learn about each patient’s unique views on health care. • Know your own cultural beliefs and practices. • Know how to show politeness, how often to seek medical care and appropriate ways to treat children or older people. Values and Beliefs Be aware of cultural factors: • Country of origin. How long a person has lived here may affect his or her views toward health • Preferred language • Communication Style. A person’s culture may affect how he or she expresses pain. • Religion • Food preferences • Family relationships Values and Beliefs Take time to learn about each patient: • Ask questions to avoid cultural stereotypes. Differences exist among members of the same group. • Learn the patient’s views about health. • Show respect. Ask how a patient would like to be addressed. • Consider privacy needs. • Use interpreters effectively Diversity Initiatives • Interpreters Available - AT&T Language line available 24/7 contact unit supervisor or overhouse supervisor for assistance • Chaplin Available 24/7 • Patient Rights and other medical information both in English and Spanish. • Community outreach for everyone, but have targeted initiatives based on the needs in our community. • Community Advisory Boards Diversity Initiatives Spalding Regional Medical Center’s Diversity Standard We recognize and respect the cultural, physical and social differences among our employees, patients and visitors. We realize that each of us comes from a different background and brings a range of talents and opinions that enrich our environment. We mirror the community we serve and strive to appreciate our differences. Diversity Initiatives Spalding Regional Medical Center’s Diversity Guidelines: • Take the time to better understand coworkers and customers. • Discourage jokes and negative comments about race, religion, color, national origin, disability, gender and age. • Do not discriminate against patients, customers or other employees on the basis of race, religion, color, national origin, disability, gender or age. Celebrate Diversity! • Take pride in your own uniqueness. • Welcome others as individuals with special qualities. • Enjoy your similarities and your differences. Communication and Team Dynamics Three components of a team are: •Team Mission Statement: a simple statement of purpose known by every member of the team which provides a “reason for being” •Team Vision Statement: expresses the destination of the team in a way that builds commitment to it •Team Success Criteria: specific and measurable criteria that lets you know when you have achieved what you set out to do Team Member Selection A successful team requires individuals to combine different abilities into a cohesive unit which is able to achieve tasks beyond the capabilities of its members. The Innovator – produces new ideas and strategies The Coordinator – directs the group, maintains control and direction of the discussion The Investigator – is knowledgeable of available resources, researches ideas and determines what can be done The Evaluator – weighs the facts, considers the pros and cons of each option The Shaper – highly motivated and are excellent at sparking life into a team The Worker – good communicator who helps reduce tension in the group by promoting better co-operation among team members. The Finisher – an organizer who ties up loose ends during the final stages of implementation The Implementer – concerned with detail, capable of directing others, can be depended on to carries out the final details Characteristics of Good Team Building - High level of interdependence among team members - Team leader has good people skills and is committed to a team approach - Each team member is willing to contribute - Team develops a relaxed climate for communication - Team members develop a mutual trust - Team members are prepared to take risks - Team is clear about goals and established targets - Team member roles are defined - Team members know how to examine team and individual errors without personal attacks - Team has the capacity to create new ideas - Each team member knows he/she can influence the team agenda Resolving Conflict Conflict is inevitable, natural, and even healthy. What is unhealthy is unresolved conflict that is allowed to affect an otherwise productive team. When conflict arises explore each team member’s position thoroughly. Consider your own as well as your team member’s position keeping in mind that the conflict may be about personalities and needs rather than the subject matter. Approach possible solutions together through collaboration. Build for your team a feeling of oneness, of dependence upon one another and of strength to be derived by unity. Vince Lomabardi Infection Control Clinical Orientation Spalding Regional Medical Center Isolation Practices… You are expected to set the example for others (non-licensed, families, guests) STANDARD Precautions CONTACT Precautions DROPLET Precautions AIRBORNE Precautions CONTACT precautions: Put gown and gloves on BEFORE entering room Remove gown and gloves JUST BEFORE leaving room and discard INSIDE room Perform hand hygiene when leaving room Disposable stethoscopes, thermometers, BP cuffs ONLY!! DO NOT use your own stethoscope DROPLET precautions: Droplets are large (>5 micrometers) and heavy; they settle on horizontal surfaces usually within a few feet of the point of aerosolization (coughing, sneezing, talking, singing) SURGICAL mask needs to be worn when entering the room (NOT N-95) Obtain a new mask each time you enter the room DO NOT wear mask outside of the room AIRBORNE Precautions How Swine Flu is contracted AIRBORNE precautions: Requires use of N-95 respirator Must be fitted for this respirator by Employee Health Nurse Provides protection from tiny particles (<5micrometers) that stay suspended in air and travel on air currents for long distances YOU MUST DO A FIT CHECK EVERY TIME YOU DON THIS RESPIRATOR (and before you enter the room) Door to room must remain CLOSED! (No exceptions) Room must be under negative pressure You must notify Engineering to check negative pressure BEFORE patient is admitted into room; they will check it every day thereafter You may use the respirator multiple times during a shift, unless it becomes soiled with blood or body fluid, if it becomes moist, or you can no longer achieve an occlusive seal when you fit-check it SCIP=Surgical Care Improvement Project “CATS” CATS, continued CLIPPERS -never RAZORS ANTIBIOTICS -give the correct antibiotic for the type of surgery -administer the first dose within 60 minutes of the incision time -stop the antibiotic within 24 hours of the close time of surgery TEMPERATURE -maintain the patient’s core temperature at or above 96.8 degrees SUGAR -maintain normoglycemia of cardiac surgery patients Surgery and Foley Catheters… Foleys MUST be removed within 48 hours of a surgical procedure unless the MD gives the specific written rationale why it must be kept. Exceptions: -OBGYN -urologic, perineal -intermittent catheterization prior to surgery or who had Foley prior to admission -ICU patient on diuretics NPSG’s………….2010 Lucky “7” ---- Infection Prevention Reduce the risk of Healthcare Associated Infections 07.01.01—Hand Hygiene 07.03.01—Prevent MDRO infections 07.04.01—Prevent ClaBSIs 07.05.01Prevent SSIs Manage as sentinel events all cases of unanticipated death or major permanent loss of function related to a healthcare associated infection Central Line BUNDLE Meticulous Hand Hygiene Maximal Barrier Precautions Chlorhexidine Skin Antisepsis Optimal Site Selection Daily Review of Line Necessity Ventilator Associated Pneumonia Bundle Maintain HOB @ 30-45 ° at all times Daily Sedative Interruption PUD Prophylaxis VTE Prophylaxis Foley catheter best practices Hand Hygiene Maintain sterile system—no breaks Maintain surgical asepsis on insertion Maintain bag below level of bladder No kinking or looping of tubing Maintain use of Stat-Lok Device to prevent tension, traction Remove Foley as soon as possible! STAFF EDUCATION: Your Role in Preventing the Spread of Multiple-Drug Resistant Organisms (MDROs) Cheryl Kirchner, RN, BSN, MS National Director, Clinical Quality Improvement July 2009 Tenet’s goal is