* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Addiction Management
Survey
Document related concepts
Transcript
•
To gain a broad understanding of relevant terms used by the medical
community in relationship to addiction management.
•
To explore the current theories of the neurobiology underlying the process
of addiction.
•
To briefly look at treatment modalities for some of the more commonly
abused substances in the world of addiction.
A. SUBSTANCE-USE DISORDERS
SUBSTANCE ABUSE
maladaptive pattern of use leading to clinically significant impairment or
distress, as manifested by >1 of the following within a 12 month period.
•
recurrent use resulting in failure to fulfill major role obligation;
•
recurrent use in situations in which it is physically hazardous
(e.g. driving);
•
Continued use despite interference with social or interpersonal function;
A. SUBSTANCE-USE DISORDERS
SUBSTANCE DEPENDENCE (ADDICTION)
Maladaptive pattern of use leading to clinically significant impairment or distress, as
manifested by >3 occurring at any time in the same 12 month period.
•
tolerance
•
withdrawal/use to avoid withdrawal
•
taken in larger amt or over longer period than intended
•
persistent desire or unsuccessful efforts to cut down
•
excessive time to procure, use substance, or recover from its effects
•
important interests/activities given up or reduced
•
continued use despite physical/psychological problem
caused/exacerbated by substance
B. SUBSTANCE-INDUCED DISORDERS
SUBSTANCE INTOXICATION
Reversible physiological and behavioural changes due to recent exposure
to a substance .
SUBSTANCE WITHDRAWAL
Substance specific syndrome that develops following cessation of or reduction
in dosage of regularly used substances.
•
•
•
•
•
•
•
Psychological dependence: the desire to repetitively consume a drug, even if at the expense of
social occupational or recreational activities which often leads to the persistence of drug use
despite implicit knowledge that the drug if likely causing a physical or mental problem.
Physical dependence: the condition in which the user of the abused substance undergoes
untoward physical effects when the drug is stopped or when its effect is counteracted by a specific
antagonist.
Addiction: a concept without a consistent, universally accepted definition, that refers to
compulsive use and overwhelming involvement with a drug, including spending an increasing
amount of time obtaining the drug, using the drug, or recovering from its effects. It may occur with
or without physical dependence and implies the risk of harm if the user does not stop using the
substance that is being abused.
Drug abuse: is definable only in terms of societal disapproval and may involve the following…
– Experimental and recreational use of drugs which are usually illegal.
– Unsanctioned or illegal use of psychoactive drugs to relieve problems or symptoms.
– Use of drugs because of dependence or the need to prevent withdrawal.
Recreational drug use: the episodic use of drugs in relatively small doses, preculding clinical
toxicity and development of tolerance and physical dependence.
Tolerance: the need to progressively increase the dosage of a drug to produce the effect
originally achieved with smaller doses.
Intoxication: the development of a reversible substance-specific syndrome of mental and
behavioral changes that may involve altered perception, euphoria, cognitive impairment, impaired
judgment, impaired physical and social functioning, mood lability, belligerence or a combination of
any of the above.
EPIDEMIOLOGY
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Approximately 1 in 5 people between the ages of 16 and 59 said that they had taken at least one of the drugs mentioned.
People ages 18 to 21 were most likely to admit having taken drugs with almost half (46%) claiming to have taken them.
More men than women said that they had taken drugs. 24% of men and 16% of women had taken at least one kind of drug
in their lives. Amongst those ages 18-21; 51% of men and 38% of women had taken drugs.
Marijuana was the most commonly used drug, experienced by 12% of all participants and 24% of those ages 18 to 25.
19.5 million people over the age of 12 use illegal drugs in the United States (Mayo Clinic).
19,000 deaths occurred from Drug Addiction in the US (Mayo Clinic).
9,102 persons died of drug-induced causes in 1999 USA (NVSR Sep 2001). 19,102 per year, 1,591 per month, 367 per week,
52 per day, 2 per hour
There were 601,776 estimated drug-related emergency department episodes in 2000.
Alcohol in combination with other drugs was the most frequently mentioned drug at time of emergency department
admission (204,524), followed by cocaine (174,896), heroin/morphine (97,287), and marijuana (96,446).
From 1999 to 2000, emergency department mentions of prescription drugs containing oxycodone increased 68%(from 6,429
to 10,825), and mentions of drugs containing hydrocodone increased 31% (from 14,639 to 19,221).
