* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
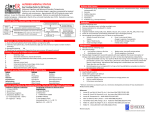
Delirium in the Elderly Dr.leila kashani 92/3/23 دستیار روانپزشکی دانشگاه علوم پزشکی تهران بیمارستان روزبه DEFINITION Acute and clinically significant deficit in cognition , attention or memory Impaired or altered perception , illusion Disturbances of circadian rhythms Acute change in mental status with a fluctuating course Altered level of consciousness Behavioral disturbances KEY FEATURES Acute onset Inattention Disorganized thinking Altered level of consciousness Cognitive abnormalities (disorientation, language difficulties, impairment in memory/learning) Perceptual disturbances (illusions, delusions, hallucinations) Emotional disturbances (anxiety, fear, irritability, anger, depression, euphoria) OTHER NAMES Acute confusional state Encephalitis - encephalopathy Acute brain failure Toxic metabolic state CNS toxicity Sun downing Organic brain syndrome Cerebral insufficiency INCIDENCE AMONG ELDERLY PATIENTS IS HIGH 1/3 of patients presenting to ER 1/3 of inpatients aged 70+ on general med units Incidence ranges 5.1% to 52.2% after noncardiac surgery Highest rates after hip fracture ( 50 % ) and aortic surgeries In ICU : 70 -87 % DELIRIUM: INCREASED RISK OF… Functional decline New nursing home placement Persistent cognitive decline: 18-22% of hospitalized elders with complete resolution 6-12 months after discharge HOW TO DISTINGUISH DELIRIUM FROM DEMENTIA Features seen in both: Disorientation Memory impairment Paranoia Hallucinations Emotional lability Sleep-wake cycle reversal Key features of delirium: Acute onset Impaired attention Altered level of consciousness PRODROME Patients may describe and/or manifest: Decreased concentration Irritability, restlessness, anxiety, depression Hypersensitivity to light and sound Perceptual disturbances Sleep disturbance - daytime somnolence and nocturnal agitation Delirium may be the only manifestation of life-threatening illness in the elderly patient DELIRIUM:PSYCHOMOTOR SUBTYPES Hyperactive (most recognized) ↑ psychomotor activity (agitation, mood labiality, refusal to cooperate, disruptive behaviors, combativeness) Hypoactive (under recognized) ↓ psychomotor activity (sluggish, lethargic, withdrawn, apathy) Mixed (highest risk for morbidity/mortality) Fluctuating course A MODEL OF DELIRIUM A multifactorial syndrome that arises from an interrelationship between: Predisposing factors a patient’s underlying vulnerability AND Precipitating factors noxious insults PREDISPOSING FACTORS I.E. BASELINE UNDERLYING VULNERABILITY Baseline cognitive impairment 25-31% of delirious patients have underlying dementia Medical comorbidities: Any medical illness Infections Toxins, including drugs Substance withdrawal Organ failure: heart, liver, kidney, etc. Metabolic Primary brain disorders Visual impairment Hearing impairment Functional impairment Depression Advanced age History of ETOH abuse Male gender PRECIPITATING FACTORS I.E. NOXIOUS INSULTS Medications Bedrest Indwelling bladder catheters Physical restraints Iatrogenic events Uncontrolled pain Fluid/electrolyte abnormalities Infections Medical illnesses Urinary retention and fecal impaction ETOH/drug withdrawal Environmental influences SOME DRUG CLASSES THAT ARE ASSOCIATED WITH DELIRIUM Medications with psychoactive effects: 3.9-fold increased risk 2 or more meds: 4.5-fold Sedative-hypnotics: 3.0 to 11.7-fold Narcotics: 2.5 to 2.7-fold Anticholinergic drugs: 4.5 to 11.7-fold Risk of delirium increases as number of meds prescribed rises PREVENTION=GOOD HOSPITAL CARE FOR THE ELDERLY PATIENT RISK FACTOR INTERVENTION Cognitive impairment Orientation protocol, cognitively stimulating activities 3x/day Sleep deprivation Nonpharmacologic protocol, noise reduction, schedule adjustments Immobility Ambulation or active ROM exercises; minimize equipment Visual impairment Glasses or magnifying lens, adaptive equipment Hearing impairment Portable amplifying devices, earwax disimpaction Dehydration Early recognition and volume repletion MANAGING CONFUSED BEHAVIORS: APPROACH STRATEGIES Introduce yourself at each encounter Use touch as appropriate Start with the “Soft Approach” Smile Warm demeanor Pleasant voice tones Go slow Talk in short, simple sentences Avoid correcting/confrontation Appeal to the emotion and let the patient know you will keep him/her safe Be flexible in getting tasks accomplished KEYS TO EFFECTIVE MANAGEMENT Find and treat the underlying disease(s) and contributing factors Comprehensive history and physical Including neurological and mental status exams Choose lab tests and imaging studies based on the above Review medication list (Psychotropics, narcotics, anticholinergics ,Digoxin, prednisone, furosemide, cimetidine have anticholinergic properties.) CBC, electrolytes, BUN, Cr, glucose, LFTs, albumin O2 Saturation Urinalysis TSH, B12 ? Toxin screen CXR CNS imaging remains debatable. LP in febrile patient with meningeal signs Cause not identified in 15 to 25% DIAGNOSIS History from family and/or caregivers Bedside observations DSM-IV diagnostic criteria Diagnostic errors are common in: Hypoactive form The setting of rapid fluctuations of cognition. DIFFERENTIAL DIAGNOSIS Dementia Alzheimer dementia Functional psychiatric disorders – delusional psychosis or depressive states Misdiagnosed as depression in as many as 40% of cases Schizophrenia has a more chronic hx with highly systematized delusions. TREATMENT OF DELIRIUM Treatment of underlying disorder will usually resolve in rapid improvement of delirium The diagnosis of delirium may serve as a marker for future cognitive and functional decline ALWAYS TRY NONPHARMACOLOGIC MEASURES FIRST Presence of family members Interpersonal contact and reorientation (Provide clocks, calendars )and environmental support Provide visual and hearing aids Remove indwelling devices: i.e. Foley catheters Mobilize patient A quiet environment with low-level lighting Uninterrupted sleep Reduce noise levels. Minimize room changes in the hospital MANAGEMENT: HYPERACTIVE, AGITATED DELIRIUM Use drugs only if absolutely necessary: harm, interruption of medical care First line agent: haloperidol (IV, IM, or PO) For mild delirium: Oral dose: 0.25-0.5 mg IV/IM dose: 0.125-0.25 mg For severe delirium: 0.5-1 mg IV/IM repeated q30 min until calm Patient will likely need 2-5 mg total as a loading dose Maintenance dose :loading dose divided BID May use quetiapine and risperidone ,… WHAT ABOUT LORAZEPAM? Second line agent Reserve for: Sedative and ETOH withdrawal Neuroleptic Malignant Syndrome SUMMARY OF KEY POINTS Evaluation should focus on ruling out infection, medication toxicity, neurological events, metabolic abnormalities, and new cardiorespiratory problems. Prevention is the best therapy – focus on interpersonal and environmental support. antipsychotics and benzodiazepines are useful in symptom control. TAKE HOME POINTS: DELIRIUM IN THE ELDERLY A multifactorial syndrome: predisposing vulnerability and precipitating insults Prevention should be our goal If delirium occurs, treat the underlying causes Always try nonpharmacologic approaches Use low dose antipsychotics in severe cases thanks and any Questions?