to stop the spread of infections in our hospitals. Everyone is needed to help. Healthcare-associated infections (HAIs) • Infections that patients acquire during the course of receiving treatment for other conditions within a healthcare setting. • Variety of causes, including (but not limited to): – the use of medical devices, such as catheters and ventilators – complications following a surgical procedure – transmission between patients and healthcare workers – antibiotic overuse • Risk for all hospitalized patients. Source: CDC website http://www.cdc.gov/ncidod/dhqp/healthDis.html Healthcare-associated infections are one of the top ten leading causes of death in the United States. In American hospitals alone, healthcare-associated infections account for an estimated… • 1.7 million infections each year – Most (1.3 million) were outside of intensive care units – 9.3 infections per 1,000 patient-days – 4.5 infections per 100 admissions • 99,000 associated deaths each year – 32% of all HAI are urinary tract infections. – 22% are surgical site infections. – 15% are pneumonia (lung infections). – 14% are bloodstream infections. Source: Klevens, Edwards, Richards, et al. Pub Health Rep 2007; 122:160-6 What is an MDRO? Multiple Drug-Resistant Organisms (MDROs) are bacteria and other germs that have developed resistance to antibiotic medications such as penicillin and amoxicillin. Examples of MDROs • MRSA (Methicillin-resistant Staphylococcus aureus) – Two types: Hospital-acquired and Community-acquired – Most infections caused by staph are skin infections, but staph also can cause more serious infections such as blood and joint infections, and pneumonia. Skin infection may appear as a spider bite that will not heal. • VRE (Vancomycin-resistant Enterococci) – Infection can lead to diseases of the urinary tract, bloodstream, heart valves (endocarditis) and brain (meningitis), as well as to serious infections in open wounds. • Drug-resistant TB (Tuberculosis) – TB can cause infection in the lungs or other parts of the body. • C. diff Clostridium difficile is a toxin-producing bacteria. – C. diff can result in diarrhea that turns into colitis. Sources for pictures: mrsasymptomsinfo.com; mrsadiagnosis.com/mrsa-basics/ Examples of MDROs • Drug resistant Staphylococcus aureus "Staph" Infections – MRSA (Methicillin-resistant Staphylococcus aureus) • HA-MRSA (Healthcare-Associated MRSA) • CA-MRSA (Community-Associated MRSA) – VISA/VRSA (Vancomycin-Intermediate/Resistant Staphylococcus aureus) Source: CDC; JAMA. 2006;295:269-270 ; IHI.ORG Examples of MDROs Other drug-resistant organisms – VRE (Vancomycin-resistant Enterococci) – ESBL Gram negative bacteria that produce extended spectrum beta lactamase enzymes, which result in resistance to most antibiotics. • K. pneumoniae (Klebsiella pneumoniae) • Acinetobacter • S. pneumoniae (Streptococcus pneumoniae) – Drug-resistant TB (Tuberculosis) – C. diff Clostridium difficile is a toxin-producing bacteria. – K oxytoca (Klebsiella oxytoca) – E coli Impact of MDROs in the Health Care System • Infections caused by MDROs are associated with worsened clinical outcomes, including an increased risk of death • MDRO infections also are associated with significantly increased costs to hospitals, mostly attributable to increased lengths of stay. • Media, legislative and regulatory pressures are compelling hospitals to more effectively control MDROs Legislative Pressure: Many states have laws regarding reporting of hospital acquired infections. Check this hyperlink to see if your state does: http://www.apic.org/scriptcontent/custom/dyncontent/le gislation/index.cfm?section=government_advocacy Regulatory Pressure: No additional payment for selected hospital acquired conditions that are not present on admission. Centers for Medicare & Medicaid Hospital Inpatient Prospective Payment Systems Final Rule effective on October 1, 2008 Selected hospital acquired conditions include: Catheter-Associated Urinary Tract Infection (UTI) Vascular Catheter-Associated Infection Surgical Site Infection Mediastinitis After Coronary Artery Bypass Graft (CABG) Regulatory Pressure: National Patient Safety Goals (NPSG) 2009 Goal 7 – Reduce the risk of health care-associated infections. A. Meet Hand Hygiene Guidelines (NPSG.07.01.01) B. Report Sentinel Events Resulting from Infection (NPSG.07.02.01) C. Prevent Multi-Drug Resistant Organism Infections (NPSG.07.03.01) D. Prevent Central-Line Associated Blood Stream Infections (NPSG.07.04.01) E. Prevent Surgical Site Infections (NPSG.07.05.01) MDROs are a Growing Problem • MDRO infections among hospital patients have continued to rise, despite widespread efforts to control their spread. – • MDROs are being seen even among patients in the community. Two main factors drive the spread of MDROs 1. Overuse and misuse of antibiotic medications. 2. Cross-transmission between patients in healthcare settings. Persons at Risk for an MDRO Infection • Persons with low immune systems, severe illness or disability, chronic illnesses that are difficult to treat and get worse over time (for example, kidney failure or cystic fibrosis) • Persons being treated for burns or persons with open wounds or surgical wounds (especially in the belly or pelvic area) • Persons with invasive medical equipment (for example, tracheotomy tubes or implanted catheters) • Persons with long or repeated hospital stays, especially if they are often treated with antibiotics • Persons who do not finish all of the antibiotics prescribed by their doctors MDRO Colonization and Spread • Colonized patients carry MDROs with no signs of infection. – Colonization generally comes about through spread of MDROs from patient to patient and is often a precursor to later infection. • Both colonized and infected patients can be the source of spreading MDROs to others through – The animate environment (e.g., hands) – The inanimate environment (e.g., equipment) – A combination of the animate and inanimate environment Tenet’s Two-Fold Approach to stop the spread of infections in our hospitals. • First, we must continue to improve the culture for hand hygiene, making the message simple and direct. • Second, we must intervene to prevent the spread of infection when people are admitted to a hospital or visiting patients in the hospital. MDRO Cycle of Transmission • Intervention must occur to break the cycle of transmission from organism to host (patient), host (patient) to environment, environment to healthcare worker and healthcare worker transmitting the organism. • Source control at the patient level and point of care control at the healthcare worker level are essential to success. • Ensuring and maintaining clean hands and environment are the basic building blocks of this program. MDRO Cycle of Transmission ORGANISM HOST HEALTHCARE WORKER ENVIRONMENT MDRO Cycle of Transmission ORGANISM Who can spread the organism? HEALTHCARE WORKER All persons who touch the patient. HOST Patient ENVIRONMENT All persons who touch the patient’s surroundings. Source control at the patient level and point of care control at the healthcare worker level break the cycle of transmission. ORGANISM HOST Source Control Antibiotic Stewardship Community Outreach Source Control Clean Hands Active surveillance Targeted decolonization Antibiotic Stewardship HEALTHCARE WORKER ENVIRONMENT Point of Care Control Clean Hands Isolation Precautions Prevention Bundles Point of Care Control Clean Environment: Decontamination of environment and equipment Breaking the cycle of transmission involves EVERYONE on the TEAM! The Program Plan to Break the Cycle of Transmission is a Team Effort. PROGRAM PLAN TASKS • Identify patients at risk for MDRO Nursing • Staff Education regarding MDRO prevention Hospital Educators • Patient / Family Education regarding MDROs Case Managers (Reminder: “If it is not documented, it is not done.”) • MDRO Surveillance INDIVIDUALS WHO ARE INVOLVED Infection Preventionists • Decontamination of environment and equipment Plant Operations • Targeted decolonization Environmental Services • Antibiotic Stewardship Laboratory / Microbiologists • Isolation Precautions Pharmacist • Prevention Bundles Dietary Services • Implement