Employed Drug Abusers cost their employers about twice as much in medical and worker compensation claims as their
drug-free coworkers.
Marijuana is the most commonly used illicit drug. In 2001, it was used by 76% of current illicit drug users.
Opiates accounted for 83% of admissions for injection Drug Addiction followed by methamphetamine/amphetamine (11%),
and cocaine (5%)
Among 1999 injected drug admissions, persons admitted for injecting opiates averaged 14 years of use before entering
treatment for the first time. Those admitted for injecting methamphetamine/amphetamine averaged 12 years, and for
cocaine 13 years.
EPIDEMIOLOGY
Past Month Illicit Drug Use among Persons Aged 12 or Older, by Age: 2008
EPIDEMIOLOGY
Past Month Illicit Drug Use among Persons Aged 12 or Older, by Race/Ethnicity: 2008
COMMONLY ABUSED SUBSTANCES
Specific Drug Used When Initiating Illicit Drug Use among Past Year Initiates of
Illicit Drugs Aged 12 or Older: 2008
WHAT CAUSES ADDICTION?
• Is it an actual disease?
• Is it a choice?
• At what point should it be considered
clinical?
• Are there positive addictions one can have?
And if so, should they be treated?
Case Study
A retired accountant developed a tremor and slowing of movements and was diagnosed
with Parkinson’s disease at age 67. At that time, his neurologist prescribed levodopa to
restore dopamine levels. A couple of years later, motor symptoms start to fluctuate and
the dopamine receptor agonist ropinirole is added to his treatment. A few months later, he
develops a strong interest in gambling, first buying lottery tickets and then visiting a
casino almostevery day. He conceals his gambling activity until he has lost more than
$100,000. When he came for a consultation 5 weeks ago, ropinirole was replaced with
monoamine oxidase inhibitor therapy. He now reports that his interest in gambling has
disappeared. What may be the link between the dopamine agonist treatment and
gambling addiction?
TIME-PERMITTING AUDIO-VISUAL CASE STUDY
•
Current theories on the
neurobiology of addiction
Every addictive drug causes its own characteristic spectrum of acute effects, but all
have in common that they induce strong feelings of euphoria and reward.
•
Addictive drugs increase the level of dopamine.
•
Addiction, consists of compulsive, relapsing drug use despite negative
consequences, at times triggered by cravings that occur in response to contextual
cues.
•
Although dependence invariably occurs with chronic exposure, only a small
percentage of subjects develop a habit, lose control, and become addicted.
•
With nearly one in 10 Americans over the age of 12 classified with substance abuse
or dependence, addiction takes an emotional, psychological, and social toll on the
country. The economic costs of substance abuse and addiction alone are estimated
to exceed a half trillion dollars annually in the United States due to health care
expenditures, lost productivity, and crime.- nlm.nih.gov
•
Currently, addiction affects 23.2 million Americans — of whom only about 10 percent
are receiving the treatment they need.
Current theories on the
Animal models inof
addiction
research
neurobiology
addiction
•
Many of the recent advances in addiction research have been made possible by the use of animal models. Since
drugs of abuse are not only rewarding but also reinforcing, an animal will learn a behavior (eg, press a lever) when
paired with drug administration. In such a self-administration paradigm, the number of times an animal is willing to
press the lever in order to obtain a single dose reflects the strength of reinforcement and is therefore a measure of
the rewarding properties of a drug. Observing withdrawal signs specific for rodents (eg, escape jumps or "wet-dog"
shakes after abrupt termination of chronic morphine administration) allows the quantification of dependence.
Behavioral tests for addiction in the rodent have proven difficult to develop and so far no test fully captures the
complexity of the disease. However it is possible to model core components of addiction, for example by
monitoring behavioral sensitization and conditioned place preference. In the first test, an increase in locomotor
activity is observed with intermittent drug exposure. The latter tests for the preference of a particular environment
associated with drug exposure by measuring the time an animal spends in the compartment where a drug was
received compared with the compartment where only saline was injected (conditioned place preference). Both
tests have in common that they are sensitive to cue-conditioned effects of addictive drugs. Subsequent exposures
to the environment without the drug lead to extinction of the place preference, which can be reinstated with a low
dose of the drug. These persistent changes serve as a model of relapse and have been linked to synaptic
plasticity of excitatory transmission in the ventral tegmental area and nucleus accumbens. Recent findings suggest
that prolonged self-administration of cocaine leads to behaviors in rats that closely resemble human addiction.
