* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Illicit drugs in pregnancy - New York State Academy of
Maternal health wikipedia , lookup
HIV and pregnancy wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Prenatal testing wikipedia , lookup
Prenatal development wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
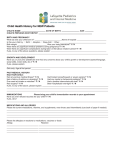
Managing common ambulatory issues in the pregnant patient Lee M. Stetzer, MD Albany Regional Family Medicine Conference October 15, 2011 Introduction • • • • “placental barrier” Thalidomide: 30% of exposed infants with developmental defects 1962: FDA requires that medications are shown to be safe and effective Do rate and extent of transfer of medications result in significant concentration in the fetus? Source: 1 FDA Risk Categories • • • • Rate medications as A, B, C, D, or X Mandated for medications approved after 1980 Do not refer to breastfeeding risk Danger of oversimplification • Risk may be modified by when or how long medications are used Source: 1 FDA Risk Categories • A: Controlled studies in women fail to demonstrate a risk to the fetus in the first trimester (and there is no evidence of risk in later trimesters), and the possibility of fetal harm seems remote. FDA Risk Categories • B: Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women or animal reproduction studies have shown an adverse effect (other than decrease in fertility) that was not confirmed in controlled studies in women in the first trimester (and there is no evidence of risk in later trimesters). FDA Risk Categories • C: Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus. FDA Risk Categories • D: There is positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (e.g., if the drug is needed in a life-threatening situation or for a serious disease for which safer drugs cannot be used or are ineffective). FDA Risk Categories • X: Studies in animals or human beings have demonstrated fetal abnormalities or there is evidence of fetal risk based on human experience or both, and the risk of the use of the drug in pregnant women clearly outweighs any possible benefit. The drug is contraindicated in women who are or may become pregnant. Cases: Case 1: 23 year old G1P0 at 26 weeks EGA with increasing nasal congestion that interferes with sleep. She has similar symptoms every fall. No fever, minimal facial pain or scratchy throat. She has tried nasal saline and a cool mist vaporizer in the bedroom without improvement. She has put impermeable covers over her pillow and mattress. She does not have any pets. Case 1: allergic rhinitis Case 1: allergic rhinitis • First line • • Topical intranasal glucocorticoids Other options • Oral antihistamines • • • • With or without decongestants Topical intranasal antihistamines Topical intranasal cromolyn Allergen immunotherapy Source: 2 Case 1: allergic rhinitis • Topical intranasal glucocorticoids • • • • Budesonide (Rhinocort Aqua): Category B Fluticasone (Flonase, Veramyst): Category C Mometasone (Nasonex): Category C Beclomethasone (Beconase AQ): Category C Source: 1, 3 Case 1: allergic rhinitis • Oral antihistamines • First generation • • • Chlorpheniramine: Category B Diphenhydramine: Category B Second generation • • • Loratidine: Category B Cetirizine: Category B Fexofenadine: Category C Source: 1, 3 Case 1: allergic rhinitis • Oral decongestants • Pseudoephedrine: Category C • • Possible first trimester risk Phenylephrine: Category C Source: 1, 3 Case 1: allergic rhinitis • Intranasal cromolyn • • Category B Possible first-line agent for mild symptoms Source: 1, 2 Case 1: allergic rhinitis • Intranasal antihistamines • • • Azelastine and olopatadine: Category C No human data, probably low risk Nasal vasoconstrictors • Oxymetazoline: Category C Source: 1, 2 Case 1: allergic rhinitis • Allergen immunotherapy • • Reasonable to not initiate during pregnancy Reasonable to continue maintenance therapy during pregnancy Source: 3 Pregnancy Rhinitis • • • • Hyperemia and edema of nasal mucosa Pathophysiology unknown Occurs in 20-30% of pregnant women Therapy (if needed) • • • Saline irrigation Ipratropium nasal spray (Category B) Intranasal steroids not effective Source: 3 Case 1 ½ Same patient returns 2 weeks later. She felt better for a few days, but then symptoms returned with 10 days of increasing headache and fever to 101° F. Also increased facial pressure. Exam shows purulent intranasal drainage. Case 1 ½: Acute bacterial sinusitis • Pain control • • acetaminophen (Category B) Ibuprofen (Category B) • • • • Trimester specific risk exists Naproxen (Category C) Hydrocodone (Category C) Codeine (Category C) Source: 1, 4 Case 1 ½: Acute bacterial sinusitis • If you choose to use antibiotics…. • • Amoxicillin: Category B Trimethoprim-sulfamethoxazole: Category C-C • • • Avoid in first trimester and near term Erythromycin: Category B Azithromycin: Category B Source: 1, 4 Case 2: 24 year old G2P1 at 28 weeks EGA comes in with worsening heartburn, especially at night. She does not have