a laboratory alert system for patients who have an MDRO Materials Management • Measure and monitor MDRO prevention processes Information Technology • Communicate results with key stakeholders Administration, Physicians Quality Management The Program Plan to Break the Cycle of Transmission is a Team Effort. PROGRAM PLAN TASKS • Identify patients at risk for MDRO Nursing • Staff Education regarding MDRO prevention Hospital Educators • Patient / Family Education regarding MDROs Case Managers (Reminder: “If it is not documented, it is not done.”) • MDRO Surveillance INDIVIDUALS WHO ARE INVOLVED Infection Preventionists • Decontamination of environment and equipment Plant Operations • Targeted decolonization Environmental Services • Antibiotic Stewardship Laboratory / Microbiologists • Isolation Precautions Pharmacist • Prevention Bundles Dietary Services • Implement a laboratory alert system for patients who have an MDRO Materials Management • Measure and monitor MDRO prevention processes Information Technology • Communicate results with key stakeholders Administration, Physicians Quality Management COMMUNICATION Has this patient been screened for MRSA? How many patients have an MDRO? Is this patient infected with an MDRO? Does this room need special cleaning? Do I need to wear protective clothing? Were the antibiotics discontinued? Patient / family MDRO education completed? Did the patient wash his / her hands? COMMUNICATION Verbal Speak up! • Confirm with co-workers (that means everybody, including physicians) that hands are clean, environment is clean, prevention measures have been followed, etc. • Ask patients if their hands are clean. Written Pay attention! Electronic • Automatic alerts on the computer, laboratory result reports, etc. • Reports for directors and administrative staff that help with staffing, cleaning plan, etc. • Isolation Signs • Physician Orders • Notes on patient charts • MDRO Flag on the Patient Face Sheet • Reports that are posted to track compliance with prevention measures Center for Disease Control and Prevention (CDC) Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Targeted plan for physicians 1. Prevention Infection Step 1. Vaccinate Step 2. Get the catheters out 2. Diagnose and treat infection effectively Step 3. Target the pathogen Step 4. Access the experts 3. Use antimicrobials wisely Step 5. Practice antimicrobial control Step 6. Use local data Step 7. Treat infection, not contamination Step 8. Treat infection, not colonization Step 9. Know when to say “no” to “vanco” Step 10. Stop antimicrobial treatment 4. Prevent transmission Step 11. Isolate the pathogen Step 12. Break the chain of contagion Source: http://www.cdc.gov/drugresistance/healthcare/default.htm Individual Actions to Prevent the Spread of MDROs Everyone, Every time • Clean Hands • Clean Environment When Indicated • Isolation precautions • Active surveillance for MDROs • Targeted decolonization of patients • Prevention Bundles • Antibiotic Stewardship Clean Hands These images illustrate the critical importance of hand hygiene in caring for patients, including those not known to carry antibiotic-resistant pathogens. An imprint of a health care worker's ungloved hand after the worker had performed an abdominal examination of a patient. After the worker's hand had been cleaned with alcohol foam, another hand imprint was obtained, and the resulting culture was negative for the MDRO. Source: Donskey and Eckstein NEJM 360 (3): e3, Figure 1 January 15, 2009 http://content.nejm.org/cgi/content/full/360/3/e3/F1 Clean Hands Your 5 Moments for Hand Hygiene More information: http://www.who.int/gpsc/5may/background/5moments/en/index.html Clean Hands Soap and Water Alcohol-based Handrub If hands are visibly dirty, wash with soap and water. If hands are not visibly dirty, use an alcohol-based hand rub. 1. Wet hands and apply soap. 2. Rub hands together for 15 to 20 seconds and make a lather. 3. Rinse hands well. 4. Dry hands using a paper towel or air dryer. If possible, use your paper towel to turn off the faucet. 1. Apply product to the palm of one hand. 2. Rub hands together for 15 to 20 seconds. 3. Rub the product over all surfaces of hands and fingers until hands are dry. Total Process time: 40-60 seconds Total Process time: 20–30 seconds Alcohol-based hand rub is: • more effective • faster • better tolerated Always use SOAP AND WATER to clean hands when caring for C. difficile patients or patients having diarrhea. What is Clostridium difficile? • Clostridium difficile (C. difficile) is a bacterium that is related to the bacterium that cause tetanus and botulism. • The C. difficile bacterium has two forms, an active, infectious form that cannot survive in the environment for prolonged periods, and a non active, "noninfectious" form, called a spore, that can survive in the environment for prolonged periods. • Although spores cannot cause infection directly, when they are ingested they transform into the active, infectious form. Source: www.medicinenet.com/clostridium_difficile_colitis/article.htm Clean Hands at the POINT OF CARE Point of care – refers to the place where three elements occur together: (1) the patient, (2) the health-care worker and (3) care or treatment involving patient contact (within the patient zone) • This requires that a hand hygiene product (e.g. alcohol-based handrub, if available) be easily accessible and as close as possible (e.g. within arm’s reach), where patient care or treatment is taking place. • Point of care products should be accessible without having to leave the patient zone. Patient Zone Clean Hands? It is an expectation of Tenet and part of being a true patient advocate Kindly remind ANYONE who does not clean their hands properly to do so. to question physicians, coworkers, other staff and visitors if they have clean hands. Clean Environment • Environmental hygiene is aimed at eliminating the reservoir of MDROs on hospital surfaces and equipment. – MDROs can persist in the environment despite routine cleaning practices – Some MDROs can remain for weeks without proper surface disinfection. – Patients admitted to rooms previously occupied by a patient with an MDRO are at higher risk for developing infection with that MDRO. Clean Environment ROOM LOOKS CLEAN BUT … the X represents MDRO culture positive sites Source: The Risk of Hand and Glove Contamination after Contact with a VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL. Clean Environment • Nearly ¾ of surfaces in patients rooms are contaminated with an MDRO. – Examples of high-touch surfaces include door knobs, bed rails, telephones, light switches, bedside tables and curtains. Once caregivers touch these surfaces, their hands or gloves are contaminated. Source: Infection Control and Hospital Epidemiology (v. 9, 1997) 622-627. The Environmental Services (EVS) Team is CRITICAL! Everyone can pitch in… It is recommended that all patient equipment be disinfected with antibacterial wipes before and after patient use. • Physical Therapists should disinfect patient equipment, such as walkers, crutches and common areas that patients come into contact with, including stairs and handrails. • Transportation Services should disinfect wheelchairs, stretchers, etc. • Nurses/Aides/Techs should disinfect patient equipment, such as blood pressure cuffs, commodes, etc. • Physicians and Nurses should disinfect non-invasive instruments such as stethoscopes, hemostats, etc. Clean Environment • All objects that come in contact with patients should be considered as potentially contaminated. • Cleaning and disinfecting high touch surfaces is essential to the health of hosptial patients, visitors and healthcare workers. Appropriate disinfectant + Adequate contact time + Friction = Good Cleaning • Be sure to READ THE INSTRUCTIONS on cleaners and FOLLOW THE MANUFACTURER’S GUIDELINES for product use and maximum disinfecting. Isolation Precautions Isolation Precautions • Be aware of possible effects of isolation on patients: – Patient perceptions of depression and anxiety; – More preventable adverse events (e.g., pressure ulcers); – Patient dissatisfaction with treatment. • Recommended actions when patients are placed on Contact Precautions: – Make a point to enter the room to assess the patient for • increased anxiety and/or depression • preventable adverse events related to immobility – Be sure to document assessments Source: CDC/HICPAC MDRO Guidelines, p. 26; http://www.cdc.gov/ncidod/dhqp/pdf/ar/MDROGuideline2006.pdf Isolation Precautions Gloves and other personal protective equipment (PPE) should not be worn in public areas. Gloved hand touching elevator button Gloved hand touching wheelchair Gloved hand touching cell phone Gloved hand touching computer Personal Protective Equipment (PPE) also NOT A FASHION STATEMENT. Isolation Precautions Transportation of Patient In Isolation Contact - Enteric Contact Airborne Droplet • Cover patient with • Cover patient with • Put mask on sheet / blanket sheet / blanket patient • Put mask on patient • Notify receiving personnel • Notify receiving personnel • Notify receiving personnel • Notify receiving personnel • No gowns or gloves with transport. • No gowns or gloves with transport. • Limit transport • Limit transport 1. Remove and dispose of contaminated PPE and perform hand hygiene prior to transporting patient. 