Such "addicted rats" are very strongly motivated to seek cocaine, continue looking for the drug even when no
longer available, and self-administer cocaine in spite of negative consequences, such as an electric foot shock.
These findings suggest that addiction is a disease that does not respect species boundaries.
Current theories on the
neurobiology of addiction
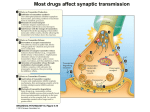
Addictive Drugs Increase the Level of Dopamine: Reinforcement
•
To understand the long-term changes induced by drugs of abuse, their initial molecular and cellular
targets must be identified. A combination of approaches in animals and humans, including functional
imaging, has revealed the mesolimbic dopamine system as the prime target of addictive drugs. This
system originates in the ventral tegmental area (VTA), a tiny structure at the tip of the brain stem,
which projects to the nucleus accumbens, the amygdala, the hippocampus, and the prefrontal cortex.
Most projection neurons of the VTA are dopamine-producing neurons. When the dopamine neurons of
the VTA begin to fire in bursts, large quantities of dopamine are released in the nucleus accumbens and
the prefrontal cortex. Early animal studies pairing electrical stimulation of the VTA with operant
responses (eg, lever pressing) that result in strong reinforcement established the central role of the
mesolimbic dopamine system in reward processing. Direct application of drugs into the VTA also acts
as a strong reinforcer, and systemic administration of drugs of abuse causes release of dopamine.
Current theories on the
neurobiology of addiction
Addictive Drugs Increase the Level of Dopamine: Reinforcement
Current theories on the
neurobiology of addiction
Addictive Drugs Increase the Level of Dopamine: Reinforcement
•
•
As a general rule, all addictive drugs activate the mesolimbic dopamine system. The behavioral
significance of this increase of dopamine is still debated. An appealing hypothesis is that
mesolimbic dopamine codes for the difference between expected and actual reward and thus
constitutes a strong learning signal .
Since each addictive drug has a specific molecular target that engages distinct cellular
mechanisms to activate the mesolimbic system, three classes can be distinguished: A first group
binds to Gio protein-coupled receptors, a second group interacts with ionotropic receptors or
ion channels, and a third group targets the dopamine transporter (Table 32–1 and Figure 32–
2). G protein-coupled receptors (GPCRs) of the Gio family inhibit neurons through postsynaptic
hyperpolarization and presynaptic regulation of transmitter release. In the VTA, the action of these
drugs is preferentially on the -aminobutyric acid (GABA) neurons that act as local inhibitory
interneurons. Addictive drugs that bind to ionotropic receptors and ion channels can have
combined effects on dopamine neurons and GABA neurons, eventually leading to enhanced
release of dopamine. Finally, addictive drugs that interfere with monoamine transporters block
reuptake or stimulate nonvesicular release of dopamine, causing an accumulation of extracellular
dopamine in target structures. Since neurons of the VTA also express somatodendritic
transporters, which normally clear dopamine released by the dendrites, class III drugs also
increase dopamine level in the VTA. Although drugs of this class also affect transporters of other
monoamines (norepinephrine, serotonin), it is the action on the dopamine system that remains
central for addiction. This is consistent with the observations that antidepressants that block
serotonin and norepinephrine uptake, but not dopamine uptake, do not cause addiction even after
prolonged use.
Current theories on the
neurobiology of addiction
Addictive Drugs Increase the Level of Dopamine: 3 classes of MOA
Current theories on the
neurobiology of addiction
The Dopamine Hypothesis of Addiction
•
•
In the earliest version of the hypothesis described in this chapter, mesolimbic dopamine was
believed to be the neurochemical correlate of pleasure and reward. However, during the past
decade, experimental evidence has led to several revisions. Phasic dopamine release may
actually code for the prediction error of reward rather than the reward itself. This distinction is
based on pioneering observations in monkeys that dopamine neurons in the ventral tegmental
area (VTA) are most efficiently activated by a reward (eg, a few drops of fruit juice) that is not
anticipated. When the animal learns to predict the occurrence of a reward (eg, by pairing it with a
stimulus such as a sound), dopamine neurons stop responding to the reward itself (juice), but
increase their firing rate when the conditioned stimulus (sound) occurs. Finally, if reward is
predicted but not delivered (sound but no juice), dopamine neurons are inhibited below their
baseline activity and become completely silent. In other words, the mesolimbic system
continuously scans the reward situation. It increases its activity when reward is larger than
expected, and shuts down in the opposite case, thus coding for the prediction error of reward.