nausea, vomiting, diarrhea, headache, edema, or RUQ pain. The same thing happened during her last pregnancy 2 years ago, and instantly resolved after she delivered. Case 2: GERD 24 year old G2P1 at 28 weeks EGA comes in with worsening heartburn, especially at night. She does not have nausea, vomiting, diarrhea, headache, edema, or RUQ pain. The same thing happened during her last pregnancy 2 years ago, and instantly resolved after she delivered. Case 2: GERD • • • • Lifestyle modifications Tums or Maalox (Category C) H2 blockers (all Category B) PPIs • • • Lansoprazole (Prevacid), esomeprazole (Nexium), pantoprazole (Protonix): Category B Omeprazole (Prilosec):Category C Metoclopromide (reglan): Category B Source: 1 Case 3 A 30 year old G1P0 at 9 weeks EGA comes in with “morning sickness”. She has been having nausea for a few weeks. She vomits once every few days. She has no fever, abdominal pain, or diarrhea. She has had no weight loss. Labs are normal including electrolytes, renal and liver function, TSH, and CBC. She would like to avoid medications and try “natural remedies” first. Case 3: Nausea • • • • • Overall, poor evidence for interventions Lifestyle modifications Ginger… in any form Vitamin B6 (pyridoxine): Category A Doxylamine: Category A • Diclectin Sources: 1,5,6 Case 3: Nausea • • • • Ondansetron (Zofran): Category B Promethazine (Phenergan): Category C Metoclopromide Meclizine: Category B Sources: 1,5,6 Case 4 A 19 year old G1P0 at 21 weeks EGA presents with 2 days of dysuria. She also reports urinary frequency and urgency for the past 21 weeks. She has no fever or back pain. Case 4: Cystitis • • Potential for obstetric complications No evidence to support a first-line antibiotic • • Cephalosporins all Category B Nitrofurantoin: Category B • • Although recent report suggesting need for increased study (9) Fosfomycin: Category B Sources: 1,7,8,9 Case 4: Cystitis • • • Amoxicillin-Clavulanate: Category B-B Trimethoprim-sulfamethoxazole Ciprofloxacin: Category C Sources: 1,7,8 Case 5 • A 24 year old G1P0 at 18 weeks EGA had a URI onset about a week ago. Several days later she presented to the ED with wheezing, dyspnea, and nonproductive cough. No fever. She was given albuterol nebulizer treatments (which helped), and a prescription for an albuterol MDI, which has been helping. She comes to your office today, still using the inhaler 4 to 6 times a day. She has had wheezing in the past with exertion, but it was never this bad. Case 5: Asthma • • • Uncontrolled asthma associated with increased risk for perinatal mortality, preeclampia, preterm birth, and low birthweight Better control associated with decreased risk Course of asthma changes in 2/3 of pregnant women Source: 10 Case 5: Asthma • • Control, control, control “It is safer for pregnant women with asthma to be treated with asthma medications than for them to have asthma symptoms and exacerbations…. Inadequate control of asthma is a greater risk to the fetus than asthma medications are.” (10) Source: 10 Case 5: Asthma • • • • • • Albuterol: Category C Salmeterol, formoterol: Category C Budesonide (Pulmicort): Category B Mometasone (Asmanex), beclomethasone (Q-Var), fluticasone (Flovent): Category C Combination ICS/LABA: limited data Prednisone: Category C Source: 1,10 Case 5: Asthma • • • Theophylline: Category C Ipratropium: Category B Montelukast: Category B Source: 1,10 In conclusion • • • There is always the potential for a medication to cross the placenta Must balance risks and benefits Consent must be informed Sources: 1) Briggs, Gerald G, et al. Drugs in Pregnancy and Lactation. 8th Ed. Lippincott Williams & Wilkins. 2008. 2) deShazo, Richard and Kemp, Stephen. Pharmacotherapy of allergic rhinitis. Up to Date ver 19.2. 2011. 3) Schatz, Michael. Recognition and management of allergic disease during pregnancy. Up to Date ver 19.2. 2010 4) Hwang, Peter and Getz, Anne. Acute sinusitis and rhinosinusitis in adults. Up to Date ver 19.2. 2011 5) Matthews A, Dowswell T, Haas DM, Doyle M, O'Mathúna DP. Interventions for nausea and vomiting in early pregnancy. Cochrane Database of Systematic Reviews 2010, Issue 9. Art. No.: CD007575. DOI: 10.1002/14651858.CD007575.pub2. Sources continued: 6) Smith, Judith, et al. Treatment of nausea and vomiting of pregnancy (hyperemesis gravidarum and morning sickness). Up to Date ver 19.2. 2011 7) Hooton, Thomas. Urinary tract infections and asymptomatic bacteriuria in pregnancy. Up to Date ver 19.2. 2011 8) Vazquez JC, Abalos E. Treatments for symptomatic urinary tract infections during pregnancy. Cochrane Database of Systematic Reviews 2011, Issue 1. Art. No.: CD002256. DOI: 10.1002/14651858.CD002256.pub2 9) Crider, Krista, et al. Antibacterial Medication Use During Pregnancy and Risk of Birth Defects. Arch Pediatr Adolesc Med. 2009;163(11):978-985 10) NAEPP Working Group Report on Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment. U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES. National Institutes of Health. National Heart, Lung, and Blood Institute. January 2005