2. Wear clean PPE to handle the patient at the transport destination. Sources: http://www.cdc.gov/ncidod/dhqp/gl_isolation_contact.html http://www.osha.gov/SLTC/etools/hospital/hazards/ppe/ppe.html Take clean PPE to the transport destination. Other Possible Infection Control Steps • Grouping of patients • Grouping of staff • Use of designated beds or units for patients with MDROs • Unit closure (rare) Other Possible Infection Control Steps • Check patients who are most likely to have harmful bacteria on their skin to determine appropriate precautions and/or treatments. • Specially treated cleansing cloths, which target harmful staph bacteria, can be used by patients before surgery to reduce the risk of infection. • Ensure specific prevention measures are in place for patients who have medical devices, such as intravenous tubes, breathing tubes or urinary catheters. • Antibiotic stewardship involves avoiding overuse and ensuring the best choices are made when selecting and giving antibiotics to patients. Active surveillance for MDROs • Active surveillance for MDROs is designed to identify patients who are colonized but not overtly infected with MDROs – Swab samples from the nose, rectum, or other body sites can be examined in the lab to detect specific MDROs. – By identifying these individuals, measures can be taken to prevent the spread to other patients. – Active surveillance has been shown to reduce the frequency of MDRO infection in specific populations in a wide variety of settings. MDRO Surveillance • Supportive reasons for susceptibility (or sensitivity) testing – Susceptibility testing is often used to determine the likelihood that a particular drug treatment regimen will be effective in eliminating or inhibiting the growth of the infection. – Enables a “sentinel event” approach to new MDROs – Facilitates molecular typing of MDRO isolates • Reporting Options – Enhanced susceptibility reports • Pathogen-specific • Facility- or unit-specific • Provider-specific (for feedback) – Incidence Monitoring - Selected Pathogens • By unit; by provider (per 1000 patient days) • Requires teamwork (Laboratory, Information Technology and Infection Prevention and Control) MDRO Surveillance Questions • Still unanswered: – Proper timing of Active Surveillance Cultures – Site(s) and protocol(s) for obtaining cultures – Coordination with contact precautions • Healthcare worker (HCW) surveillance cultures? – Usually not needed unless HCWs are epidemiologically linked to MDRO transmission. Targeted Decolonization of Patients • Decolonization of patients aims to eradicate MDROs from colonized patients in an effort to prevent subsequent infection or spread. Specially treated cleansing cloths, which target harmful staph bacteria, can be used by patients before surgery to reduce the risk of infection. Decolonization of Patients Topical antibiotics may be applied; However, current guidelines, citing concern for the development of resistance to the drugs used for decolonization, advise against widespread use of this practice. Considerations for those who choose to proceed: • Decolonization of MDRO is most successfully achieved with MRSA. – Less likely to succeed with VRE – Rarely reported for Multiple drug-resistant gram negative bacilli (MDR-GNB) • Limiting factors: – Availability of surveillance cultures – Need for follow-up cultures – Occurrence of • Last decolonization • MRSA strain was resistant to mupirocin, or • Emergence of resistance during decolonization • HCW decolonization not usually needed Prevention Bundles See .edu courses for review of strategies to prevent: • Central Venous Catheter Blood Stream Infections (CVCBSI) • Ventilator Associated Pneumonia (VAP) • Catheter Associated Urinary Tract Infections (CAUTI) • Surgical Site Infections (SSI) Overview of Antibiotic Stewardship In the hospital setting, it is estimated that as much as 50% of antibiotic use is unnecessary. Antibiotic misuse fosters the development and spread of antibiotic resistance. • Antibiotic stewardship involves limiting inappropriate antibiotic use while optimizing the selection, dose, duration and route of therapy with the most appropriate drug for the patient. • Stewardship programs have been associated with improved antibiotic use and reduced costs. Judicious Use of Antibiotics • Attention to antibiotic ordering patterns – (IT, pharmacy and medical staff support) – Expert/peer review • Use antibiograms to help educate medical staff regarding appropriate antibiotic selection • Limit formulary choices – Prior approval programs • Automatic stop orders – Physician reminder systems – (lab and pharmacy support) • Review drug firms’ sales efforts on antibiotic prescribing patterns Summary • Clean hands and a clean environment are the two most important methods of controlling the spread of bacteria and other germs that cause HAIs. • We’re asking everyone, including our patients and visitors, to clean their hands before and after touching another person or the patients’ environment. • Kindly remind ANYONE who does not clean their hands or environment properly to do so. The safety of our patients and caregivers is of utmost priority. • While not every action noted in this presentation may pertain to your specific duties, all employees can help prevent the spread of MDROs by focusing on two basic elements of cleanliness: clean hands and a clean environment. The Basics of Patient Safety People Are Set-Up to Make Mistakes Incompetent people are, at most, 1% of the problem. The other 99% are good people trying to do a good job who make very simple mistakes and it's the processes that set them up to make these mistakes. Dr. Lucian Leape, Harvard School of Public Health How Can Safety be Improved? Human errors occur because of: Inattention Memory lapse Failure to communicate Poorly designed equipment Exhaustion Ignorance Noisy working conditions A number of other personal and environmental factors Where to Start Consider safety improvement recommendations made by external groups Implement Patient Safety Goals Patient Safety Standards Improve accuracy of patient identification 1. Use two identifiers NPSG.01.01.01 Eliminate transfusion errors related to pt misidentification NPSG.01.03.01 Improve effectiveness of communication among caregivers 2. Read back and verify NPSG.02.01.01 Standardization of abbreviations NPSG.02.02.01 Measure turn around of critical test results NSPG.02.03.01 Standardized approach to hands-off communication, including opportunity to ask & respond to questions NSPG.02.05.01 Improve Safety of Using Medications 3. Look alike- sound alike drugs NSPG.03.03.01 Label medications and containers on and off the sterile field NSPG.03.04.01 Reduce patient harm associated with use of anticoagulant therapy NSPG.03.05.01 Patient Safety Standards 7. Reduce the risk of health care associated infections 8. Hand hygiene NPSG.07.01.01 Infection related sentinel events NSPG.07.02.01 Prevent infections due to multiple drug-resistant organisms NSPG.07.03.01 Prevent line-associated