Under physiologic conditions the mesolimbic dopamine signal could represent a learning signal
responsible for reinforcing constructive behavioral adaptation (eg, learning to press a lever for
food). Addictive drugs, by directly increasing dopamine, would generate a strong but inappropriate
learning signal, thus hijacking the reward system and leading to pathologic reinforcement. As a
consequence, behavior becomes compulsive; that is decisions are no longer planned and under
control, but automatic, which is the hallmark of addiction.
Current theories on the
neurobiology of addiction
The Dopamine Hypothesis of Addiction
•
This appealing hypothesis has been challenged based on the observation that some
reward and drug-related learning is still possible in the absence of dopamine. Another
intriguing observation is that mice genetically modified to lack the primary molecular
target of cocaine, the dopamine transporter DAT, still self-administer the drug. Only
when transporters of other biogenic amines are also knocked out does cocaine
completely lose its rewarding properties. However, in DAT–/– mice, in which basal
synaptic dopamine levels are high, cocaine still leads to increased dopamine release,
presumably because other cocaine-sensitive monoamine transporters (NET, SERT)
are able to clear some dopamine. When cocaine is given, these transporters are also
inhibited and dopamine is again increased. As a consequence of this substitution
among monoamine transporters, fluoxetine (a selective serotonin reuptake inhibitor,
see Chapter 30) becomes addictive in DAT–/– mice. This concept is supported by
newer evidence showing that deletion of the cocaine binding site on DAT leaves
basal dopamine levels unchanged but abolishes the rewarding effect of cocaine.
Current theories on the
neurobiology of addiction
The Dopamine Hypothesis of Addiction
•
•
The dopamine hypothesis of addiction has also been challenged by the
observation that salient stimuli that are not rewarding (they may actually
even be aversive and therefore negative reinforcers) also activate the VTA.
However, the neurons in the VTA that are activated by aversive stimuli do
not release dopamine, and dopamine neurons are actually inhibited by
aversive stimuli. These findings suggest that the controversy can be
resolved in favor of dopamine reward theories.
Whatever the precise role of dopamine under physiologic conditions, all
addictive drugs strongly increase its concentration in target structures of the
mesolimbic projection. This suggests that high levels of dopamine may
actually be at the origin of the adaptive changes that underlie dependence
and addiction.
Current theories on the
neurobiology of addiction
Addiction: A Disease of Maladaptive Learning
•
•
•
Addiction is characterized by a high motivation to obtain and use a drug despite negative consequences. With
time, drug use becomes compulsive ("wanting without liking"). Addiction is a recalcitrant, chronic, and stubbornly
relapsing disease that is very difficult to treat.
The central problem is that even after successful withdrawal and prolonged drug-free periods, addicted individuals
have a high risk of relapsing. Relapse is typically triggered by one of the following three conditions: reexposure to
the addictive drug, stress, or a context that recalls prior drug use. It appears that when paired with drug use, a
neutral stimulus may undergo a switch and motivate ("trigger") addiction-related behavior. This phenomenon may
involve synaptic plasticity in the target nuclei of the mesolimbic projection (eg, nucleus accumbens). Several
recent studies suggest that the recruitment of the dorsal striatum is responsible for the compulsion. This switch
may depend on synaptic plasticity in the nucleus accumbens of the ventral striatum, where mesolimbic dopamine
afferents and cortical glutamatergic afferents converge. If dopamine release codes for the prediction error of
reward (see The Dopamine Hypothesis of Addiction), pharmacologic stimulation of the mesolimbic dopamine
systems will generate an unusually strong learning signal. Unlike natural rewards, addictive drugs continue to
increase dopamine even when reward is expected. Such overriding of the prediction error signal may eventually
be responsible for the usurping of memory processes by addictive drugs.
The involvement of learning and memory systems in addiction is also suggested by clinical studies. For example,
the role of context in relapse is supported by the report that soldiers who became addicted to heroin during the
Vietnam War had significantly better outcomes when treated after their return home, compared with addicts who
remained in the environment where they had taken the drug. In other words, cravings may recur at the
presentation of contextual cues (eg, people, places, or drug paraphernalia). Current research therefore focuses on
the effects of drugs on associative forms of synaptic plasticity, such as long-term potentiation (LTP), which
underlie learning and memory (see Synaptic Plasticity & Addiction).