bloodstream infections NSPG.07.04.01 Prevent surgical site infections NSPG.07.05.01 Medication Reconciliation Across the Continuum 9. On Admission NSPG.08.01.01 At Transfer NSPG.08.02.01 At Discharge NSPG.08.03.01 Modified med rec process where meds used minimally/prescribed for short duration NSPG.08.04.01 Reduce the Risk of Harm Resulting from Falls NSPG.09.02.01 Implement Fall Reduction Program Evaluate Effectiveness Patient Safety Standards 13. Encourage Patients Involvement in their Own Care Encourage patients and families to report concerns about safety NSPG.13.01.01 15. Identify Safety Risks Identify patients at risk for suicide NSPG.15.01.01 16. Improve recognition and response to changes in patients condition Code Prevention Team NSPG.16.01.01 Patient Safety Standards UNIVERSAL PROTOCOLPrevent errors in surgery 1. Conduct pre-procedure verification process UP.01.01.001 2. Mark the procedure site UP.01.02.01 3. Procedure time Out UP.01.03.01 Patient Rights HIPAA Advanced Directives Bioethics Everyone Has a Role in Patient Safety Employees and Physicians Management Administrative and Medical Staff Leaders Steps to Improve Safety Basic Tenets of Human Error Everyone commits errors. Human error is generally the result of circumstances that are beyond the conscious control of those committing the errors. Systems or processes that depend on perfect human performance are fatally flawed. A Strategic Objective We must redesign our processes so that simple mistakes don’t end up harming patients Eliminate opportunities for errors Build better safeguards to catch and correct errors before they reach the patient What hospital staff need to know about the impaired and/or disruptive practitioner The Impaired Practitioner Definition – one whose behavior or performance has been affected by alcohol, chemicals, and/or mental or physical illness that interferes with his or her ability to function competently. Signs of Substance Abuse Difficulty meeting schedules or deadlines Odor of alcohol Slurred speech Poor hygiene Poor coordination Isolation from others Frequent or unexpected absences Family problems Doesn’t answer pages Denial Financial problems Inappropriate anger Dramatic mood swings What should you do if you suspect practitioner impairment? 1. Report incidents to your supervisor – report up hospital chain of command 2. File an incident/occurrence report 3. Report issue to Vice President Medical Affairs, CMO or Chief of Staff 4. Call the Ethics H Reporting may save a life! What should you not do? Discuss suspicions with other staff or practitioners (always maintain confidentiality) Attempt an intervention with the practitioner yourself Allow patient safety to be jeopardized at any time – Call your supervisor immediately! Tolerate physical abuse or threats – Call security! Behaviors of a Disruptive Physician or Practitioner Employs threatening or abusive language Makes degrading or demeaning remarks Uses profanity or other offensive language Uses threatening or intimidating physical behaviors Makes public derogatory remarks about the quality of care provided by others Behaviors – continued Writes inappropriate entries in medical record concerning quality of care Imposes strange requirements on staff having nothing to do with good patient care Creates a hostile environment Has little or no insight into the effects of his or her behavior What are your options if you encounter a disruptive practitioner? Report all instances to your supervisor File an incident/occurrence report File a report through your peer review process Call your CNO or Chief of the Medical Staff or other medical staff leader Early intervention is the key, so don’t let this slide!! What should you not do? Argue with the physician or practitioner Tolerate physical abuse or threats of violence – call security Allow patient safety to be jeopardized Take it personally Ignore it and not report Occurrence Reporting System Occurrence Reports are an essential part of the visitor and patient safety programs They are used to: 1. Investigate and reduce risks to patients 2. Document the facts surrounding an occurrence 3. Identify trends within departments or across the hospital that can be addressed by improving processes. When & What You Should Report When? The occurrence reporting policy and procedure requires that you submit an occurrence report before the end of your shift. What is reportable? 1. An occurrence that is not consistent with the routine operation of the hospital or the routine care of the patient or patients. 2. Actual injury or the POTENTIAL for injury, illness, or property damage is enough for an occurrence report to be completed. Fact vs. Opinion Occurrence reports should not be used to blame an individual or department. When completing a report, you should keep your comments to the facts of the event and avoid opinions, speculation, and blame. Fact vs. Opinion Which scenarios are fact or opinion? 1. Patients states they had a wallet in a drawer. The previous nurse must have taken it. 2. Patient states they had a wallet in their drawer and that it is missing 3. Cardiac consultation ordered 12/5/04. Nurse A and B failed to note order and call consult. Consult called 12/8/04 after identifying omission. 4. Cardiac consultation ordered 12/5/04. Chart did not indicate consult completed. Consult called on 12/8/04. Performance Improvement Performance Improvement at Spalding Regional Medical Center addresses all services, sites and units of the medical center. Performance Improvement focuses constantly on improving services provided by leaders and departments, and care received by all patients, especially those with high risk and problem prone diagnoses. Data obtained from the community is also used to identify opportunities for improvement. Improving health outcomes for our community is the centerpiece of our performance improvement plan. Spalding looks at population based risks factors, individual risks factors, community demographics, major health problems, availability of health services, environmental factors and relationship of these factors to produce the community health status and uses the PDCA model to implement those initiatives. (See PDCA Model). Spalding Regional Medical Center uses a systematic organization-wide approach to monitor quality that is used to plan, design, measure, assess and continually improve organizational performance across the institution. An example of this approach is the Commitment to Quality (C2Q) teams that focuses on major PI initiatives. Some of the C2Q teams are Nursing/Clinical Quality, ER, Radiology, OR, and IHI 100K lives, LOS, Medication Administration and Safety. Examples of initiatives are the safety measures and the publicly reported quality indicators. Each department has the safety measures posted. Attached is a list of the quality indicators. (See Quality indicators monitored and reported at Spalding) Performance Improvement Methodology We use the concept of total quality management in a Plan Do Check Act (PDCA) model to organize our improvement initiatives. Begin Identify the outputs provided by the hospital/department Does the analysis support the hypothesis? No State team's ideas about what is going wrong within the process (Develop Hypothesis) Yes Identify the output to be improved Create a team Develop a description of the process which creates the output (flowcharting) Identify customers of the output Gather the customer's requirements State team's ideas about what is going wrong within the process (Develop hypothesis) Do you have enough data? No Collect Data Yes Brainstorm possible solutions (fishbone) Select "best" solution & document new process (Matrix)/(Flowchart) Develop implementation plan (action plan) Collect data (use original data collection plan) Analyze data Develop a plan for collecting information (data) about how the process is currently being performed (collection plan for basline data Is there quantifiable improvement? No P – Plan – Yellow Collect Data Yes D – Do – Blue Monitor new process C – Check – Green Analyze the Data Begin Again! A – Act - Red QUALITY MEASURES MONITORED AND REPORTED SPALDING REGIONAL MEDICAL CENTER The following information is to be completed on every patient admitted with a core measures diagnosis and is listed on time out sheets Advance Directives SRMC complies with the Patient Self Determination Act and requires all patients (over the age of 18) to have documentation of Advanced Directives. The Advance Directive informs the hospital of the patient’s healthcare decisions. Advance Directives may include the following: •Living Will •Healthcare Surrogate Designation •Refusal of Treatment •Durable Power of Attorney for Healthcare •Organ Donation • During the admitting process or pre-admission process the patient should receive information regarding communicating health care choices and Advance Directives. This information is included in the Patient Information Packet. • If the patient has an Advanced Directive, a copy is placed in the Medical Record. If a patient wishes to execute an Advanced Directive, the patient is provided with a copy of the Advance Directive form (from Admissions dept. or the Case Management/Social Services dept.) and the steps outlined in the policy are followed. Bioethics SRMC encourages ethically informed, responsible and compassionate decision making and practice throughout the range of our hospital’s activities. An Ethics committee provides a forum for case by case debate of ethical issues when there is conflict among healthcare professionals stemming from controversial patient care decisions. Complaints and Grievances • Every patient has the right to file a general complaint or concern about his/her care and treatment and not be penalized in any way for doing so. Any healthcare team member receiving a complaint from a patient along with the person in charge will, as soon as possible, attempt to correct the problem. The concern will be referred to the Department Manager or Shift Supervisor. All significant complaints and grievances will be referred to Risk Management and/or Customer Service. Communication • SRMC utilizes AT&T Language Line Services as a mechanism to meet the special needs required by our customers who do not speak English. AT&T Language Identification cards are available in Administration, Nursing Office and Nursing Departments to assist in the determination of the language being spoken. The complete procedure is documented in the policy and procedure. Safety Presentation Code Red → Fire The operator will announce Code Red and then a location. Each department has different functions during a Code Red. Please ask your supervisor what your function is. Please familiarize yourself with the proper fire control procedures and escape routes. Make sure you know where your fire extinguisher is located and the location of the fire alarm pull stations Your first order is to remove any patients from the fire area Second, notify by pulling a fire alarm station Third, try to contain the fire by shutting doors Fourth, if possible try to extinguish the fire. If not, evacuate. After the fire has been cleared by the proper channels, the operator will announce, “Code Red, All Clear” Code Red continued At the hospital we use the acronym RACE and PASS R rescue A alarm C contain E extinguish or evacuate P pull pin A aim S squeeze S spray When using a fire extinguisher: Pull the pin, Depress the handle, and Use sweeping motion at the base of the fire. Do Not Use the fire hose cabinets A = Common Combustibles C = Electrical Equipment B = Flammable Liquids Code Zero & Code Secure Code Zero means evacuation: Horizontal, Vertical, or Total Code Secure means Facility Lockdown: NO One enters or leaves the hospital for any reason Code Blue Code Pink Dr. 200 Code Blue Code Blue is a Cardiac Arrest/Cardiopulmonary Arrest This is when a person becomes unresponsive and pulseless Code Pink Patient, Infant to 14 years of age, found unresponsive or needing resuscitation efforts Dr. 200 Dr. 200 is a Code Blue on an infant in Labor and Delivery or the Nursery Code Weather Alert Pending Status indicates the probability of a severe weather condition that might interfere with hospital operations. Active Status indicates that a severe weather condition already exists and additional activities should be undertaken. – Departments are to remain operational. Staffing levels will be maintained to provide established standards of care. – It may become necessary to remove certain patients from areas in front of windows. Windows should remain closed unless otherwise instructed. – Assure patients they are safe and the hospital is taking the proper steps to insure their safety. Code D Code D is an emergency or disaster that seriously overtaxes or threatens to overtax the routine capabilities of the hospital All nurses and other personnel without specific assignments in the plan will report their availability to their supervisors and remain in their areas until further instructions Disaster functions are pre-assigned and designated by position rather than by name “Code D” Instructions for General Staff Follow the 5 R’s REMAIN in the Hospital - Do Not Leave RETURN To Your Assigned Work Area REPORT To Your Immediate Supervisor REASSESS Your Assigned Patients or Job Duties and Report Status to Your Supervisor RESPOND to All Instructions “Code D” Instructions for Supervisor/Manager RETURN To Your Assigned Work Area REASSESS the Condition of Your Unit (Physical area, Staff, & Patient Responsibilities) 1. Delegate Disaster Call List to assess availability. Do Not Ask Staff to come in. Labor Pool Leader will decide this. 2. Complete Disaster Unit Report REPORT To Your Immediate Supervisor (Supervisors Report to Dept. Director/OHS at night) RESPOND to All Instructions Code Adam Code Adam is an infant or child abduction Levels Are: 1. Infant – 1 Year 2. 1 – 4 Years of age 3. 5 – 12 Years of age 4. 12 Years and older Code Beta/Code Alpha These behavioral codes are called as an emergency summons utilized in the event of an acute acting out or violent episode with any person within the facility. A Behavioral Code is determined as a person having the potential to cause injury to self and/or others. Code Beta A Code Beta may be called in any situation which cannot be resolved by the staff present, and when verbal interventions have not been successful. Calling a Code Beta does not mean that the individual will be physically restrained. Code Alpha If the subject is in possession of a weapon (i.e. knife, gun or club), Code Alpha will be the emergency summons. The response to this code will be to notify the PBX operator at the emergency number (extension #1234) and call Security at extension #2419. The PBX operator will notify the Griffin Police Department immediately. Staff should not approach the subject, but secure the area and wait for the local police to arrive Code Lift If a patient, visitor, or employee has fallen and the first responder needs additional help in lifting the person, the emergency number will be called (1-2-3-4) and a Code Lift plus location will be called overhead. Once a Code Lift is called, all available transporters, engineering personnel and Over House supervisor should respond to the call. Before the person is lifted, an RN should triage the person and determine what is needed in the lift. If help is needed in lifting a patient from a bed to a chair or a chair to the bed, a portable lift is located on the first floor. MET Team Medical Emergency Team The MET team may be consulted to assist in the assessment and the emergency management of patients that the staff member has general concerns about or who develop an acute change in their condition. The patient or family member may request a MET team consult as well. Any member of the patient care team who has a concern or needs assistance in the assignment or evaluation of a patient may activate a consult with the MET team by dialing the emergency number (1-2-3-4) and advising the operator MET Team needed and patient’s room number. A MET team plus location will be called overhead. The MET team members are ICU RN and/or Over House Supervisor and Respiratory Therapist. MSDS – Material Data Sheets There is a MSDS on every chemical used in the hospital. This includes cleaners, whiteout, glue, sprays, etc. These sheets are located in the Emergency