Current theories on the
neurobiology of addiction
Addiction: A Disease of Maladaptive Learning: Synaptic Plasticity & Addiction
•
Long-term potentiation (LTP) is a form of experience-dependent synaptic plasticity that is induced
by activating glutamate receptors of the N-methyl-D-aspartate (NMDA) type. Since NMDA
receptors are blocked by magnesium at negative potentials, their activation requires the
concomitant release of glutamate (presynaptic activity) onto a receiving neuron that is depolarized
(post-synaptic activity). Correlated pre- and postsynaptic activity durably enhances synaptic
efficacy and triggers the formation of new connections. Because associativity is a critical
component, LTP has become a leading candidate mechanism underlying learning and memory.
LTP can be elicited at glutamatergic synapses of the mesolimbic reward system and is modulated
by dopamine. Drugs of abuse could therefore interfere with LTP at sites of convergence of
dopamine and glutamate projections (eg, ventral tegmental area [VTA], nucleus accumbens, or
prefrontal cortex). Interestingly, exposure to an addictive drug triggers LTP at excitatory afferents
and reduces GABAA receptor-mediated inhibition of the VTA, thus increasing the excitability of
dopamine neurons. Genetic manipulations in mice that abolish LTP at this synapse also have
effects on persistent changes of drug-associated behavioral paradigms such as reinstatement of
conditioned place preference, further supporting the idea that LTP is involved in contextdependent components of relapse. Similarly, interfering with transcriptional signaling implicated in
the late phases of LTP affects conditioned place preference.
Current theories on the
neurobiology of addiction
Addiction: A Disease of Maladaptive Learning
•
•
Non–substance-dependent disorders, such as pathologic gambling and compulsive shopping,
share many features of addiction. Several lines of arguments suggest that they also share the
underlying neurobiologic mechanisms. This conclusion is supported by the clinical observation
that, as an adverse effect of dopamine agonist medication, patients with Parkinson's disease may
become pathologic gamblers (see Case Study). Others patients may develop a habit for
recreational activities, such as shopping, eating compulsively, or becoming excessively involved in
sexual activity (hypersexuality). Although large-scale studies are not yet available, an estimated 1
of 7 parkinsonian patients develops an addiction-like behavior when receiving dopamine agonists.
Large individual differences exist also in vulnerability to substance-related addiction. Whereas one
person may become "hooked" after a few doses, others may be able to use a drug occasionally
during their entire lives without ever having difficulty in stopping. Even when dependence is
induced with chronic exposure, only a small percentage of dependent users progress to addiction.
Recent studies in rats suggest that impulsivity may be a crucial trait that represents a risk for
addiction. The transition to addiction is determined by a combination of environmental and genetic
factors. Heritability of addiction, as determined by comparing monozygotic with dizygotic twins, is
relatively modest for cannabinoids but very high for cocaine. It is of interest that the relative risk for
addiction (addiction liability) of a drug (Table 32–1) correlates with its heritability, suggesting that
the neurobiologic basis of addiction common to all drugs is what is being inherited. Further
genomic analysis indicates that only a few alleles (or perhaps even a single recessive allele) need
to function in combination to produce the phenotype. However, identification of the genes involved
remains elusive. Although some substance-specific candidate genes have been identified (eg,
alcohol dehydrogenase), future research will also focus on genes implicated in the neurobiologic
mechanisms common to all addictive drugs.
Current theories on the
neurobiology of addiction
Nonaddictive Drugs of Abuse
•
•
•
Some drugs of abuse do not lead to addiction. This is the case for substances that alter
perception without causing sensations of reward and euphoria, such as the hallucinogens and the
dissociative anesthetics (Table 32–1). Unlike addictive drugs, which primarily target the
mesolimbic dopamine system, these agents primarily target cortical and thalamic circuits. Lysergic
acid diethylamide (LSD), for example, activates the serotonin5-HT2A receptor in the prefrontal
cortex, enhancing glutamatergic transmission onto pyramidal neurons. These excitatory afferents
mainly come from the thalamus and carry sensory information of different modalities, which may
constitute a link to enhanced perception. Phencyclidine (PCP) and ketamine produce a feeling of
separation of mind and body (which is why they are called dissociative anesthetics) and, at higher
doses, stupor and coma. The principal mechanism of action is a use-dependent inhibition of
glutamate receptors of the N-methyl-D-aspartate (NMDA) type.