Room and the Engineering Department for your review if needed. Chemical Spill kit is located in the Plant Operations Office on the 2nd floor Abuse See attached policy End of Life Issues End of life is a condition that is caused by injury, disease or illness which has resulted in severe and permanent deterioration, indicated by the incapacity and complete physical dependency and for which, to a reasonable degree of medical certainty, treatment of the irreversible condition would be medically ineffective. Focus on end of life issues is not about cure, but about care. Individuals have the right to self-determination and decision-making regarding end of life issues through Advance Directives. Cultural and religious beliefs should be respected, therefore the health care provider should examine their own attitudes and spiritual beliefs regarding end of life issues in the context of providing patient care. Elizabeth Kubler-Ross described the process of dying and five stages in preparation for death: • • • • • • denial isolation anger bargaining depression acceptance Grief is an expected response to loss. Four stages of grief have been described: shock and numbness searching and yearning disorientation and disorganization resolution and reorganization Palliative care is a shift from cure to comfort caring for the whole patient, not just the illness. Palliative care is about feeling comfortable in body, mind and spirit. Meeting these needs may involve comforting the patient’s family as well. Each person approaches death in their own way, bringing to this last experience their own uniqueness. • Death comes in its own time; its own way. Death is as unique as the individual who is experiencing it . Organ Donation Organ Donation Clinicians should be aware of the legislative factors involved in organ donation. The uniform Anatomical Gift Act was enacted in 1970 by all 50 states. The act legally provides anyone above the age of 18 with the right to indicate willingness to become a donor at the time of death. The act also authorizes the next of kin to donate and protects the health care professional from liability related to participating in the donation process. These laws constitute the framework for “required request” in addition to approximately 454 state laws that require families be given the option to donate or to decline to donate. Ninety-five percent of all donor situations occur in the critical care units. Identifying Potential Organ Donors: All donors of vascular organs are patients who have been declared brain dead utilizing criteria that have been established within a particular locale or institution (Simmons et al., 1984). The nurse must be familiar with the policy and procedure specific to his or her institution. There have been many criteria used to diagnose brain death. Flye (1989) has reviewed many of the criteria used and has found three principles common to all: There have been many criteria used to diagnose brain death. Flye (1989) has reviewed many of the criteria used and has found three principles common to all: 1. Coma of established cause: no toxins, physiologic abnormalities corrected 2. Cerebral unresponsiveness, Absent brainstem reflexes: pupils, oculovestibular responses, respiration Clinicians, as well as all others involved in the consent process, should understand the decision to donate an organ is highly personal and emotional one. It is made under stressful conditions, thus the discussion should take place in non-threatening, private environment. The topic should not be discussed at the patient’s bedside, in the waiting area, or in open public places. The actual request for a donation will be made by staff from Lifelink of Georgia and have the ability to address questions that the family may have regarding timing, cost, and distribution of the organs, the surgical procedure and the effects on funeral plans. The manner in which a family is approached can make the difference in a positive or negative outcome. Families who receive accurate, truthful information, who have questions answered, and who believe they have been dealt with honestly are more likely to respond positively to a request for organ and tissue donation. The nurse is probably one of the most important people involved in this process. Nurses are more likely to identify the potential donor, call the referral to the OPO and be involved with approaching the family because of their existing relationship with the family. The donor families often find emotional benefit from their decision to donate. Research shows that beyond their altruistic satisfactions, they may often find solace and comfort in knowing their loved ones live on through others. Many nurses also receive benefit from the knowledge that their participation Medication Administration Pharmacy Hours 24 hours; 7 days per week (work assignment below is MondayFriday scenario) • In-house Pharmacist – ext 3743 • 1st and 2nd Floor Pharmacist 3771 • 3rd and ICU Pharmacist – 3790 • Clinical Pharmacist - 1400 • Before 9A or after 4P or on the weekends call ext 6910 Medication Administration/Rights 1. Medications are safely and accurately administered • MARs are printed around 4am daily • Any changes to orders must be handwritten on the MAR • You may request a new printed MAR on new admissions, level of care transfers, and post-operatively • Every time a medication is administered it must be documented on the MAR. If it is not charted on the MAR and that chart is audited then those charges are lost. • If the administration of any medication is ever in question then the patient’s chart should be reviewed before administering. Do not rely on the cardex alone. • For all meds the administration times must be accurately charted. (i.e.: if Vancomycin is to be given at 09:00, but is actually given at 09:30 then you must circle the printed time, write the actual time the med was given, and initial.) Medication Errors and Adverse Drug Reaction Reporting Reporting is NON-PUNITIVE!! – The hospital responds to ALL actual or potential adverse drug events and medication errors. • You can access the eSRM system on e-tenet.com to report ADRs and medication errors. Every single event, even if you feel it is minor, should be reported. Medication Access/Delivery Process Each unit has a Pyxis Machine where stock medications are stored. • • • You must fill out the appropriate paperwork to be granted access to these machines. There is a pyxis packet that you can keep as a reference. This packet will also be what you use to complete your Pyxis competency & thus be granted access to the Pyxis machine. All medications require an order to be sent to the Pharmacy and entered into the system prior to access to the medication. Some medications (as defined by JHACO) can be over-ridden. These medications are limited and for use in emergent and/or urgent situations in which the patient’s status would be changed if there was a delay in treatment. As each medication in each Pyxis machine falls below its PAR level the Pharmacy is notified and the medication is refilled on the next hourly round. Medication Access/Delivery Process con’t. • • • For non-formulary items they will often be placed in a bin in the tower of the Pyxis labeled “Meds Ordered Not Loaded.” When accessing these items, you must choose that icon on the Patient’s profile in order to access that medication. If that icon is not present on the patient’s profile then it can be over-ridden. All specially made IV’s such as Zantac drips, antibiotics, Potassium IV fluids, etc are placed on the appropriate hook that correlates to that patient’s specific room number. Some medications will also be stored in the refrigerator. You can access the refrigerated items through the patient’s profile or through the override function. Other medications, such as certain antibiotics, are loaded in the pyxis machine and shall be removed and activated by nursing for immediate patient use. IV Preparation by Nursing 1. 2. 