The classification of NMDA antagonists as nonaddictive drugs was based on early assessments,
which, in the case of PCP, have recently been questioned. In fact, animal research shows that
PCP can increase mesolimbic dopamine concentrations and has some reinforcing properties in
rodents. Concurrent effects on both thalamocortical and mesolimbic systems also exist for other
addictive drugs. Psychosis-like symptoms can be observed with cannabinoids, amphetamines,
and cocaine, which may reflect their effects on thalamocortical structures. For example,
cannabinoids, in addition to their documented effects on the mesolimbic dopamine system, also
enhance excitation in cortical circuits through presynaptic inhibition of GABA release.
Hallucinogens and NMDA antagonists, even if they do not produce dependence or addiction, can
still have long-term effects. Flashbacks of altered perception can occur years after LSD use.
Moreover, chronic use of PCP may lead to an irreversible schizophrenia-like psychosis.
~50% of those with substance abuse have mental health problems.
~30% of those with mental health disorder have a substance use
disorder (concurrent disorder).
- 50% of those with schizophrenia
- 25% of those with anxiety disorder
MODERATE DRINKING (WITHIN THE RECOMMENDED GUIDELINES OF U.S.
DEPARTMENT OF HEALTH AND HUMAN SERVICES)
Men: 2 or less/day
Women/Elderly: 1 or less/day
DRINKING PROBLEM (ABOVE THE RECOMMENDED GUIDELINES) ASSOCIATED
WITH:
Drinking to reduce depression or anxiety
Loss of interest in food
Drinking alone
Lying/hiding drinking habits
Injuring self or others while intoxicated
Drunk more than 3 or 4 times last year
Increasing tolerance
Withdrawal symptoms
Experiencing medical, social, or financial problems by drinking
ALCOHOL INTOXICATION
Coma:
•
60+ mmol/L (non-tolerant drinkers)
•
90-120 mmol/L (tolerant drinkers)
Legal limit for impaired driving: 17 mmol/L
A “Standard Drink”
Table wine (12%) – 5 oz. or 142 mL
Alcohol levels correlate poorly with intoxication
Regular beer (5%) – 12oz. or 341 mL
or
1 pint beer = 1.5 SD
1 bottle wine = 5 SD
26-er = 17 SD
40 oz. = 27 SD
ALCOHOL WITHDRAWAL
(Occurs within 12 to 48 hours after prolonged heavy drinking)
•
Stage 1 (onset 6-12hrs after last drink): tremor, sweating, agitation, anorexia, cramps,
diarrhea, sleep disturbance;
•
Stage 2 (onset 1-7 days): visual, auditory, olfactory, or tactile hallucinations;
•
Stage 3 (onset 12-72hrs and up to 7 days): seizures (grand mal, non-focal, brief);
•
Stage 4 (onset 3-5 days): delirium tremens, confusion, delusions, hallucinations,
agitation, tremors, autonomic hyperactivity (fever tachycardia, HTN);
Mortality rate 20% if untreated.
ALCOHOL WITHDRAWAL MANAGEMENT
Clinical Institute Withdrawal Assessment for Alcohol (CIWA-A)
scoring system (max score of 67);
•
mild <10
•
moderate 10-20
•
severe >20
Areas of Assessment
include:
Nausea/Vomiting
Tremor
Paroxysmal sweats
Anxiety
Agitation
Visual/tactile/auditory
disturbances
Headache
Disorientation
Treatment protocol using CIWA-A scale
Diazepam 20mg PO q1-2h prn until CIWA-A <10 points; Reassess 1-2 hrs after last dose;
•
If oral diazepam not tolerated: Diazepam 2-5mg IV/min – max 10-20mg q1h; or Lorazepam
SL;
•
If >65yrs, severe liver disease, severe asthma or respiratory failure: Lorazepam 1-4mg
PO/SL/IM q1-2h;
Thiamine 100mg IM then 100mg PO OD for 3 days;
Supportive care (hydration);
If hx of withdrawal seizures:
•
Diazepam 20mg PO q1h for min of 3 doses;
•
Dilantin (if hx of seizures or multiple withdrawal seizures);
If hallucinosis present:
•