3. Only medications that are being made for immediate patient use and considered emergent can be mixed on the floor. Aseptic technique must be used to prepare all medications. Label all IV solutions Controlled Substances • • • • • • All controlled substance are secured either in the Pyxis machines or in some areas of the hospital in locked cabinets. A narcotic inventory is to be done on each Pyxis machine once per week on Mondays. You can suspend a narcotic inventory count in the event that another nurse needs immediate access to the Pyxis. A nurse can waste a partial dose of a narcotic if another nurse witnesses the waste. The wasted dose should be disposed of properly. You can also return the waste to the pyxis return bin to have the Pharmacy waste. A nurse can NOT waste a whole dose of a narcotic. This will result in an incident report. Pain Management Margo McCaffery (1979) states that pain is whatever the patient says it is, existing whenever the patient says it does. Pain has physical, emotional, and spiritual components. Pain Management is a team effort that allows the patient to be as comfortable and free of pain as possible. The team consists of the patient, family, physician, nurse, physical therapist, pharmacist, clergy, and social worker. Pain management means the nurse should be able to: • 1. Assess each patient’s pain • 2. Use pain relief methods effectively • 3. Educate patients and family 4. Reduce barriers to effective pain management Pain Assessment measures the amount of pain the person is experiencing and the effect it is having on the person as a whole. The initial screening questions regarding pain need to determine if the patient is in pain now or has been in the last few weeks or months. If the patient answers affirmatively, examine the pain site and then further questions must be addressed. Pain Assessment con’t. 1. 2. 3. 4. 5. 6. 7. Location – Ask the patient to point to the site(s) of pain on their body or on a body diagram. Intensity – Ask the patient to rate his pain on 0-10 scale. (see attached scale and faces) Quality - A description of the pain in the patients own words should be elicited Onset/Duration – Elicit information about patterns of pain (continuous or intermittent) and variation. Aggravating/Reliving Factors – Ask what makes the pain better and worse. Effects of Pain – Effects on daily life functions such as sleeping, eating, dressing, working, emotions, etc. Examine pain site – Observe for swelling, redness, tenderness, guarding, splinting, etc. For Non-Verbal patients: FLACC assessment scale is used to score pain rating on a 0-10 scale Category Score 0 Score 1 Score 2 FACE No particular Expression or smile Occasional grimace, or frown, withdrawn, disinterested Frequent to constant quivering chin, clenched jaw LEGS Normal position or Relaxed Uneasy, restless, tense Kicking, or legs drawn up ACTIVITY Lying quietly, Normal position, Moves easily Squirming, shifting back and forth, tense Arched, rigid or jerking CRY No cry (awake or asleep) Moans, whimpers; occasional complaint Crying steadily, screams or sobs, frequent complaints CONSOLABIL ITY Content, relaxed Reassured by occasional touching, hugging or being talked to, distractible Difficult to console or comfort Each of the five categories is scored which results in a total score between 0-10. After scoring, continue to complete Pain Management Assessment for all items that are applicable. Finally, discuss the present pain management regimen and effectiveness, pain intensity, as well as the individuals pain goals related to function and quality of life. After the initial assessment, the patient must be reassessed regularly to ensure the pain is relieved. The clinician should evaluate the patient’s pain every time they assess the individual. Any patient with unrelieved pain must be evaluated every two hours or more often if indicated. The plan of care should be adjusted accordingly. Each subsequent assessment should evaluate the effectiveness of the treatment and if the pain has/has not been relieved. The clinician should determine the source of unrelieved pain. Goals of Pain Management: 1. At time of initial patient evaluation inform patients that pain relief is an important part of their care. 2. Initial and follow-up assessments will use the patient’s self report of pain as their primary indication of pain. 3. The assessment will focus on the location, quality, and intensity of pain. 4. Health care professionals in conjunction with the patient will establish and implement a plan to achieve pain relief. 5. Review and modify the plan of care for patients at regular intervals to achieve the best possible pain relief. Restraints Spalding Regional Medical Center’s philosophy concerning restraints is that use of a restraint device is the done as a last resort and only after the all reasonable alternatives have been tried and have failed. Alternatives to restraints should always be attempted prior to use. There should always be a physician order that states: reason for restraint, time limitation, and type of restraint. These orders must always be signed and dated appropriately. The patient should be assessed, reassessed, and restraints reordered according to policy and procedure and also depending on the type of restraint. Restrained patients need to have their restraints taken off and skin checked. Also check that food and fluids are offered and allow bathroom use every two hours. This must be documented as per the SRMC policy and procedure. The nurse should be knowledgeable regarding the policy and procedure for Restraints for SRMC. Restraints Physician Notification: Non-Violent/Non-Self-Destructive Restraint Use Immediately Violent/Self-Destructive Restraint Use Immediately Restraints Physician Face-to-Face Assessment: Non-Violent/Non-Self-Destructive Restraint Use 24 hours initially Violent/Self-Destructive Restraint Use 1 hour initially Restraints Physician Face-to-Face Re-assessment: Non-Violent/Non-Self-Destructive Restraint Use Each Calendar Day Violent/Self-Destructive Restraint Use Pts 18 and older- Q 8 hours Pts 9 – 17 – Q 4 hours Pts less than 9 – Q 4 hours Restraints Maximum time for Monitoring: Non-Violent/Non-Self-Destructive Restraint Use Q 2 hours Violent/Self-Destructive Restraint Use Q 15 minutes with continuous observation Blood Administration See attached policy Discharge Planning Discharge Planning / Social Services • Nursing Service must assess all patients for psychosocial needs at the time of admission and document their findings on the Nursing Admission Assessment. Every patient admitted to Spalding Regional Medical Center must receive an assessment of their discharge planning needs and if needs are identified, the patient/family must be referred to Social Services for a follow-up assessment. The following admissions should be automatically referred to Social Services: a. CVA’s b. Hip Fractures c. Individuals who are more than 75 years of age and living alone d. Overdose/suicide patients e. Patients from an extended care facility f. Patients for nursing home placement g. Women’s Services at risk situations h. Identified needs per nursing assessment sheet • 2. Social Services / Unit Based Care Coordinator must screen all admissions within one business day. If a emergency need arises when Social Services and Care Coordination are not on site, the Nursing Staff should notify the Overhouse Supervisor. The Overhouse Supervisor contacts Clinical Care Coordinator/Director as needed. • 3. If home health or post discharge planning needs are identified, the patient must be given their choice of the post discharge caregiver/vendor. If the patient does not have a choice, the Patient Choice Form and a list of vendors to select from must be given to the patient/family to choose a vendor. (Completed by Nursing Staff only if Care Coordination staff not on site). Most often discharges are planned ahead and arrangements have been made with forms completed and on chart at the time of discharge. 4. Once the patient selects a vendor, notify the vendor of the service to make arrangements for delivery of the equipment to the hospital or home depending on the need. (Exp. Walker or Bedside comode) The vendor’s phone number is listed on the patient choice –vendor selection form. Contact Care Coordination if there are questions concerning post discharge setup or if other than simple DME—exp: IV Antibiotics.