Haloperidol 2-5mg IM/PO q1-4h – max 5 doses/day or atypical antipsychotics (olanzapine,
risperidone);
•
Diazepam 20mg times 3 doses (seizure prophylaxis – haloperidol lowers seizure threshold);
Admit if:
•
Still in withdrawal after >80mg of diazepam;
•
Delirium tremens ( severe confused state, fluctuating levels of consciousness, agitation,
insomnia, hallucinations/delusions, tremors, hyperpyrexia, diaphoresis), recurrent
arrhythmias, or multiple seizures;
WERNICKE-KORSAKOFF SYNDROME
Alcohol-induced amnestic disorders - d/t thiamine deficiency;
Necrotic lesions - mammillary bodies, thalamus, brainstem;
Wernicke’s encephalopathy (triad – nystagmus, ataxia, confusion): acute and reversible
•
Tx: Thiamine 100mg PO OD x 1-2wks;
Korsakoff ’s syndrome (anterograde amnesia, confabulations): chronic and only 20% reversible with
treatment
•
Cannot occur during an acute delirium or dementia;
•
Must persist beyond usual duration of withdrawal;
•
Tx: Thiamine 100mg PO bid/tid x 3-12mnths;
ALCOHOL DEPENDENCE MANAGEMENT
NON-PHARMACOLOGICAL:
•
Alcoholics Anonymous
•
Aversion therapy
•
Motivational interviewing, Psychotherapy
•
Other supportive measures (detox centers)
•
Meds important as adjunctive treatment: SSRIs, odansetron, topiramate;
PHARMACOLOGICAL:
•
Naltrexone (Revia): 50mg once daily.
Successful in reducing the “high” assoc with alcohol; mod effective in reducing cravings,
frequency or intensity of alcohol binges;
•
Disulfiram (Antabuse): Initially 100mg daily for 1-2 weeks; maintenance 200mg
daily. Maximum 300mg daily
Toxic rxn with alcohol consumption (flushing, sweating, nausea and vomiting,
palpitations, headache, dyspnoea, chest pain, hypotension, cardiovascular collapse,
convulsions, arrhythmias, death); If pt relapses, must wait 48 hrs before restarting
Antabuse;
(BLOW, C, COKE, CRACK, FLAKE, FREEBASE, ROCK, SNOW)
Alkaloid extracted from leaves of the coca plant; blocks presynaptic uptake of dopamine
(causing euphoria), norepinephrine and epinephrine (causing vasospasm, hypertension).
Self-administered by inhalation or intravenous use.
INTOXICATION
Elation
Euphoria
Pressured speech
Restlessness
Sympathetic stimulation (tachycardia, mydriasis, sweating)
Prolonged use may result in paranoia and psychosis;
OVERDOSE (MEDICAL EMERGENCY)
Hypertension
Tachycardia and ventricular arrythmias
Tonic-clonic seizure
Dyspnea
TREATMENT
IV Diazepam (to control seizures)
Propanolol or labetalol (to manage HTN and arrythmias)
WITHDRAWAL
Initial “crash” (1-48hrs):
• Increased sleep
• Increased appetiite;
Withdrawal (1-10 wks):
• Dysphoric mood plus fatique, irritability, vivid, unpleasant dreams
• Insomnia or hyperinsomnia
• Psychomotor agitation or retardation
COMPLICATIONS
Relapse suicide (significant increase in suicide during withdrawal period)
MANAGEMENT
Supportive management
CHRONIC ABUSE: TREATMENT
• Psychotherapy
• Group therapy
• Behaviour modifications useful in maintaining abstinence
• Studies of dopamine agonists to block cravings show inconsistent results
COMPLICATIONS
• Neurovascular: Arrythmias, MI, CVA, ruptured AA
• Neurologic: Seizures
• Psychiatric: Psychosis, Paronoia, Delirium, Suicidal ideation
MAJOR RISKS ASSOCIATED WITH THE USE OF CONTAMINATED NEEDLES:
HEPATITIS B
HEPATITIS C
BACTERIAL ENDOCARDITIS
HIV
ACUTE INTOXICATION
Direct effect on receptors in CNS results in:
TREATMENT
•
decreased level of consciousness ABC’s
•
decreased pain perception
•
sedation
•
decreased sex drive
0.4mg up to 2 mg IV for diagnosis
•
nausea/vomiting
(also used for life-threatening CNS
•
decreased GI motility (constipation,
and cardiac depression);
anorexia)
•
•
IV glucose
•
Naloxone hydrochloride (Narcan):
•
Intubation, mechanical ventilation
+/- naloxone drip until patient alert
respiratory depression
without naloxone (up to 48hrs with
TOXIC REACTION
long-acting opioids);
•
Shallow respiration
•
Miosis
•
Bradycardia
Longer half-life drugs – observe for at least 24hrs for
•
hypothermia
toxic reaction;
CAUTION
OPIOID WITHDRAWAL
ONSET: 6-12h;
DURATION: 5-10 days;
SYMPTOMS
•
Depression
•
Insomnia
•
Drug Craving
•
Myalgias
•
Nausea
•
Chills
•
Autonomic instability (lacrimation,
rhinorrhea, piloerection)
COMPLICATIONS
Loss of tolerance
(overdose on relapse)
•
Miscarriage
•
Premature labor
MANAGEMENT
•
Long-acting oral opiods:
Methadone, Buphrenorphine
•
Alpha-adrenergic agents:
Clonidine
CHRONIC ABUSE: TREATMENT
PSYCHOSOCIAL TREATMENT
• Narcotics Anonymous (emphasize total abstinence)
LONG-TERM TREATMENT
• Withdrawal maintenace treatment
•
Methadone (relieves drug cravings and withdrawal symptoms without
inducing sedation or euphoria);
•
Naltrexone or Naloxone (used to extinguish drug-seeking behaviour);
(WEED, HERB, CHRONIC, JAY, BUD, BLUNT, BOMB, DOOBIE, HYDRO, SINSEMILLA, HASH,
JOINT, POT, GRASS, REEFER, MARY JANE, GANJA, HOMEGROWN, DOPE, SPLIFF)
Marijuana, Hashish (hash) and hash oil come from cannabis sativa.
Psychoactive substance: delta-9-Tetrahydrocannabinol (THC)
Self-administration: smoking
MEDICAL USES:
Anorexia-cachexia (AIDS, Canacer)
Spasticity, muscle spasms (MS, spinal cord injury)
Levodopa-induced dyskinesia (Parkinson’s disease)
Controlling tics and obsessive-compulsive behaviour (Tourette’s syndrome)
Reducing intra-ocular pressure (Glaucoma
INTOXICATION
• Tachycardia
• Conjunctival vascular engorgement
• Dry mouth
• Increased appetite, sense of well-being
• Euphoria/laughter
• Muscle relaxation
• Impaired performance on psychomotor tasks (including driving)
High doses: Depersonalization, paranoia, anxiety
May trigger schizophrenia and psychosis in predisposed individuals;
CHRONIC USE
Associated with tolerance and an apathetic, amotivational state;
Cessation does not produce significant withdrawal phenomenon
DEPENDENCE: TREATMENT
Behavioural and psychological interventions to maintain an abstinent state.
(SPEED, BENNIES, GLASS, CRYSTAL, CRANK, PEP PILLS, AND UPPERS)
INTOXICATION
• Euphoria
• Improved concentration
• Sympathetic and behavioural hyperactivity
• At high dose: coma
WITHDRAWAL
• Dysphoria
• Fatique
• Restlessness
CHRONIC USE
Paranoid psychoisis (diagnostically similar to schizophrenia with agitaiton, paranoia, delusions,
and hallucinations);
TREATMENT: Antipsychotics
INTOXICATION
• Tachycardia
• Hypertension
• Mydriasis
• Tremor
• Hyperpyrexia
• Variety of perceptual and visual changes
• High doses: depersonalization, paranoia, and anxiety
NO SPECIFIC WITHDRAWAL SYNDROME;
TREATMENT OF AGITATION AND PSYCHOSIS:
• Support, reassurance, diminished stimulation
• Benzodiazepines
• High potency antipsychotics (seldom required)
Baxter, S. D. & McSheffrey, G.G. The Toronto Notes 2010. Toronto: University of Toronto, 2010.
Bertram G. Katzung, Susan B. Masters, Anthony J. Trevor: Basic & Clinical Pharmacology, 11e; Chapter 32
Hyman SE: Addiction: A disease of learning and memory. Am J Psychiatry 2005;162:1414
Kauer JA, Malenka RC: Synaptic plasticity and addiction. Nat Rev Neurosci 2007;8:844
http://www.nida.nih.gov/nidamed
http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.cfm
http://www.hbo.com/addiction
http://www.nlm.nih.gov/medlineplus/magazine/issues/spring07/articles/spring07pg14-17.htmlL